Lupine Publishers Group
Lupine Publishers
Research Article(ISSN: 2644-1209) 
Presentatıon of a Temporal Artery Case with One Eye Volume 1 - Issue 5
Mehmet Tayfur1, Gamze MADEN1*, Şeyma Gülcenur ÖZTURAN1, Dilan YILDIZ1, Burak ERDEN1, Mehmet Egemen KARATAŞ2 and Mustafa Nuri ELÇİOĞLU1
- 1Department of Ophthalmology, Okmeydani Training and Research Hospital, Turkey
- 2Department of Ophthalmology, SisliHamidiyeEtfal Training and Research Hospital, Turkey
Received: September 25, 2018; Published: October 01, 2018
*Corresponding author: Department of Ophthalmology, Okmeydani Training and Research Hospital, Turkey
DOI: 10.32474/TOOAJ.2018.01.000124
Abstract
Temporal arteritis or giant cell arteritis(GCA), is a frequently seen systemic inflammatory vasculitis, affecting elderly people. Early treatment is very important to reduce the risk of future vision loss. In this report, we presented arteritic anterior ischemic optic neuropathy (AAION) in a late-diagnosed temporal arteritis. Interestingly, despite late diagnosis prompt improvement was seen and total blindness, the most worrisome complication of temporal arteritis, was prevented with urgent treatment. In this case report, we presented urgent treatment of the patient with AAION who is blind in one eye due to complicated cataract surgery. We reported the importance of prompt treatment and approach to patients who has already diagnosed with temporal arteritis.
Introduction
GCA is a vasculitis that affects the vessels in the middle and large wings. The incidence increases with age and is approximately 70.1 per 100,000 person over 80 years [1]. Temporal arteritis is a systemic vasculitis that can cause risk of serious death due to focal ischemic occlusions in the cranial arteries [2]. The most serious forms of eye involvements are inflammatory anterior ischemic optic neuropathy (AION), and central retinal artery occlusion (CRAO) [3,4]. AION is seen in %75 of GCA patients and CRAO is seen %15 of them. Arteritic anterior ischemic optic neuropathy (AAION) is an acute, often painful optic neuropathy that occurs predominantly in elderly patients over age 50. The incidence increases with decades and it can cause permanent loss of vision [5]. Ischemia occurs at the head of the optic nerve in relation with structural crowding of the nerve fibers, impairing perfusion and leading to optic disc edema [6]. Genetic can be one of the factor of the etiology of the GCA, as an evidence it is more common in Caucasians. Although it has been reported in many different races and ethnicities [5].
Case Presentation
A 67-year-old female patient was admitted to the emergency room with complaints of headache and decreased vision in the left eye for 3 days. Known history of hypertension and bilateral cataract surgery 2 years ago. Analgesic and anti-depressant medicines were prescribed in addition to other medications containing vitamin B12, iron preparation, gabapentin, thiocolchicoside as the end-effector. The visual acuity at the arrival of the patient is hand motion in the right eye and 0,05 (snellen equivalent ) in the left eye, without increases with correction. In the anterior segment examination, the right eye was probable, followed by complicated cataract surgery, corneal decompensation with intraoculer lenses (iol) reflex, the left eye’s iol was centralized and the anterior segment was calm. Although there was no sight in the right fundus examination, there was papiledema and flame hemorrhages located adjacent to the disc in the left fundi. After examination the anamnesis was questioned. Patient had headache and tenderness of the temporal arteries, jaw claudication, malaise, loss of appetite, anorexia and weight loss, joint and muscle pain. Serum C reactive protein (CRP) and platelets(PLT) elevations were detected in patients requiring urgent laboratory tests. AION associated with GCA was diagnosed and admitted to the eye service. The patient was treated with systemic steroid therapy ( pulse 1 gr/day methylprednisolone).
Results
Laboratory results of our patient before treatment:
a) CRP : 193.7mg/L (referance range: 0-5 ).
b) PLT : 757.000mm^3 (150.000-400.000).
c) HGB: 10.8g/dL (11.5-15.5) , MCV:83.1 fL(80-95).
d) HCT: %32.9 (35.5-48).
e) MCHC : 32.8g/dL(31-37).
f) RDW:% 15.1(11.2-15).
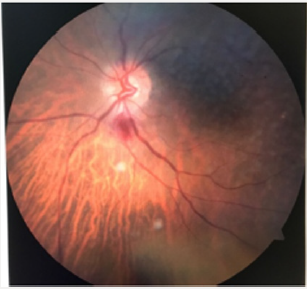
Erythrocyte sedimentation rate (ESR) could not be studied under emergency conditions. High CRP and thrombocytosis and chronic disease anemia supported the diagnosis. Systemic steroid treatment was begun immediately.After 3 days of treatment the patient visual acuity was not increased but optic disc edema reduced (Figure 1). On the other hand, there was a decreases in all systemic symptoms of temporal arteritis.
Laboratory results on the 3rd day of treatment:
a) CRP: 86.2mg/L .
b) ESR: 92mm/h.
c) PLT: 740.000mm^3.
d) HGB: 10.1g/dL.
e) Ferritin: 442ng/mL( 13-150).
The patient was consulted to the rheumatology department. Rheumatologist confirmed that patient was clinically compatible with the temporal arteritis and ordered a biopsy for definitive diagnosis. Positive biopsy findings for GCA (giant cell chronic inflammatory infiltrate) were confirmed. After iv treatment, the patient was discharged with oral steroids and rheumatology and eye polyclinic controls were given. At the 1st month control of the patient, it was observed that ESR, CRP, PLT decreased to the normal limits and chronic anemia was improved.However, the vision was noted as 0.05 (snellen chart) in the first hospitalization.In the fundus examination, optic disc edema was replaced by a slight pallor.
Laboratory results on the first month of treatment:
a) CRP:16.1mg/dL
b) ESR: 12mm/h
c) PLT: 287.000mm^3
d) HGB: 12.7g/dL
Discussion
GCA typically present with headache (most common) and tenderness of the temporal arteries or scalp, jaw claudication (symptom most specific for the disorder), malaise, loss of appetite, anorexia and weight loss, fever, joint and muscle pain, and ear pain. Symptoms related to systemic inflammation systemic symptoms may be considered as age related pain and that can cause mis or late diagnosis. Also symptomatic treatments like myorelaxan, analgesic, gabapentin analogues may delay the diagnosis while reducing the pain. So unfortunately irreversible complications can seen. GCA has serious systemic complications such as temporal arteritis, life-threatening heart attack, paralysis and ocular complications such as double vision and visual loss, they are also important morbidity in advanced age [4,7]. The most commonly reported ocular complications are AAION and choroidal ischemia [3,4]. Choroidal ischemia may be associated with the optic neuropathy and produces peripapillary pallor and edema deep to the retina. Ocular manifestations include rapid onset of unilateral visual loss accompanied by decreased visual acuity (typically severe: <20/200 in over 60% of the patients), visual field (altitudinal field defect is most common) or both. A relative afferent pupillary abnormality is common in unilateral or asymmetric optic neuropathies [8]. A chalky-white pallor with optic disc edema, which may be severe, is the hallmark of AAION, but it is not uncommon to see hyperemic swelling that may be indistinguishable ophthalmoscopically from NAION [5]. Oftentimes the disc’s swelling is diffuse, but flame hemorrhages which is located adjacent to the disc, and thinning in the peripapillary retinal arterioles can be seen.
An elevated ESR (up to 70-120mm/min) and/or CRP can support the diagnosis. These tests have 97% specificity for temporal arteritis wih AAION. Patients with NA-AION do not have these types of abnormalities [5]. Other tests in GCA include: platelet count for possible thrombocytosis, leukocyte count, and hemoglobin levels. Platelet count is often elevated acutely in cases of AAION and can be used in conjunction with elevated ESR and CRP levels to make a preliminary diagnosis. In our patient who was treated with B12 vitamins and iron preparation due to mis-diagnosis although she had chronic anemia. Confirmation of the diagnosis of temporal arteritis by superficial temporal artery biopsy is recommended in cases of AION with clinical suspicion of arteritis. Positive biopsy findings (intimal thickening, internal limiting lamina fragmentation, and chronic inflammatory infiltrate with giant cells) is confirmatory for GCA. A negative biopsy does not rule out GCA because of skip lesions (both discontinuous arterial involvement) and solely contralateral temporal artery inflammation. They can cause falsenegative results (with a 3-5% false-negative error rate). If the GCA’s risk high and the initial biopsy is found to negative, a biopsy of the contralateral temporal artery should be considered. Early steroid treatment is essential. High dose systemic corticosteroids are standard [5]. Intravenous (IV) methylprednisolone, 1g/day, for the first three days has been recommended for severe cases but there is no study to compare oral and IV steroid treatments in patients with GCA. The patients should be treated with oral prednisone 60-100mg/day after intravenous pulse therapy. High dose oral treatment continue for a several months, even it may continue for several years in severe cases to avoid permanent vision loss [5]. In AAION, there is usually no increase in visual acuity after treatment, but the risk of AAION in the other eye is 50%. In our case, the patient had already blind in one eye so we can emphasize that early diagnosis was the most important factor in patients with GCA.
Conclusion
When the AAION due to temporal arteritis is suspected, treatment should be start immediately. A systematic and detailed anamnesis are essentials for the diagnosis of temporal arteritis, which has serious systemic and ocular complications (permanent blindness-total blindness). The treatment only for the symptoms without diagnosis can causes delay in diagnosis and increases mortality & morbidity rates.
References
- Belenguer Benavides A, Vilar Cambies C, Geffner Sclarsky D (2004) Stroke as the first manifestation of temporal arteritis: Three case reports and a review of its pathogenesis and treatment. Rev Neurol 39(3): 227- 232.
- Zborowska B, Ell J, McGhee Collett M, Scholyer R, McCluskey PJ (2004) Progressive visual loss in a patient with presumed temporal arteritis despite treatment: How to make the diagnosis. Clin Experiment Ophthalmol 32(3): 335-336.
- Esgin Haluk, Bülbül Ebru Demet (2005) Dev hücreli arterite bağlı kısa aralıkl bilateral santral retinal arter tıkanıklığı Retina Vitreus 13: 319- 321.
- Liu GT, Glaser JS, Schatz NJ, Smith JL (1994) Visual Morbidity in giant cell arteritis. Clinical characteristics and prognosis for vision. Ophtalmology 101(11): 1779-1785.
- Sohan Singh Hayreh (2009) Ischemic optic neuropathy. Prog Retin Eye Res 28(1) 34-62.
- Anthony C Arnold (2001) Ischemic optic neuropathies. Ophthalmol Clin North Am 14(1): 83-98.
- Keltner JL (1982) Giant cell arteritis. Signs and symptoms. Ophthalmology 89: 1101-1110.
- Beck RW, Servais GE, Hayreh SS (1987) Anterior ischemic optic neuropathy. IX. Cup-to-disc ratio and its role in pathogenesis. Ophthalmology 94(11): 1503-1508.