Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2644-1209
Case Report(ISSN: 2644-1209) 
Sequential Endogenous Endophthalmitis Volume 1 - Issue 2
Sid A Schechet* and Vinod Lakhanpal
- Eye Consultants of Maryland, University of Maryland Medical Center, USA
Received: January 30, 2018; Published: February 16, 2018
Corresponding author: Sid A Schechet, The University of Chicago, Department of Ophthalmology and Visual Sciences, 5758 S Maryland Avenue, Clinic 1B, Chicago, USA
DOI: 10.32474/TOOAJ.2018.01.000107
Abstract
This report describes an unusual case of culture-proven bilateral endogenous endophthalmitis secondary to an underlying psoas abscess in a 54 year old male. The patient first was found to have endophthalmitis in the left eye, and, in spite of being on the appropriate intravenous antibiotics, he subsequently developed endophthalmitis in the right eye two days later With timely treatment and close communication with the primary team, the patient recovered with a successful visual outcome.
Keywords: Endogenous endophthalmitis; Bilateral; Psoas abscess; Vitrectomy; Staph aureus
Abbreviation: EE: Endogenous Endophthalmitis; MSSA: Methicillin-Sensitive Staph Aureus; STEMI: ST-Elevation myocardial Infarction
Introduction
Endogenous endophthalmitis (EE) is a severe vision threatening disease that occurs as a result of hematogenous spread of bacteria or fungi into the eye from distant sites of the body. It is a rare cause of endophthalmitis causing less than 10% of all endophthalmitis cases [1]. EE presenting bilaterally has been reported in up to 33% of EE cases [2]. EE is associated with co morbidities such as diabetes mellitus, liver disease, cardiac disease, malignancy, immunosuppressant, in-dwelling catheters, and intravenous drug abuse [3-7]. The initial diagnosis is incorrect in up to 50% of cases, so a high level of suspicion for this disease is vital in order to perform prompt treatment that could preserve useful vision [5,8]. We describe a case of endophthalmitis presenting first in the left eye followed two days later in the right eye with the infectious source ultimately being found to be an occult psoas abscess.
Case Report
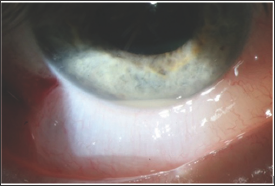
A 54 year-old Caucasian male with hypertension, diabetes mellitus, hyperlipidemia, and prostate cancer and no ocular history presented to the emergency room with dull abdominal pain. He was found to have an ST-elevation myocardial infarction (STEMI) and underwent urgent coronary stenting. The following day he was septic with Methicillin-sensitive staph aureus (MSSA) bacteremia and started on appropriate intravenous antibiotics. Urine cultures and echocardiogram were unremarkable. Two days later he developed blurry vision in the left eye with a visual acuity (VA) of 20/300, and he was found to have a hypopyon, anterior chamber inflammation, and vitreous membranes all while the right eye was unremarkable. He was diagnosed with endophthalmitis of the left eye and due to the rapid nature of the findings he underwent a pars planavitrectomy with intravitrealvancomycin and amikacin (Figure 1).
Figure 1: Hypopyon of the left eye.
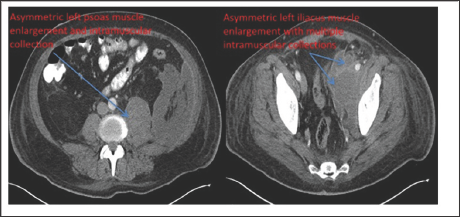
Two days later he complained of new blurry vision in the right eye and was found to have a hypopyon and vitreous inflammation on exam with a VA of 20/200. This eye was diagnosed with endophthalmitis and treated with vitreous tap and intravitrealvancomycin and amikacin. Both vitreous samples grew MSSA. We discussed with the primary team that further efforts should be done to find the source of the bilateral endogenous endophthalmitis. A transesophageal echocardiogram was unremarkable. The patient was still having persistent abdominal pain since presentation, which was initially attributed to the STEMI, so a CT-scan of the abdomen and pelvis was performed revealing a large left-sided psoas abscess which was drained with cultures being positive for MSSA (Figure 2).
Figure 2: Axial cut of computed-tomography imaging of the abdomen and pelvis revealing a large left-sided psoas abscess demonstrated by the blue arrows.
Discussion
Endogenous endophthalmitis (EE) is a devastating ocular disease. This case demonstrates that despite being on the appropriate intravenous antibiotics, patients can still develop endophthalmitis due to poor ocular penetration of the antibiotics. Older reports suggested intravenous antibiotics are the definitive treatment for EE while intravitreal antibiotics with/without vitrectomy make a limited contribution [9]. In the recent past, a more active approach is taken to manage EE with vitreous tap and inject and possible vitrectomy in addition to intravenous antibiotics [10,11]. In a review by Jackson, there was less of a trend for enucleations or eviscerations when patients received intravitreal antibiotics. Further, when vitrectomy was performed, there was a better visual acuity outcome and fewer rates of enucleations or eviscerations [5]. Connell found that with bacterial EE, vitrectomized eyes had better VA and none required enucleation when compared to non-vitrectomized where 50% required enucleation [4]. Treatment options should be weighed on a case-by-case basis, but one should be cognizant not to directly follow the guidelines of the Endophthalmitis Vitrectomy Study as the pathogenesis of EE is markedly different than for post-cataract extraction endophthalmitis [12].
In our case the bacterium isolated from eyes, blood, and abscess was MSSA. In terms of bacterial EE, studies do vary, but generally in western nations there is a predominance of grampositive bacteria, while in Asian countries the cause is mostly gram-negative [1,3]. Interestingly, with Methicillin-resistant Staph Aureus EE that is unresponsive to vancomycin, there are recent reports about the effectiveness of intravitreal and intravenous daptomycin, which crosses the blood-ocular barrier [5,11,13]. This patient had risk factors predisposing him to EE such as diabetes mellitus, hypertension, and a history of malignancy. Many studies have shown these to be risk factors for EE with other risk factors including: intravenous drug use, HIV infection, liver disease, chronic obstructive pulmonary disease, end-stage renal disease, immunosuppressant, indwelling catheters, hypertension, and more [14,15]. When evaluating a patient with the aforementioned risk factors, one should be cognizant of the warning signs and consider endophthalmitis in the differential; however, there have been reports of healthy individuals with no risk factors who developed EE [16]. In conclusion, to the author's knowledge, this is the fourth documented case of endogenous endophthalmitis secondary to a psoas abscess. Further, this is a unique case of EE in that one eye presented days after the first even while being treated with the appropriate intravenous antibiotics, but this serves as a lesson that EE can still occur in that situation. A more aggressive approach was taken to treat the first eye with vitrectomy, and since the bacteria was known at the time of the second eye's presentation, it was decided to treat more conservatively with tap & inject. With rapid diagnosis and proactive treatment, this case resulted in a successful visual outcome for the patient. Early recognition of EE with aggressive management of vitreous tap and antibiotic injection with or without vitrectomy- in addition to systemic antibiotics- should be considered to ensure a successful visual outcome. Close follow up and communication with the primary team is also vital in terms of locating and treating the underlying pathology.
References
- Okada AA, Johnson RP, Damico DJ, Baker AS (1994) Endogenous bacterial endophthalmitis: A ten year retrospective study. Ophthalmology 101(5): 832-838.
- Vaziri K, Schwartz SG, Kishor K, Flynn HW (2015) Endophthalmitis: state of the art. Clinical Ophthalmology 9: 95-108.
- Chung KS, Kim YK, Song YG, Kim CO, Han SH, et al. (2011) Clinical review of endogenous endophthalmitis in Korea: a 14-year review of culture positive cases of two large hospitals. Yonsei Med J 52(4): 630-634.
- Connell PP, EC Oneill, D Fabinyi, FMA Islam, R Buttery, et al. (2011) Endogenous endophthalmitis: 10-year experience at a tertiary referral centre. Eye (Lond) 25(1): 66-72.
- Jackson TL, Paraskevopoulos T, Georgalas I (2014) Systematic review of 342 cases of endogenous bacterial endophthalmitis. Surv Ophthalmol 59(6): 627-635.
- Zhang H, Liu Z (2010) Endogenous endophthalmitis: a 10-year review of culture-positive cases in northern China. OculImmunolInflamm 18(2): 133-138.
- Lim HW, Shin JW, Cho HY, Kim HK, Kang SW, et al. (2014) Endogenous endophthalmitis in the Korean population: a six-year retrospective study. Retina 34(3): 592-602.
- Jackson TL, Paraskevopoulos T, Georgalas I (2014) Systematic review of 342 cases of endogenous bacterial endophthalmitis. Surv Ophthalmol 59(6): 627-635.
- Greenwald MJ, Wohl LG, Sell CH (1986) Metastatic bacterial endophthalmitis: A contemporary reappraisal. Surv Ophthalmol 31(2): 81-101.
- Christensen SR, Hansen AB, La cour M, Fledelius HC (2004) Bilateral endogenous bacterial endophthalmitis: a report of four cases. Acta Ophthalmol Scand 82(3 Pt 1): 306-310.
- Schiedler V, Scott IU, Flynn HW, Davis JL, Benz MS, et al. (2004) Culture- proven endogenous endophthalmitis: clinical features and visual acuity outcomes. Am J Ophthalmol 137(4):725-731.
- (1995) Results of the Endophthalmitis Vitrectomy Study: A Randomized Trial of Immediate Vitrectomy and of Intravenous Antibiotics for the Treatment of Postoperative Bacterial Endophthalmitis. Arch Ophthalmol 113(12): 1479-1496.
- Buzzacco DM, Carroll C (2012) Intravitreal Daptomycin in a Case of Bilateral Endogenous Endophthalmitis. Arch Ophthalmol 130(7): 940941.
- Sheridan KR, Potoski BA, Shields RK, Nau GJ (2010) Presence of adequate intravitreal concentrations of daptomycin after systemic intravenous administration in a patient with endogenous endophthalmitis. Pharmacotherapy 30(12): 1247-1251.
- Leibovitch I, Lai T, Raymond G, Zadeh R, Nathan F, Selva D (2005) Endogenous endophthalmitis: a 13-year review at a tertiary hospital in South Australia. Scand J Infect Dis 37(3): 184-189.
- Shankar K, Gyanendra L, Hari S, Narayan SD (2009) Culture proven endogenous bacterial endophthalmitis in apparently healthy individuals. OculImmunolInflamm 17(6): 396-399.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...