Lupine Publishers Group
Lupine Publishers
Research ArticleOpen Access
Neuro-Bechet Syndrome: A Case Study in Messina Volume 2 - Issue 5
Felicia M Ferreri*
- University of Messina, Biomorf Department, Italy
Received:March 14, 2023; Published:March 31, 2023
Corresponding author: Felicia M Ferreri, University of Messina, Biomorf Department, Italy
DOI: 10.32474/TOOAJ.2023.03.000178
Introduction
Behçet’s syndrome (hereafter shortened as BS or NBS) is a rare and chronic autoimmune disorder that frequently generates inflammation in several human organs, including the eyes [1-3]. The Turkish dermatologist Hulusi Behçet first described the disease in 1937 [1,2]. Behçet’s syndrome can affect people of all ages and ethnicities, but it frequently occurs in individuals of Middle Eastern and Asian descent.
The symptoms of NBS vary widely from person to person and it can affect different parts of the nervous system, including the brain, spinal cord, and peripheral nerves. Some common symptoms may include headaches, memory loss, confusion, difficulty speaking or understanding speech, weakness or numbness in the limbs, and visual disturbances such as double vision or blindness [4-6].
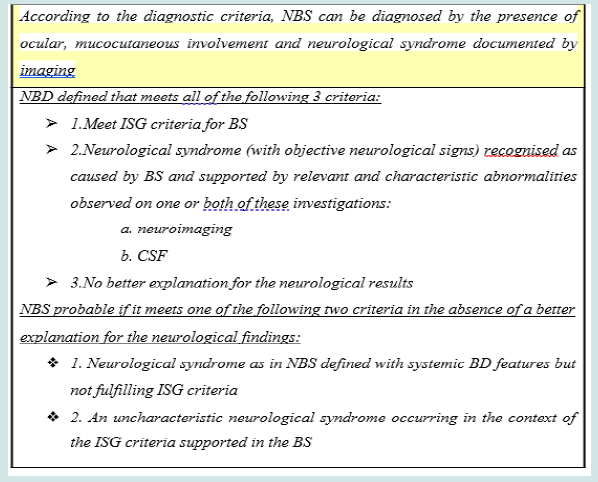
The NBS diagnosis is often challenging, since the associated symptoms frequently occur in other neurological disorders. A number of clinical trials, such as a neurological examination, imaging studies of the brain and spinal cord, and blood tests to look for signs of inflammation or autoimmunity are today available as a diagnostic tool. The treatment of NBS typically involves a combination of medications to both control the inflammation and manage the symptoms, with the goal of maintaining an acceptable quality of life in patients. The most popular treatments are corticosteroids, immunosuppressive drugs, and pain medications. In some cases, physical therapy is also recommended.
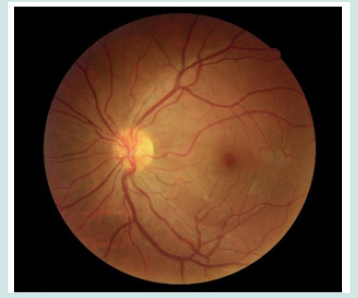
Eye disorders are a common complication of NBS, with up to 70% of patients experiencing some form of ocular involvement during the course of their disease. The most common eye manifestation of NBS is uveitis; other eye disorders associated with NBS include retinal vasculitis, conjunctivitis, episcleritis, and scleritis [1-7]. The severity of eye involvement in NBS can vary widely, ranging from mild and self-limited to severe and vision-threatening. Prompt diagnosis and treatment are essential to prevent permanent visual impairment. The aim of our study was to show that although it is a rare condition, NBS should be considered when there is an overt picture of NBS, especially in young subjects with neurological manifestations. As we claimed before, neurological onset is rare or difficult to interpret diagnostically. In such scenarios, the ophthalmologist has a fundamental role in the clinical- diagnostic interpretation and in the differential diagnostic pathway, in the search for even the slightest signs that can lead the clinical picture back to Behçet’s disease. In what follows we describe a significant case report in our hospital, Policlinico Universitario “G. Martino” of Messina, Italy.
Case Report
Patient: P. D. ♂ 31 years old
Clinical presentation: Acute onset of gravitational headache and right hemiparesis. Remote pathological history also shows: recurrent oral aphthroid ulcers in the last four months (please see Figure 1), arthalgias/myalgias, visual impairment.
Materials and Methods
The patient is admitted to neurology and undergoes a series of investigations. Neurological examination: horizontal nystagmus, right facio-brachio-crural hemiparesis and positive Hoffman and Babinski signs, bilateral. Blood chemistry tests: ESR 49 (standard range 0-15), CRP 1.70 (standard range <0.5), fibrinogen 537 mg/ dl (standard range 200-400) MRI: T2-weighted sequences show: a hyperdense lesion localised between the bulb and pons and extending to the mesoencephalon, cerebral pedicle and internal capsule (brainstem). Diagnostic suspicion: glial neoplasm. Ophthalmological consultation is requested.
Results
Ophthalmological examination
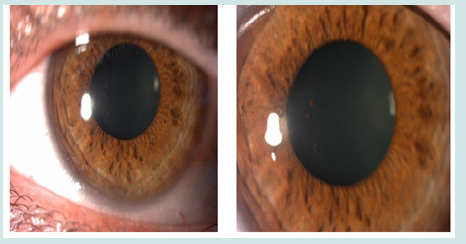
anterior segment: pigment on anterior crystalloid in OS (Figure 2)
Therapy: 1gr/ev methylprednisolone for 5 day, Prednisone oral 50mg/day, Cyclosporine 100mg/day
HLA typing: HLA B5 (51)
The clinical picture and diagnostic investigations led us to disprove the suspicion of cerebral glioma, proposing the diagnosis of NBS, which was confirmed by ophthalmological and neurological manifestations in a patient with a clinical history of recurrent oral aphthae (Table 1).
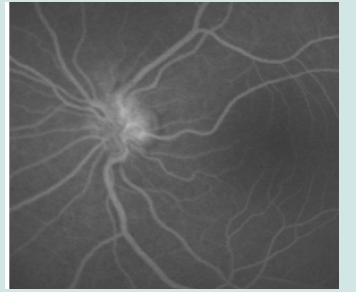
Figure 3: Therapy: 1gr/ev methylprednisolone for 5 day, Prednisone oral 50mg/day, Cyclosporine 100mg/day.
a) Follow-up: clinical and MRI regression after 3 months (please see Figures 3 & 4).
Development: after 5 months of therapy relapse of neurological symptoms, after one-year biological therapy with anti-TNF-α (adalimumab) 80mg was started (Figure 5).
Discussion
This case of neuro-Behçet, manifesting as a pseudotumoral lesion, reflects the need to consider this diagnosis in a young patient showing an acute neurological syndrome. Neurological onset is rare or difficult to interpret diagnostically and ophthalmological examination plays a key role in the differential diagnosis, looking for even the slightest signs that may lead the clinical picture towards NBS. The pseudotumoral form is a rare presentation of NBS, especially considering that only about 5% of BS patients develop neurological symptoms and manifestations. These lesions can mimic tumors, strokes, demyelinating and inflammatory diseases of the CNS, which is why neurologists must consider this diagnosis, as appropriate treatment can improve the clinical state and prognosis.
Conclusion
Neurological involvement in NBS is a prognostically negative factor in terms of morbidity and mortality. It mainly affects young male subjects. A parenchymal form and a non-parenchymal form are distinguished. The typical form of presentation is a meningoencephalitic syndrome with a sub-acute course in an overt picture of BS. The diagnosis is more complex where there is a non-definite Behçet’s picture, with a purely neurological onset. An unusual form of disease presentation is the pseudotumoural form, in which a suspected tumour mass is documented on imaging. These forms are rare, as in the case presented to us. About ten such cases are currently documented in the literature. These are complex diagnostic situations, in which careful ophthalmological assessment plays an important role in the diagnostic pathway, in the search for signs that may recognise a BS picture. The patient in our case comes to the observation of neurological colleagues with an acute clinical presentation of headache and right hemiparesis.
Magnetic resonance imaging documents a hyperdense lesion in the T2 sequences, involving the brainstem region. A diagnostic suspicion of glial neoplasia is therefore raised. However, on clinical examination, recurrent aphthae in the oral region are noted. An ophthalmologic consultation is then requested on suspicion of other pathology. There have been no controlled or comparative studies on the treatment of any aspect of NBS. Retrospective studies have shown that two-thirds of patients with brainstem or brain injury have a good recovery in response to steroid cycles, but the other third have recurrences. We recommend considering disease-modifying treatment (DMT) after significant parenchymal recurrence depending on severity, response to steroid, previous neurological relapse, disease course and other systemic features associated with BS.
We recommend considering a biologic agent, including TNF- α-blockers (relevant examples are infliximab, adalimumab, etanercept) or interferon α, when first-line therapies are ineffective or they are not well-tolarated by patients and if the disease has relapsed or it displays aggressive neurological or systemic features.
The main lessons we learned from our clinical experience and the subsequent advices for the future are as follows:
a. Consider the diagnostic hypothesis in young patients with manifestations of BS and
b. neurological symptoms;
c. Acute neurological onset is rare, but it should not be underestimated;
d. The ophthalmologist must lay a key role in each step of the differential diagnostic pathway.
References
- Pourmand R, Ali-Reza Nikseresht, Afshin Borhani Haghighi (2005) Neuro-Behçet disease. A review. The Neurologist 11(2): 80-89.
- Frohman EM, Frohman TC, Zee DS, McColl R, Galetta S (2005) The neuro- ophthalmology of multiple sclerosis. The Lancet Neurology 4(2): 111-121.
- Mastrolia M, Emilia Taddei , Ilaria Pagnini , Maria Canfora, Giacomo Emmi, et al. (2023) Behçet syndrome in children and adults: discovering similarities and differences by a comparative study. Rheumatology 62(SI2): SI189-SI195.
- Horany K (2001) Neuro-Bechet’s Disease: A clinical review. Neurosciences Journal 6(4): 224- 226.
- Peine B, Figueroa C, Robinette N (2022) Neuro-Behcet's syndrome: case report and literature review. Radiology Case Reports 17(9): 3064-3070.
- Akman-Demir G, Ayranci O, Kurtuncu M, Vanli EN, Mutlu M, et al. (2008) Cyclosporine for Behçet's uveitis: is it associated with an increased risk of neurological involvement? Clinical & Experimental Rheumatology 26(4): S84-90.
- Bettiol A, Fatma Alibaz Oner, Haner Direskeneli, Gulen Hatemi, David Saadoun, et al. (2022) Vascular Behçet syndrome: from pathogenesis to treatment. Nature Reviews Rheumatology 19(2): 111-126.