Lupine Publishers Group
Lupine Publishers
Research ArticleOpen Access
Ophthalmology During COVID-19: A Snapshot of Clinical Practice in the United States Running head: Ophthalmology Practices During COVID-19 Volume 3 - Issue 3
Erin Jennings, Douglas Brown, Jonathan Lam* and Yi Zhang
- Department of Ophthalmology, Temple University-Lewis Katz School of Medicine, USA
Received:November 03, 2021; Published:November 16, 2021
Corresponding author: Jonathan Lam, Department of Ophthalmology, Temple University-Lewis Katz School of Medicine, Philadelphia, PA, USA
DOI: 10.32474/TOOAJ.2021.03.000163
Introduction
Virus and Transmission
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is a human Coronavirus first reported in December of 2019 in Wuhan, China after 41 cases of unexplained pneumonia were identified in the region [1]. On January 7, 2020, the World Health Organization (WHO) officially identified the pathogen as a novel human coronavirus via throat and nasopharyngeal swab, and on March 11, 2020 the WHO declared the outbreak as a pandemic associated with substantial morbidity and mortality [2]. SARS-CoV-2 belongs genetically to the Coronaviridae family, a group of viruses typically known to cause mild upper respiratory infections and gastrointestinal symptoms in patients, and is often transmitted through direct contact, or through respiratory droplet transmissions. [3,4] Of particular concern to ophthalmologists, the novel virus has been found in the conjunctival secretions of SARS-CoV-2 positive patients presenting with conjunctivitis, providing an additional infection source, likely from direct inoculation via infected droplets or through connection with the nasolacrimal system [1,5]. While the vast majority of SARS-CoV-2 positive patients present with respiratory or gastrointestinal symptoms, early research from China suggested the presence of ocular signs and symptoms, including conjunctivitis and increased secretions [6]. Furthermore, patients with ocular manifestations were more likely to have severe systemic manifestations [5,7]. With increasing levels of uncertainty around COVID-19 disease transmission, immunologic response, and reliability around viral testing, official recommendations and guidelines for medical practice in ophthalmology were issued by the WHO, Federal Drug Administration (FDA), American Academy of Ophthalmology (AAO), and various researchers worldwide who had been researching the disease since its outbreak. With rapidly changing recommendations, in addition to a dearth of national standardization of medical COVID-19 guidelines, hospital and private practice administrators had to overhaul existing operational guidelines in order to prevent disease spread between both patients and health care workers alike. Organizations have differed in their approach based on infection risk in the region, financial implications, and their workforce’s ability to implement changes. Beginning in April 2020 Ophthalmologists at Temple University Hospital, in Philadelphia, Pennsylvania, a region at the height of the pandemic, sought to evaluate Ophthalmology practices’ implementation of Coronavirus guidelines across the nation. The aim of the current study was to assess and quantify how ophthalmologists early in the COVID-19 pandemic adapted and altered their clinical practice between April 22, 2020, to July 25, 2020.
Materials and Methods
The COVID-19 in Ophthalmology survey is a population based, cross-sectional study of ophthalmologists across the United States. Participants were identified on April 21, 2020, using the “Find an Ophthalmologist” feature on the American Academy of Ophthalmology’s website, which allowed for random retrieval of contact information across the 50 states. This form ensured a random sampling of participants by state and general demographics. The survey was distributed via email contact and responses were collected between April 2020 and July 2020. We sent out a total of 2,299 emails and received 147 responses (response rate of 6%). Results were compiled and analyzed conducting using the Google Survey Tool.
Results
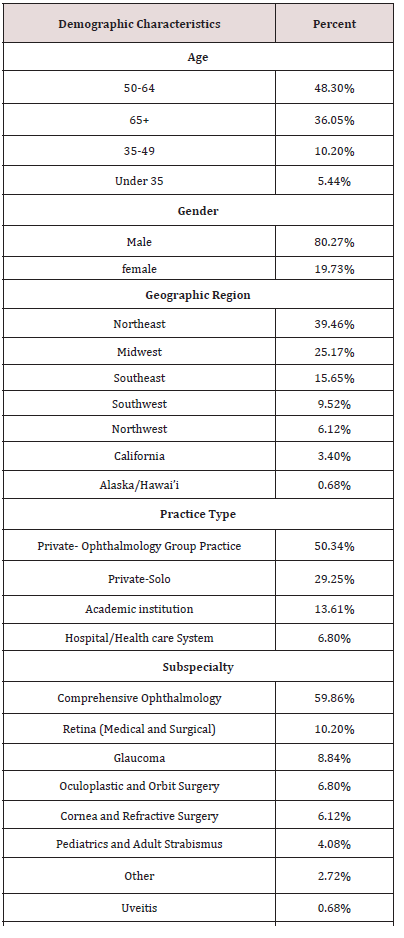
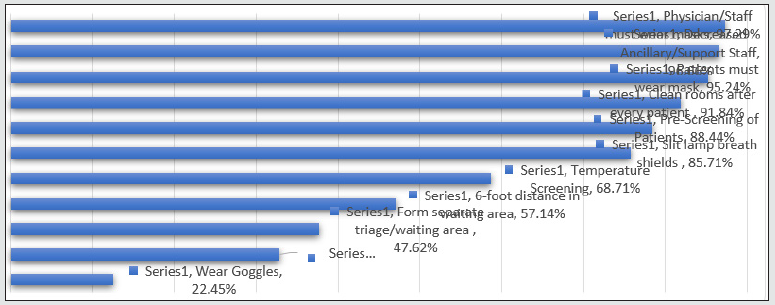
Given the high transmissibility of SARS-CoV-2, ophthalmologists were forced to alter their clinical practice. This was accomplished primarily through changes to clinical personnel, limiting the number and type of patients seen, screening protocols, and adhering to up-to-date sanitization guidelines. The survey respondents were distributed amongst all major geographic regions of the United States; Northeast 39.7%, Southeast 15.8%, Southwest 9.6%, Midwest 24.7%, Northwest 6.2%, California 3.4%, and Alaska/Hawaii 0.7%. The majority of respondents were male (80.1%) and practiced comprehensive ophthalmology (60.3%). In terms of age, the most frequent of survey respondents was 50-65 years (48.6%), closely followed by the over 65 age range (36.6%). Only 10.3% of respondents were 34-49 years of age with less than 5.5% of respondents being under 35 years of age. Most respondents were in a private, group practice (50.7%) or a private, solo practice (29.5%). Less than 13% of respondents primarily worked in an academic setting while only 6.8% primarily worked in a hospital/healthcare system (Table 1). On March 18, 2020, the AOA released an email to members mandating they cease all in-office visits and surgeries unless urgent or emergent to help minimize the number of patients entering the clinic [8]. This aimed to stratify and limit the number of people exposed in clinic while conserving personal protective equipment (PPE) and resources for healthcare professionals. On March 27, 2020, the AAO, in coordination with several ophthalmology subspecialty societies, released a list of urgent and emergent procedures routinely done in operating rooms and ambulatory surgical centers [9]. This list included many ophthalmic procedures performed in the case of trauma and sight threatening infections. Based on our survey, adhering to these recommendations resulted in a large decrease in patient volume across ophthalmology clinics with nearly half of practices (41.8%) seeing less than 25% of their usual patient volume. Only 20.5% of ophthalmology practices were seeing 26-50% of their patients, 12.3% of practices were seeing 51-75% of patients and 11.6% of practices were still seeing 76-100% of their patients. Notably, 13.7% of ophthalmology practices were seeing no patients at all (0%). Upon further review 55% of respondents who were not seeing patients were in solo private practice with 66.7% of respondents identifying as age 65 years or older. This follows national patient volume trends during a similar period. During the beginning of the pandemic in March 2020, there was a 54% average decrease in the amount of patients accessing care with ophthalmology experiencing a greater decrease in patient volume than any other specialty (81% patient volume decrease) according to an analysis by Strata Decision technology [10]. Similarly, ophthalmologic procedures experienced the highest reduction in patient volume with a 97% decrease in cataract surgery and an 88% decrease in glaucoma procedures over a two-week period from March 22-April 4, 2020, compared to the year prior; other high hit areas were sleep apnea procedures (91% decrease) and osteoarthritis procedures (88% decrease) [10]. At the time of our study, there was an 8.6% percent increase in ophthalmology patient visits at the start of May 2020 compared to the weeks prior in April [11]. When patients were seen, ophthalmologists employed a variety of measures to protect themselves and their patients (Figure 1).
Figure 2: Personal protective equipment considered appropriate by survey respondents when performing short and long cases (>1 hour in duration) for low-risk procedures (non-endoscopic, SARS-CoV-2 negative) and high-risk procedures (endoscopic, SARS-CoV-2 positive).
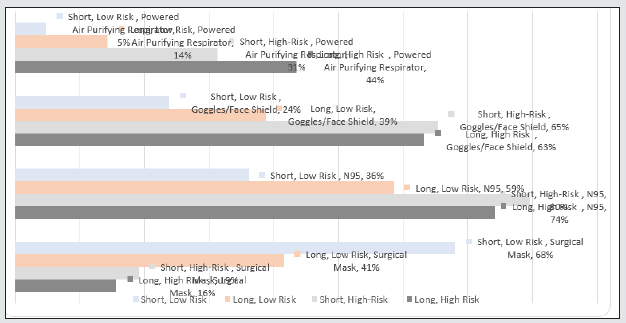
The majority of ophthalmologists surveyed had begun implementing virtual visits at the time of the survey, with 61% of practices using telemedicine; of the ophthalmologists who had not been using telemedicine, 47.1% indicated that they planned on using it at a later date. Portney et al. examined telehealth visits in the state of Michigan. Telehealth visits comprised 0.04% of all ophthalmology visits between September 2019 to March 2020. The amount of telehealth visits peaked at 17.0% during April 5th, 2020, to April 11th, 2020, which correlates with the state Stay-at- Home order on March 24th, 2020 [12]. In the subsequent months of March 2020 to September 2020, telehealth visits comprised 1.6% of all ophthalmology in the state of Michigan. Thus, demonstrating the increase and subsequent decrease in use of telehealth in ophthalmology. The study showed that by September 2020, 37.4% of ophthalmologists had used telehealth which differs from our survey which has 61% of ophthalmologists claiming to have used telehealth by April 2020. [12] of patients seen in office, 89% of respondents stated that they were following the proposed AAO guidelines or other criteria set to screen patients. Routine preoperative testing for SARS-CoV-2 remains controversial, and precautions with personal protective equipment should suffice [13]. This study emphasizes the lack of consensus, as 48.2% of respondents stated 75-100% of patients undergoing surgery were receiving preoperative testing with 40.1% of practices performing no routine preoperative testing. Upon further examination of the respondents, those who were not performing preoperative testing were predominantly either group private practices (67.3%) or solo private practices (27.3%). In the instance of a positive test result, elective procedures may be delayed for six weeks to decrease unnecessary risk of exposure. In terms of elective surgery, only 42.9% of respondents were still performing these procedures over the survey time frame. We asked survey respondents what personal protective equipment they considered most appropriate in a variety of surgical cases. We defined “short” cases as occurring in less than one (1) hour with “long” cases exceeding this limit. We defined the procedure as “low-risk” when the patient either had a negative SARS-CoV-2 preoperative test or there was no endoscopy or intubation required. Thus, “high-risk” cases involved either a SARS-CoV-2 positive patient, endoscopy, or intubation. Figure 2 outlines what personal protective equipment survey respondents consider to be appropriate when performing various levels of cases (short, low risk; long, low risk; short, high risk, and long, high risk). It is important to note that respondents were able to choose multiple pieces of personal protective equipment that they felt best protected them during procedures of varying risk. These findings portray the individual differences in perceived personal protective equipment needed to limit exposure to the coronavirus. Thus, the phrase “adequate PPE” is not uniformly defined across respondents.
Discussion
The main limitation of this study includes a low survey response rate resulting in a small study sample size. However, our survey respondents cover all major geographic locations, practice types, and subspecialties, and age ranges. This wide distribution strengthens our study as representative snapshot of ophthalmology practices during our survey timeframe. With wide-spread changes to ophthalmology practices throughout the COVID-19 pandemic, there has been a significant financial impact on the specialty at large. Many ophthalmologists practice outside of healthcare systems within small or solo private based practices and are dependent on elective procedures and maintenance of clinic visits. Thus, the interruption clinic volume had a devastating financial impact within the specialty. Reports from early in the pandemic in the United States showed ophthalmology had the largest decrease in patient visits of all medical specialties, with an estimated 80% initial decline in patient visits [11]. As of July 2020, one third of Ophthalmology practices were reporting clinical patient volumes between 26-50% of pre-COVID-19 levels and surgical interventions were yet to start apart from emergent cases [14]. Similar results were reflected in our survey over the same time period. As of December 2020, there was a reported 18% decrease in cumulative visits compared to the baseline pre-pandemic week of March 1-7. When compared to other medical specialties, this cumulative decline in visits puts Ophthalmology among those specialties most impacted by the pandemic [10,15]. The decrease in clinic and operative volume by ophthalmology practices has amounted to an approximately $60.1 billion loss of revenue per month for hospitals nationwide, and has necessitated an estimated 87% of ophthalmologic practices to apply for federal aid funding through the Medicare Provider Relief Fund and the Paycheck Protection Program,10,11 Despite recent surveys showing encouraging trends, ophthalmology practices have suffered a significant financial impact from the effects of the virus, and financial recovery will continue to be a challenge as practices grapple with slowly returning to pre-pandemic patient volumes.
COVID-19 fundamentally altered the clinical landscape and the ophthalmic field at large. Ophthalmologists demonstrated great flexibility and ingenuity as practices around the country quickly adapted to the “new normal” required by the pandemic. In addition to changes in clinic flow to maintain physical distancing, hygiene, and universal precautions, ophthalmologists quickly applied new models of virtual care [12]. These included digital health solutions such as telehealth, artificial intelligence decision support for triaging and clinical care, and home monitoring of visual acuity. These digital models allow for a cost-effective option to keep up with the increasing global burden of eye disease, especially following the lock-down period of the pandemic [12]. While the pandemic severely impacted Ophthalmology practices financially, we must note that office and surgical suite closures assuredly effected visual outcomes among patients. These cumulative visual effects and delays to ophthalmic care due to the pandemic are still widely unknown, and these are pivotal questions that should be considered in future studies as this information will impact the Ophthalmology field, our patients, and society as a whole. In summary, unpredictable viral trends and associated significant financial burden further emphasize the importance of continual monitoring and adherence to established guidelines, and continual analysis and reexamination of the way ophthalmologists practice within the changing environment. Further studies should continue to examine the impact of the ongoing COVID-19 pandemic and the continual adaptations by the field of ophthalmology.
References
- Xia J, Tong J, Liu M, Shen Y, Guo D (2020) Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS‐CoV‐2 infection. J Med Virol 92(6): 589-594.
- World Health Organization (WHO) (2020) Novel coronavirus (2019‐nCoV) situation report. World Health Organization, Geneva, Switzerland.
- Ivan Seah, Rupesh Agrawal (2020) Can the Coronavirus Disease 2019 (COVID-19) Affect the Eyes? A Review of Coronaviruses and Ocular Implications in Humans and Animals. Ocul Immunol Inflamm p. 1-5.
- Centers for Disease Control and Prevention. How COVID-19 Spreads.
- Amesty MA, Alió Del Barrio JL, Alió JL (2020) COVID-19 Disease and Ophthalmology: An Update. Ophthalmol Ther 9(3): 1-12.
- Wu P, Duan F, Luo C (2020) Characteristics of Ocular Findings of Patients with Coronavirus Disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol 138(5): 575-578
- Chen L, Deng C, Chen X, Zhang X (2019) Ocular manifestations and clinical characteristics of 534 cases of COVID-19 in China: A cross-sectional study. Med Rxiv.
- (2020) Important coronavirus updates for ophthalmologists. American Academy of Ophthalmology.
- (2020) American Academy of Ophthalmology. List of urgent and emergent ophthalmic procedures.
- (2020) The national and procedure volume tracker. Strata decision technology.
- Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler D (2020) The Impact of the COVID-19 Pandemic on Outpatient Visits: A Rebound Emerges. The Commonwealth Fund.
- Portney DS, Zhu Z, Chen EM, Steppe E, Chilakamarri P, et al. (2021) COVID-19 and Utilization of Teleophthalmology: Trends and Diagnoses (CUT Group). Ophthalmology.
- American Academy of Ophthalmology. Special considerations for ophthalmic surgery during the COVID-19 pandemic.
- EM Parikh R (2020) COVID-19 and Ophthalmology: The Pandemic’s Impact on Private Practices. Eyenet Magazine, American Academy of Ophthalmology.
- Ateey Mehrotra (2021) The Impact of COVID-19 on Outpatient Visits in 2020: Visits Remained Stable, Despite a Late Surge in Cases. The commonwealth Fund.