Lupine Publishers Group
Lupine Publishers
Review ArticleOpen Access
Neural Mechanisms and Causes of Non-Traumatic and Non- Pathological Strabismus. Comparison of Vision Therapy Programmes - A Systematic Review Volume 3 - Issue 3
Spiros Dielas OD*
- Professor, Raúl Pérez Ramos, Spain
Received:September 17, 2021; Published:October 07, 2021
Corresponding author: Spiros Dielas OD, Professor Raúl Pérez Ramos, Spain
DOI: 10.32474/TOOAJ.2021.03.000162
Abstract
Purpose: This study’s aim is to explore the various neural mechanisms and possible causes of strabismus, review vision therapy programmes suggested by different authors and observe potential variations of the aforementioned programmes in adults and children.
Methods: A search was conducted using various scientific databases and other sources. The risk of bias of the included articles was evaluated using the SYRCLE for animal studies, the ROBINS-I and the JBI tool for case reports.
Results: The search showed a total number of 28789 articles. After excluding irrelevant to this research articles, the final reviewed studies are 34.
Conclusion: Strabismus alters various brain areas the neural synapses and connections of which are affected. Numerous vision therapy procedures are recommended by the referenced authors while different programmes are applied in children and adults
Introduction
Strabismus is a misalignment of the eyes usually characterised by loss of binocular fusion. Depending on the severity and the age of onset it may co-exist with suppression, normal or abnormal retinal correspondence, poor or no stereopsis, reduced eye movements, nystagmus and amblyopia. However, the mechanisms and causes of strabismus remain under investigation. The reason for this is because strabismus is a condition that presents a multifarious and multi-level complexity. The visual system develops early in life. The first four to six postnatal months of age are crucial for the development of binocular fusion and stereopsis. As Katz and Shatz accurately observe, “the connection of the visual system is initially based on the formation of synapses which are controlled by molecular guidance cues” [1]. Moreover, Zhang, Poo, Kirkby and others correctly state that “when various stimuli by activity is received, the neural circuit starts to develop and coordinate [2], forming a local network of interactions within the cortex” [3]. The visual cortex (V1) is organized in columns of neurons coming from the lateral geniculate nucleus (LGN). Each column is driven by a dominant eye (namely the right or the left eye) [4]. Katz and Shatz interestingly suggest that “in early months of life these columns are absent in layer 4 (V1) which is responsible for binocular sensory fusion and stereopsis. Early visual activity and stimuli trigger anatomical rearrangements in the synaptic physiology of layer 4 neurons which are activated by both eyes and finally each formed column responds to one eye stimulus only” [1]. These signals from the left and right eye join in V1 and form neurons of binocularity in layer 4 which are essential for sensory fusion. A specific part of V1 and V2 neurons, are sensitive to relative disparity of a visual target or elements of a visual scenery and are responsible for stereopsis [5]. Consequently, it appears that visual disparity and eye alignment are closely intertwined. More precisely, the interruption of this interaction between visual disparity and eye alignment might be attributed as one of the causes of strabismus which is produced by abnormal sensory experiences early in life. Additionally, sensory fusion and stereopsis and a combination of binocular disparity of visual signals and accommodative response due to closeness of the visual target, drive the extraocular muscles of the eyes to change their angle. When the binocular system is developed normally the eye movements are precise and coordinated, while a disruption of the development of binocular fusion leads to poor stereopsis and motor guidance of the extraocular muscles and is associated with strabismus and suppression. The absence of sensory fusion and the abnormal development of binocular neurons of disparity, will eventually lead to the loss of critical error signals in the cortex or the brain stem, necessary for the orthoptic alignment and development of the eyes [5]. This may result in poor visual activity and stimuli in the early months of life. Moreover, this condition once developed may further lead to false calibration of the neural circuits and connections in multiple levels from the visual cortex to the motor neurons. The sensitivity of the binocular vision neurons and the binocular motor coordination of the eyes are connected with the level of development of the visual system through relevant visual experience in early stages of an individual’s life. This observation implies that the interruption of binocular vision encountered at an early age may lead to strabismus. The degree that the visual and visuomotor function may be influenced, due to the aforementioned early abnormal visual experience, depends largely on the age of onset, the duration and the type of interruption [5]. As a result, the ocular dominant columns in layer 4 of the visual cortex which develop through the visual input of each eye separately will be unavoidably affected. The following example, retrieved from Tychsen’s study, may frame better the said issue. In strabismic monkeys the binocular connections in the ocular dominant columns dropped by 50%, whereas the monocular ones were preserved. Yet, the ocular dominant columns of the strabismic eye were considerably less than in the non- strabismic one. The remained connections spurred abnormal and inhibitory reactions causing suppression in every row of columns which corresponded to the strabismic eye [4] Conventional treatments of strabismus include, inter alia, full prescription glasses in the case of accommodative esotropia, patching, penalisation using atropine drops or Bangerter filters if strabismus co-exists with amblyopia and surgery. Modern treatment methods developed in the last century are based on active vision therapy which focuses on the binocular function. More precisely, these methods aim to re- train the brain regarding the way it uses the two eyes together. Vision therapy varies from simple to complicated tasks and also incorporates different techniques and sensory integration. These techniques not only require the active effort and contribution of the eyes, but also the body movement and balance involvement. The equipment that is usually used includes inter alia: stereoscopes, Brock string, Hart charts, tranaglyphs, vectograms, Marsden ball, rotator, aperture rule, red/green filters, polarized and red-green reading bars, tachitoscope, fusion targets, prisms, lenses and other filters. Vision therapy’s core philosophy takes advantage of the neuroplasticity of the brain. This means that the brain has the extraordinary ability to continuously learn, improve and adjust to the specific existing surrounding conditions regarding the use of the two eyes together by forming new neurological pathways and synapses, establishing, internalising and generating new skills. Depending on the age and the severity of the problem, applied vision therapy has indeed demonstrated outstanding results in various cases of binocular vision dysfunctions. Strabismus is one of the binocular vision dysfunctions that vision therapy may be applied effectively, demonstrating satisfying and even exceptional results without the need for any surgical intervention. The way vision therapy makes this possible, is a rather interesting procedure. As already discussed, vision therapy’s main concept is based on the neural plasticity of the brain. The said plasticity of the visual system develops until the age of 9. Thus, greater positive results may be achieved through active vision therapy especially within this timeframe, namely from birth until the first 9 years of a child’s life. This is because the cells in the lateral geniculate nucleus and the visual cortex “die” after the age of 9, because of the lack of stimulation [6]. This does not mean that vision therapy in adults is not effective, but it may require longer periods of time and more intense efforts to achieve the desired results. Moreover, the said difficulty may discourage the individual from continuing the participation of the treatment, if the individual has established and internalised the visual dysfunction with habitual visual patterns. Depending on the severity of the problem, namely how deep the issue is established and whether the individual is aware or not of these habitual patterns, it may be close to impossible to “break” and “erase” the said patterns. An example of such a difficulty that will undoubtedly hinder vision therapy treatment applicability and results, is the existence of an adult patient who is diagnosed with alternating exotropia, visual acuity OU: 10/10, abnormal retinal correspondence (ARC), suppression and complete absence of Randot stereo fusion. In this type of strabismus it may be extremely difficult to “break” the alternate fixation patterns along with the ARC pattern. This also depends on how much embedded these patterns are in a patient’s visual framework and whether the individual is aware of them or not. For example, in the possible case of a strabismic adult patient who is not aware of the habitual visual patterns embedded into the strabismus problem, a vision therapy treatment plan may have a minimal effect on eliminating the said patterns. Needless to say, each case is unique, which implies that the success of a vision therapy programme depends not only on the optometrist’s expertise and experience, but also on the patient’s persistence, constant focus and determination to follow the instructions and guidance of the optometrist.
-According to Press [6]: In children, the expansion of binocular awareness and the cosmetic improvement of a strabismic deviation outweigh the relatively minor alteration in habitual vision. As a patient lives with his strabismus longer, and the adaptation builds, the elimination of the strabismus may be perceived as a tradeoff. An example is a patient with divergence excess exotropia who panoramically views at distance. This patient essentially enjoys the benefits of having a “picture within a picture” television screen. He has learned how to divide his attention - split the screen, so to speak - so that the fixating eye watches the main programme centrally, while the exotropic eye views a peripheral station. At the moment he aligns his eyes, he feels cheated out of one picture. Before commencing a vision therapy (VT) programme, a complete behavioral and functional visual examination is necessary in which not only the characteristics of the visual system are evaluated in an analytical way, but also the use of the visual system through observation of the patient’s behavior.
According to Vidal-López, 2018, [7] as depicted in p. 93, it is important to classify the strabismus by:
a) Age of onset: congenital if it occurs between birth and 6 months of age and early onset strabismus between 6 and 36 months of age.
b) Constancy: constant when the strabismus is always observed, intermittent when the condition is observed occasionally and accommodative when the accommodation is the primary cause of the squint.
c) Localisation: in distance and near vision.
d) Laterality: unilateral, when only one eye deviates, alternating, when the strabismus occurs in both eyes.
e) Directionality: horizontal, esotropia, if the eye turns nasally, exotropia, if the eye turns temporally. Vertical hypertropia when the eye turns upwards and hypotropia when the eye turns downwards. Rotational, incyclotropia and excyclotropia.
f) Magnitude: microtropia below 4 Δ, small-angle strabismus from 4 Δ to 9 Δ, moderate-angle strabismus from 10 Δ to 30 Δ and large-angle strabismus more than 30 Δ.
g) Correspondence: if the retinal correspondence is normal or abnormal. If it is abnormal, is it harmonious to the deviation angle or unharmonious.
h) Concomitance: concomitant strabismus is present when the angle of deviation does not vary more than 5 Δ in any gaze position. Non-concomitance is present when the angle of deviation varies in different gaze positions.
i) Organic origin: if the strabismus is related to a disease or syndrome if it is functional or not.
According to Von Noorden, 1988, [25] a successful therapy on strabismus needs to meet the following criteria:
a. Incomplete binocular vision: Which is characterised by orthotropia or eterophoria without symptoms, normal visual acuity in eyes, peripheral identification, normal retinal correspondence, central scotoma in one eye and low or absence of stereopsis. This outcome is the best possible.
b. Microtropia: small or absence of movement in cover test, possible mild amblyopia, peripheral identification, abnormal retinal correspondence and low or absence of stereopsis.
c. Small-angle strabismus (<20 Δ): this deviation is acceptable, with abnormal retinal correspondence, low or absent stereopsis.
d. Large-angle strabismus (>20 Δ): this deviation is noticeably obvious. Suppression is present and stereopsis is absent.
Van Noorden studied the results of strabismus surgery in infantile esotropia and assessed which outcomes could be considered as “successful” and whether this evaluation could be characterised as subjective, since the alignment of the eyes surgically does not necessarily enhance the binocular fusion of the brain. In fact, there is no intervention post surgically to stimulate the fusion and stereopsis of the brain. Instead, the visual system shall regain fusion and stereopsis by itself with no further stimulation intervention which leads to very low or even no results of such regainment. On the contrary, active vision therapy brings the two foveae together and re-aligns the eyes with the visual axis by enhancing binocular fusion and stereopsis and providing the necessary stimulation, so that the brain can rebuild neural synapses of binocularity in the visual cortex. Having set the pace for the analysis of this paper, the aim and structure of this work will be presented briefly. The aim of this review is to gather scientific literature about the neural mechanisms and potential causes of nontraumatic and pathological strabismus and the changes that occur in the visual cortex. Also, different approaches of vision therapy programmes set forth by different authors in strabismic cases will be critically observed aiming to evaluate whether any variances between treating children and adults exist. To this end, a systematic review is performed based on bibliography and internet search databases. Both tools are used to search for scientific evidence, possible explanations regarding the neural origins of strabismus, experiments in animals with induced strabismus and case studies and reports in the field of vision therapy treatment of strabismus.
Objectives
Many reviews, research papers and studies have been conducted by ophthalmologists and optometrists analysing the “peripheral” origins of strabismus related to abnormalities of muscles and pulleys of the eyes that affect the oculomotor system. Many cases of strabismus are indeed associated with syndromes and oculomotor dysfunctions, nevertheless little is known about the “central’’ roots of strabismus. So far, the research on central roots examines the potential neural changes and alterations of the binocular circuit and acknowledge that an abnormal neural signal is the effect of false input to the muscles and pulleys of the eyes, rather than the cause [8]. Similarly, more weight has been placed on the well- established approach in the methods of strabismus treatment, rather than vision therapy. Specifically, extensive studies regarding the efficacy and results of strabismus surgery and the use of pharmaceutical substances, such as the Botulinum toxin have been thoroughly investigated and little is known about other methods of intervention, such as vision therapy. Respectively, although a considerable quantity of scientific data is available on the effects of vision therapy in different visual dysfunctions such as convergence insufficiency, still a finite number of reviews are dealing with the vision therapy treatment programmes in various strabismic cases. Hence, the available literature about vision therapy strabismus plans written by different optometrists for adults and children is limited. It follows from the above that VT,being an alternative treatment of strabismus, is a field “under investigation”. To this end, this review will contribute through the gathering of available literature and bibliographic information on the analysis of the following topics: i) the potential neural causes and mechanisms of strabismus, ii) how different authors propose different vision therapy programmes in various strabismic cases and iii) the difference in approach to vision therapy treatment procedures for adults and children. The whole aim of this thesis is to provide specific information to a wider audience in the scientific community.
Methods
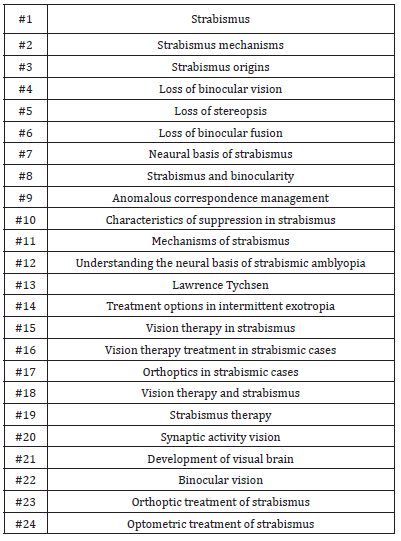
For the purposes of this review, a search was conducted on the scientific databases of PubMed, FrontiersIn, Plos One, Science Direct, and Journal of Neurophysiology. Further sources also include the OEPF (Optometric Extension Program Foundation), the COVD (College of Optometrists in Vision Development) and the E-Cronicon websites. Regarding the first five databases, the research was conducted using key research words and phrases that are presented in Table 1, describing with specific vocabulary the subject of the investigation. The search conducted on the OEPF website was focused on the Journal of Behavioral Optometry which revealed relevant articles in Volume 15 – Issue 1 – “Optometric Management of Patients with Incomitant Strabismus”, written by David L. Cook O.D. and Volume 13 – Issue 2 – “The Interface between Ophthalmology and Optometric Vision Therapy”, written by Leonard J. Press O.D. Although the title of the latter article does not match the subject of this review, further information on methods of optometric vision therapy is covered in Table 7 of the appendix section. The information of the said article is presented in a sequential and methodological plan for the strabismus vision therapy and this is why this article was considered relevant for the purposes of this paper. Furthermore, additional studies and reviews regarding the efficacy of VT, sequential plans of treatment and results of therapy in various forms of strabismus were retrieved from the COVD website. The said studies include and present the expertise of different authors who approached strabismus therapy on an ad hoc basis, namely according to the history of the patient, the age of onset and the diagnostic results of the patient. The titles, abstracts and citation information of the COVD studies are available on the “Summary of Research and Clinical Studies on Optometric Vision Therapy” document using the search engine of the website and typing the phrase “summary of research on optometric vision therapy”. The studies were looked up on PubMed database for further review and availability status.
However, the full text of a considerable number of studies was not available for review due to the absence of DOI number which is essential in tracking the full text. Last but not least, the review of “The Power of Effective Vision Therapy” written by Joseph Pederzolli in 2019 was specifically searched on E-Cronicon. The “Origins of Strabismus and loss of binocular vision” written by Emmanuel Bui Quoc and Chantal Milleret published on 25th September 2014 found in Frontiers In integrative neuroscience Volume 8 – Article 71, formed the basis for further search of the neural mechanisms and causes of strabismus, and for tracking other relevant studies in the reference section. Additionally, another article that included a rich section of relevant references on strabismus is the “Neural mechanisms of oculomotor abnormalities in the infantile strabismus syndrome” written by Mark M.G. Walton, Adam Pallus, Jérome Fleuriet, Michael J. Mustari and Kristina Tarczy-Hornoch, published on 10th April 2017 by J Neurophysiol. The references section of other studies was also utilised to pinpoint experiments in cats and monkeys with induced strabismus and changes in their visual cortex, the neural wiring of retinal waves in mice and the development of the visual brain and to supplement information on the changes that occur in V1 and V2 and how other sections of the brain controlling the oculomotor movements are affected. As mentioned before, the research found on vision therapy was limited to reviews on its efficacy in strabismus, the role of vision therapy in various forms of strabismic cases, orthoptics programmes and a few vision therapy case studies and reports on adults and children. All studies reviewed and included herein were written in the English language. No other limitations were imposed with regards to the eligibility criteria in the year of publication, publication status and length. It should be noted that a number of studies were reviewed, however only a few were selected for the purposes of this review according to the following criteria:
a. Articles referring to strabismus the aim of which is to explain the possible neurological changes in the visual pathway and the visual cortex, the oculomotor abnormalities and the changes in the brain areas that control the eye movements, the role of uncorrelated binocular input in strabismus, the loss of binocular fusion and stereopsis, the neural basis of suppression and strabismic amblyopia, the early development of the visual system and the interconnections to various cortexes and the development of binocular fusion and stereopsis.
b. Articles referring to induced experimental strabismus in animals aim to explain the modifications of the visual cortex connections, neural deficits, deficits in the synapses of binocular fusion and stereopsis and neural correlations.
c. Articles describing the characteristics of suppression and anomalous retinal correspondence and their clinical assessment.
d. Articles referring to vision therapy and orthoptics which describe treatment procedures and sequential plans, the efficacy of therapy in various forms of strabismus and case studies and reports in children and adults.
As far as the aforementioned selection criteria of articles and case studies is concerned, the following observations shall be noted. Firstly, the titles and abstracts were reviewed in order to exclude irrelevant subjects of investigation. Secondly, duplicates in studies which shared the same citation, same author(s), title, publication date, volume and issue were omitted. Thirdly, the complete texts of the remaining reviews were studied in order to assess and select the ones that complied with the aforementioned criteria and research pursuits of this study. Articles describing traumatic, pathological, accommodative, muscle, pulley and syndrome related causes of strabismus, the surgical intervention in muscles and pulleys of the eyes, the use of toxins, pharmacological preparations and patching methods in cases of strabismic amblyopia, were excluded. The only exception in patching as a method of intervention is the use of Bangerter filters and binasal occlusion combined with vision therapy techniques. The reason for this is that Bangerter filters enhance binocularity and contrast sensitivity in amblyopic cases, whereas binasal occlusion enhances peripheral fusion of the retina which in combination with vision therapy activities will contribute to the eye alignment of strabismic cases. An article describing the use of Bangerter filters for amblyopia was excluded because it focused on a different subject. However, a few articles that were included herein describe the use of binasal occlusion combined with vision therapy procedures. The risk of bias assessment was performed in all experimental studies in animals, humans, case studies and reports using specific tools that are described analytically in the Results section. Finally, all included studies were gathered in two separate tables; Table 6 includes the strabismus studies and Table 7 the vision therapy reviews and studies.
Results
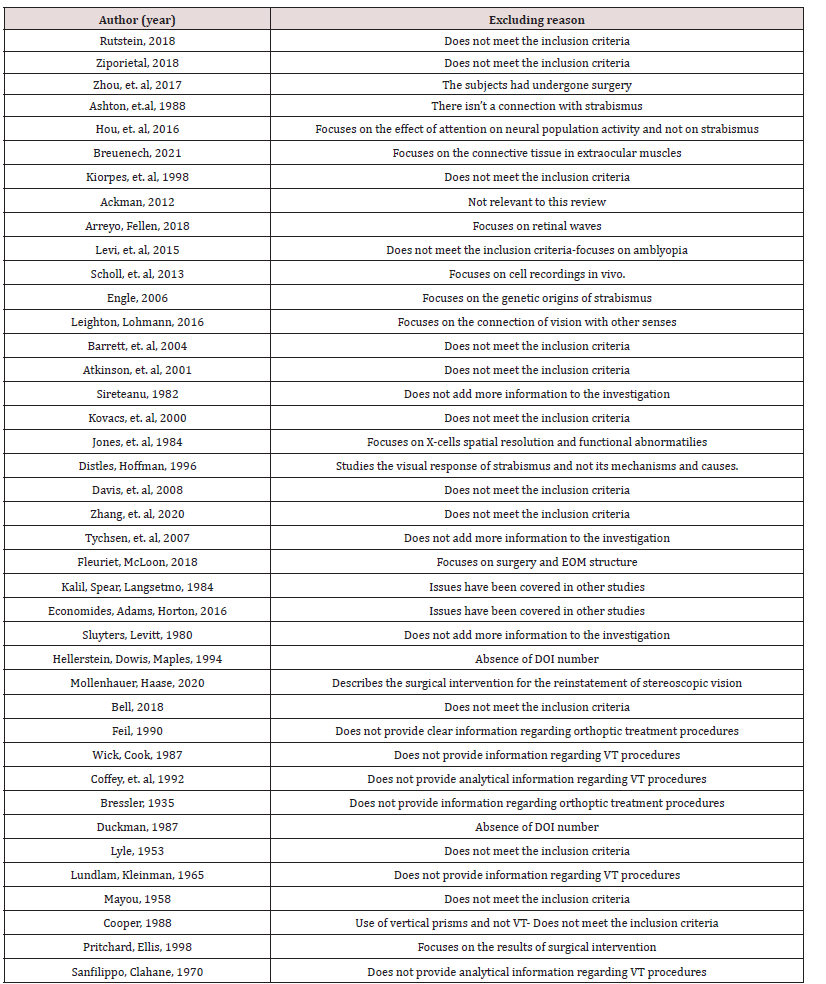
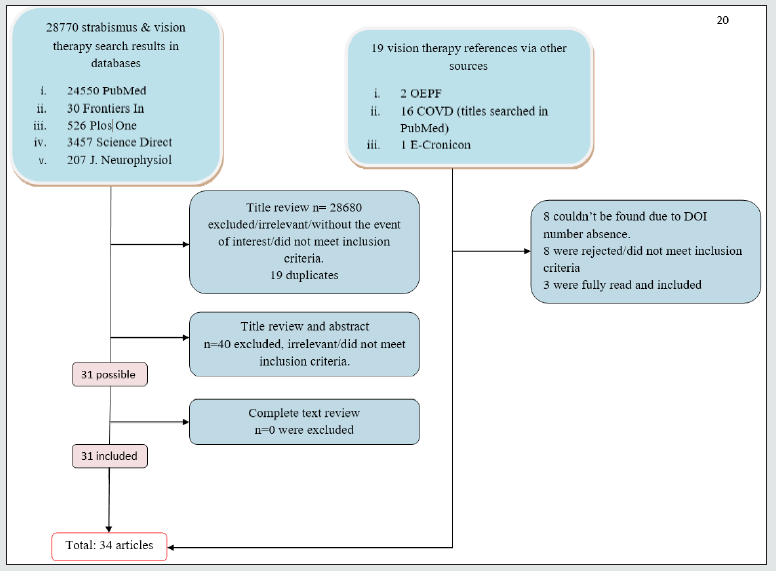
The total number of search results regarding both strabismus and vision therapy topics were 28,770. As already discussed, a considerable number of these studies were irrelevant to the subject of this review, while many of the results did not meet the aforementioned selection criteria. Therefore, 90 articles were selected. After rejecting 19 duplicates, 71 articles were reviewed based on their titles and abstracts. Finally, 40 of these articles were rejected as being irrelevant to this review. Thus only 31 articles were ultimately deemed as relevant and therefore fully reviewed. Three (3) other relevant articles were retrieved from other sources (OEPF, COVD and E- Cronicon) collecting 34 articles in total for this review. Flowchart 1 presents in a clear manner the process of selection and rejection of articles from both sources. As mentioned, the COVD articles were searched on PubMed database. Eight (8) out of 16 articles were not available and impossible to be found due to the absence of their DOI number. Eight (8) articles were rejected as they did not meet the inclusion criteria and did not provide vision therapy programmes in a descriptive manner. The result is the complete exclusion of the COVD list. Finally, 2 articles retrieved from OEPF and one from E-Cronicon were included, making a total of 3 articles from other sources. Consequently, the final number of articles included in this review from both sources is 34.
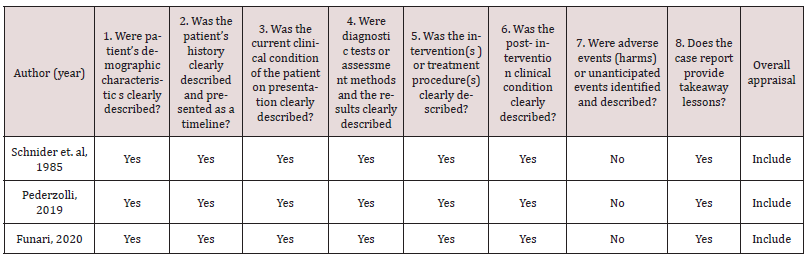
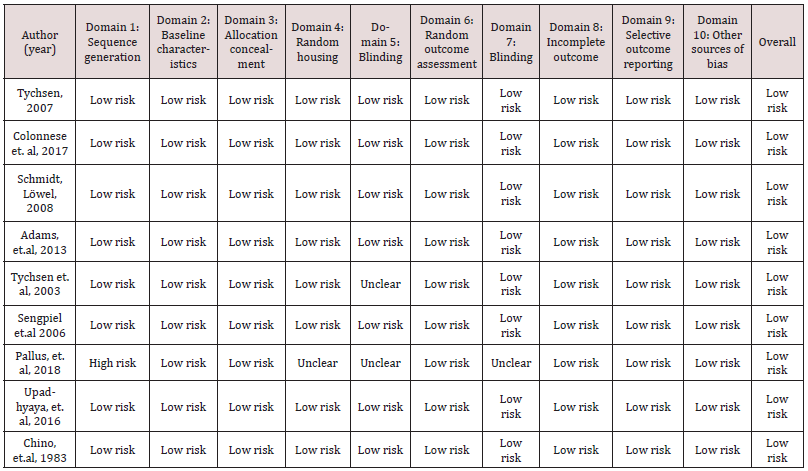
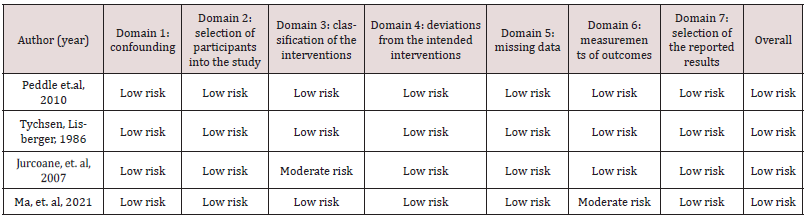
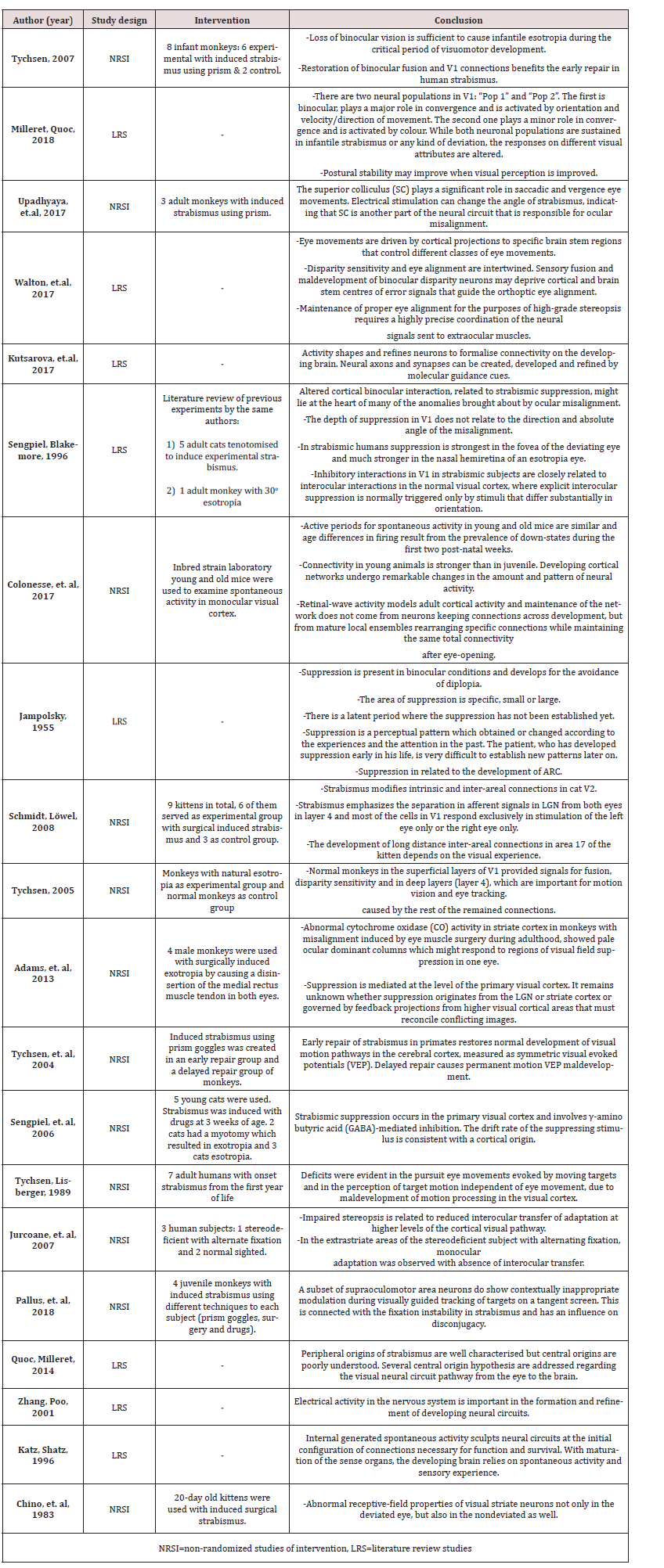
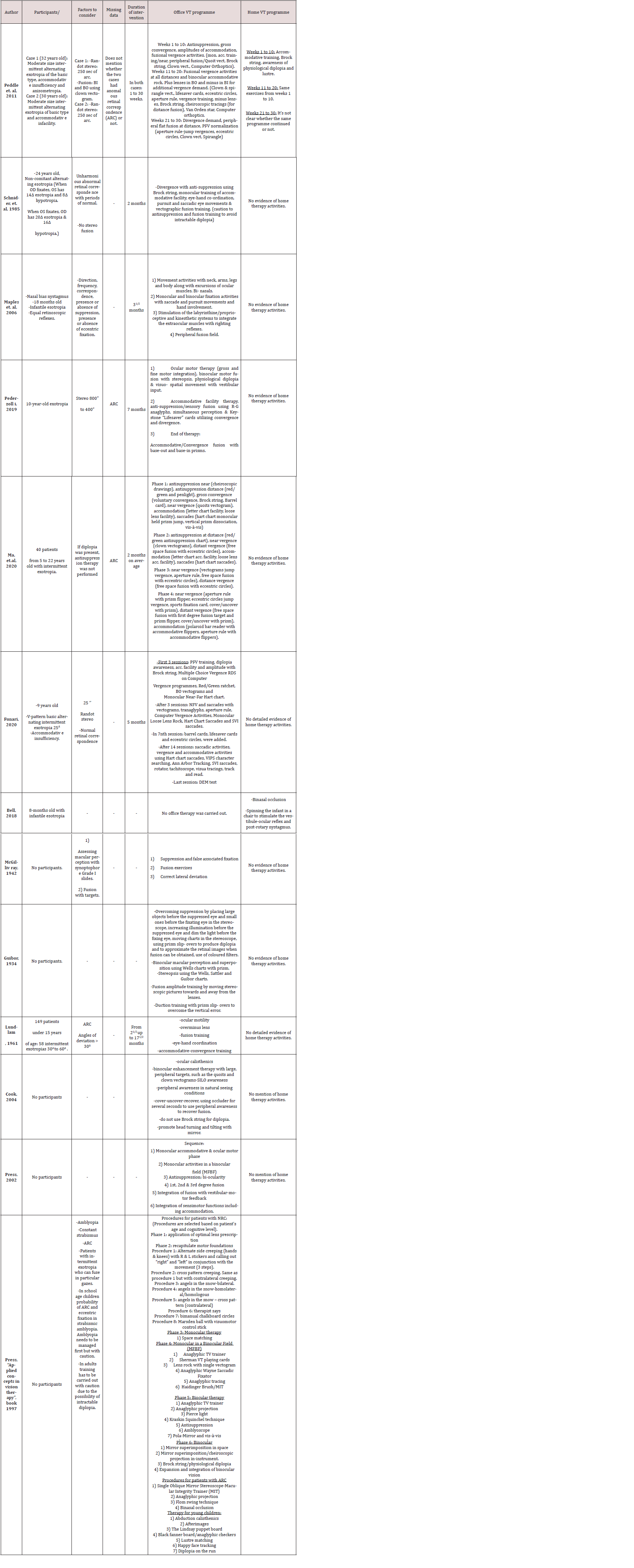
Various risk of bias tools were utilised for the analysis of nonrandom studies describing the participation of individual patients, animals and humans. In the context of risk of bias assessment, Table 3 sets out studies of intervention based on experiments on animals with induced strabismus and the SYRCLE risk of bias tool for animal studies. Also, the ROBINS-I risk of bias tool was useful in assessing the risk of bias in non-random studies of intervention in humans. The results of this assessment can be found in Table 4. Furthermore, vision therapy case reports including one patient were evaluated for potential risk of bias according to the JBI tool for case reports presented in Table 2. Generally, the risk of bias assessment performance revealed that the relevant risk of the reviewed studies is rather low, since animal selection, housing and intervention criteria were carefully considered. The potential intervention bias of the scientists is also low; and the scientists who conducted the study were surprised about cases where the outcome of their study differed from their hypothesis. The same was observed in non-random human studies, case studies and reports. The summary Tables 6 and 7 in the appendix section present the participants, the diagnosis, the main conclusions and interventions of the reviewed studies the subject of which is vision therapy and strabismus respectively. Notably, a meta- analysis was not possible, because many studies measured different data: a great number in animals and few in humans, while a number of studies did not mention any relative risk values; thus, it was deemed appropriate for the review results to be presented in Tables 6 and 7 in the appendices section. To be more precise regarding the collection of data from the reviewed studies, Table 6 summarises the ones that focus on strabismus experiments, reviews of literature data, literature reviews containing information about the development of visual brain and articles describing the changes in synapses of neurons and the neuroplasticity of the brain. What is more, Table 7 summarizes all studies found in vision therapy programmes of strabismus treatment written by different authors.
Specifically, Table 7 includes the author, the participant(s), the diagnosis that was identified and further factors to consider which supplements the diagnosis data. Furthermore, the “Factors to Consider” column includes data that significantly influence the vision therapy treatment and results. Factors that potentially facilitate VT efficacy are the following: existence of some degree of fusion, normal retinal correspondence, absence of suppression - although this is a rarely encountered situation - and intermittent exotropia cases with a degree of fusion in specific position of gaze. Factors that potentially complicate and hinder VT effectiveness are the following: absence of fusion, suppression, abnormal retinal correspondence, amblyopia, presence of diplopia and eccentric fixation. In certain reviews the aforementioned abnormalities were presented as a general informative guidance for additional dysfunctions of strabismus and were not assigned to specific cases. Furthermore, the “Missing Data” column of Table 7 includes data that was neither available nor mentioned in the study yet the said data may have played a significant role in the treatment procedures and subsequent results of therapy. Finally, the columns “Office VT programme” and “Home VT programme” sum up the vision therapy protocols proposed by each author and describe the procedures in the office and home therapy.
A considerable number of studies omitted references regarding the significant contribution of home vision therapy activities. The “Applied concepts in vision therapy” book written by Leonard Press provides relevant information on the efficacy of VT treatment in strabismus, yet the book chapters 8 and 16 which were studied for this review do not address any home vision therapy activities. The author states that vision therapy procedures of other visual dysfunctions can be used for the treatment of strabismus without though specifying which procedures could be applied in the context of strabismic cases which are mentioned in Chapter 4 of the book.
Discussion
According to the results of this systematic review, strabismus affects many areas of an individual’s brain. These areas include inter alia: the lateral geniculate nucleus located in the thalamus which is the principal pathway for visual perception and location [5], the intra-areal connections of V1 and V2 and inter- blob zones found in layers II-III, IV-B, IV-C-α and V located in the visual cortex and receive stimuli activity by orientation, and the velocity and direction of movement [9] and layer 4 in V1 which is responsible for stereopsis. Abnormalities in layer 4 may result in poor or even no stereoscopic vision a result which is characteristic in most forms of strabismus. Additionally, the binocular connections of the ocular dominant columns in the visual cortex are also influenced and reduced whereas the monocular ones are maintained [4]. Moreover, the oculomotor system and the brain centers that control the eye movements are affected as well. These centers are: the superior colliculus in the midbrain which plays a major role in saccadic eye movements, the cerebellum for eye movement control and nystagmus, the extrastriate visual areas in the “dorsal” and “ventral” stream which play a major role in saccadic, pursuit and the vergence eye movements to visual targets and the vestibuloocular reflex which moves the eyes in opposite direction from the head movement [5]. Furthermore, the presence of suppression in strabismus when the two eyes are open appears to relate to altered cortical binocular integration and interocular inhibitory interactions in V1 [10] a result closely associated with past visual experiences and attention of the strabismic subject [11].
The aforementioned areas in the brain are possibly affected simultaneously, depending on the severity of an individual’s condition and the age of onset of the symptoms. Nevertheless, diversity among strabismic cases is present and each case is a unique combination of abnormalities, severity of dysfunctions and affected brain areas. For example, some cases may present fusion capabilities in particular gaze positions, while others sufficient vergence eye movements which can be functional up to a certain point, in a few cases suppression might not be deeply rooted as an inhibitory visual mechanism whereas other cases may not show head and postural imbalance control. Therefore, certain patients may display good diagnostic characteristics which may enable the best possible VT result, whereas other patients may demonstrate severe conditions and abnormalities affecting the efficacy and methods of treatment used in vision therapy. There is one mechanism that is almost always present among the different encountered cases and that is suppression which is not affected by the angle and direction of deviation and, as mentioned before, it may or may not be deeply rooted as an inhibitory mechanism. However, studies have shown that suppression is much stronger in the nasal hemiretina of the esotropic eye [10]. Having mentioned the parameters that affect the severity of strabismus cases, it is equally important to focus on any potential identifiable aspects that enable the normal development of the brain and the changes that are provoked by strabismus while the brain is developing. The binocular synapses of the visual system prenatally are connected, already developed up to a certain point and ready to receive input when the eyes are opened for the first time. The binocular circuitry and cortical networks form and rearrange new synapses, connections and maintain the network by receiving continuous stimuli [3], disparity sensitive error signals which guide the orthoptic eye alignment [5] and molecular guidance cues [12]. When the received stimulus is poor or lost, the connections and synapses are reduced or even obliterated, disparity error messages are absent and eye alignment maintenance is affected, resulting in abnormal signals to the extraocular muscles and ultimately in the misalignment of the eyes. The various possible causes of such an abnormal function between the eyes and the brain, are extensively discussed on the “Origins of strabismus” review, written by Quoc and Milleret in 2014. This review describes in detail a considerable number of possible errors and abnormalities in the visual pathway which pave the way to scientists for additional research towards the understanding of the binocular disruption. However, it remains unknown what happens first; the loss of binocular fusion or the eye misalignment? This is a question that, if answered, will certainly shed light on the main causes of strabismus which will probably make strabismus treatment more specific and hopefully more efficient for both adults and children.
In the meantime, and before answers to the aforementioned questions are justifiably delivered, a promising solution is the exploitation of the brain’s unique capacity of neural plasticity and the exceptional ability of the visual system to create new synapses and connections with proper guidance and stimulation. This is why VT is considered to be a more promising alternative solution to strabismic cases since it is based on the continuous brain activity and its ability to re-build the lost connections and also re-train the brain to keep the orthoptic eye alignment by maintaining sensory and motor memory. This can be enhanced when the stimulation received from the various activities is repetitive up to the point of internalisation and automation. Scientific reviews also present the effect of strabismus in other areas of the brain which may result in abnormal head and body posture, orientation and balance. Consequently, it is logical to combine eye exercises with body, posture, balance, vestibular and orientation exercises. The combination of these exercises features VT as a promising holistic treatment approach of strabismus. The said treatment may result in improving a child’s life when it comes to school performance and other activities, such as sports in which the effective coordination of the eye movements is crucial. To this end as recommended, future research studies may focus on the observation of the brain areas that are affected in strabismus before and after vision therapy by using technological means of brain imaging, such as fMRI and other techniques. The results will most probably show the efficacy of VT treatment compared to other passive treatments, such as surgery, patching in strabismic amblyopia cases and Botinulum toxic use and will provide both information and clarity on the causes and mechanisms that stimulate strabismus as well as the relevant alterations in the brain. As far as the vision therapy study reviews is concerned, a variety of visual therapy programmes is presented in Table 7 describing different cases of eye deviation and concomitant eye dysfunctions, focusing mainly on the application of antisuppression, eye movement, peripheral, monocular fixation in a binocular field (MFBF) and fusion exercises. Each researchertherapist utilises a different sequential protocol of exercises depending on the age of the patient (infant, children or an adult), the age of onset of the problem, the characteristics of the visual system, the diagnosis and the co-existence of further abnormalities that accompany strabismus. The severity of these abnormalities will affect the treatment protocol in VT. Another consideration for the selection of procedures in a VT programme is the patient’s cognitive capacity; for example, a 3-year-old is not ready to read and execute mathematical problems comparing to a 7-year old child. Furthermore, key factors for a successful VT programme are connected with the cooperation of the child in the office treatment, compliance with office and home therapy and willingness of the parents to follow and implement the instructions given by the optometrist. A successful VT programme depends a lot on these parameters and an uncooperative patient makes the treatment process difficult for implementation and leads to uncertain results.
In infants, the therapy is passive focusing on peripheral activation, movement activities including the body, stimulation of labyrinth/proprioceptive and kinesthetic systems, monocular and binocular fixation activities with saccade and pursuit movements using fixation targets that keep the interest of the infant [13]. Stimulation of the vestibular-ocular reflex and post-rotary nystagmus is also a practice that is used in infants according to Bell (2018). In children from 5 to 13 years of age, the standard vision therapy procedures may be implemented along with games and computer orthoptics. However, a vision therapy sequence must be carefully selected as at this age various abnormalities may have been developed and rooted in the visual system such as suppression and abnormal retinal correspondence. If ARC is deeply rooted, a VT programme focusing on antisuppression techniques will not bring good results, but rather intractable diplopia. Hence, the therapist has to consider key differential diagnostic factors in order to deal with the strabismus abnormalities that can be solved aiming to establish functional vision. Also, fusion is the ultimate and final goal of a vision therapy programme. According to Press (1997), “Brock did not accept the patient for treatment, if he believed that the patient could not possess the capacity to achieve fusion”. Fusion is a differential diagnostic factor when examining the patient for the first time, because if the patient possesses this capacity even in specific position of gaze and preferably in Randot stereo test, then the optometrist may be able to bring out the optimal VT result of functional binocular vision.
A generic sequential programme of vision therapy for children with strabismus and normal retinal correspondence would initially include activities focusing on antisuppression, ocular motility, accommodation, convergence and divergence, peripheral awareness and fusion, monocular, MFBF and later biocular and binocular activities to achieve fusion. If strabismus is the first diagnosis and another dysfunction is present and detected as secondary, such as accommodative insufficiency, then activities that focus on the improvement of accommodative facility and amplitude, such as monocular loose lens rock, Hart chart, aperture rule, Brock string can also be included in the primary care of strabismus [14].
Older studies which describe orthoptic treatment techniques lack the holistic approach of today’s vision therapy procedures. Guibor’s 1934 and McGillivray’s 1942 reviews focus mainly on the procedures of overcoming suppression and re-aligning the eyes by achieving only a degree of fusion. The antisuppression techniques of these studies are based on increasing illumination before the suppressed eye, using coloured filters and prism slip-overs causing diplopia. The recommendation of the authors on the binocular macular perception and stereopsis enhancement is to use the Weels, Sattler and Guibor charts. In addition to this, the synoptophore and fusion targets increase the fusion amplitude [15,16]. Lundlam’s review in 1961 comes closer to modern techniques and philosophy of vision therapy encompassing ocular motility, eye-hand coordination, accommodative, convergence and fusion training [17]. Currently, other authors, such as Cook and Press, focus the vision therapy treatment on peripheral fusion and monocular fixation in a binocular field techniques. At the initial stage of therapy of strabismus these techniques are useful stepping stones in improving peripheral awareness. The same authors emphasise that antisuppression and Brock string techniques shouldn’t be used if diplopia is considered to become intractable [18,19]. Press, in his book, commences the therapy by integrating procedures of body movement, such as the alternate side creeping utilising hands and knees with right and left stickers and calling out “right” and “left” in conjunction with the movement, angels in the snow, games such as “Therapist says” and Marsden ball with visuomotor control stick. As the therapy progresses, the treatment shifts towards monocular training which is the steppingstone for MFBF activities, such as bimanual chalkboard circles, Wayne-saccadic fixator, Sherman VT playing cards, anaglyphic tracing and Macular Integrity Tester (MIT). The next phase incorporates biocular therapy focusing on balancing the two eyes as much as possible. Biocular exercises include anaglyphic TV trainer, Pierce light, Kraskin-Squinchel technique, antisuppression, amblyoscope, pola-mirror and visà- vis. At the final stage are the binocular treatment techniques which include the mirror superimposition in space, cheiroscopic projection in-instrument, Brock string/physiological diplopia, expansion and integration of binocular vision. Vision therapy in adult strabismic cases with normal retinal correspondence includes antisuppression, convergence, divergence, fusional vergence and computer orthoptics techniques [20]. A different approach in therapy is necessary when abnormal retinal correspondence is present. Leonard Press in his book “Applied concepts in Vision Therapy” mentions the following procedures: single oblique mirror stereoscope-macular integrity trainer (MIT), anaglyphic projection, Flom swing technique and binasal occlusion.
Strabismus treatment programmes of vision therapy differ between children and adults, according to Leonard Press in his book “Applied concepts of Vision Therapy” who includes a separate section with specific therapy activities for young children. These are: abduction calisthenics, afterimages, the Lindsay puppet board, Black fanner board/anaglyphic checkers, luster matching, happy face tracking and diplopia on the run. At a first glance, most of these activities seem like a simple game exercise, yet their purpose is to practice the missing visual skills in an individual’s strabismic case and reduce the symptoms of the strabismus visual dysfunction. Young children find it often difficult maintaining attention and focus for long periods of time. It is very helpful when the therapist demonstrates a variety of exercises in his quiver by which the child does not lose interest in the process. The engagement of a child’s attention plays a significant factor in the efficacy of VT treatment. Moreover, it is equally important that the activities in a VT programme shall relate to the cognitive level of the child. Adult patients are able to maintain attention on activities that do not look as fun as those in children. The communication between the therapist and an adult patient may differ from that with a child; for example, an adult patient with previous visual experiences may be more capable in describing the visual changes that occur during an exercise. Needless to say, this is not the rule in every adult and child case, as many are the times when the communication between a small child and a therapist is excellent. However, a therapy programme of a strabismic adult patient is important to be executed with caution, careful consideration of the involved activities and thorough diagnostic optometric evaluation. If abnormal retinal correspondence (ARC) is present in the strabismic eye, antisuppression activities may lead to intractable diplopia. Hence, before commencing a VT programme, a complete optometric evaluation provides necessary information regarding the visual problems and abnormalities related to the strabismus of the individual, thus helping the therapist design a taylor-made VT treatment programme that will encounter the visual dysfunctions and suit the visual needs of the patient. Finally, the following treatment procedures are recommended by the author of this review. Specifically, binasal occlusion is very helpful as an initial step in “breaking” an esotropic deviation and potential cross-fixation. Binasals enhance the peripheral awareness of the strabismic eye in far and close distances. Furthermore, in cases where normal retinal correspondence is present, antisuppression techniques may be incorporated into the therapy programme, whereas the same techniques must be completely avoided in patients with abnormal retinal correspondence. When ARC is deeply rooted into the visual system and the individual presents fusion abilities using the new point on the retina, then the best option would be to amplify the ARC point of fusion. An effort to “erase” the new retinal focus point utilising antisuppression techniques may lead to intractable diplopia. As mentioned before, the enhancement of the ARC retinal point of the strabismic eye along with the NRC retinal point of the non-strabismic eye, helps to maintain fusion and avoid intractable diplopia.
VT procedures shall also include binocular peripheral awareness combined with binasal occlusion, eye movement exercises using gross targets and engaging saccades and pursuits and MFBF activities which are the stepping stone for biocular and binocular procedures. At the final stage there are the biocular and binocular activities where fusion is practiced and enhanced.
Conclusion
Strabismus demonstrates a polymorphy of symptoms of visual dysfunctions, such as amblyopia, suppression, abnormal retinal correspondence, nystagmus, absence of stereopsis and vergence and eye movement abnormalities. The collection of data studied from different reviews in strabismic animals and humans present the alteration that occurs in areas in the brain that control binocular fusion and eye movements. Areas in V1 present deficits in neural synapses and connections, binocular ocular dominant columns and demonstrate abnormalities in layer 4 which is responsible for stereoscopic vision. Oculomotor areas such as the superior colliculus and the cerebellum which both control the eye movements and nystagmus respectively and extrastriate visual areas in the “dorsal” and “ventral” stream and the vestibulo-ocular reflex are also affected.
Vision therapy procedures applied in different strabismic cases indicate that a part or even full binocular fusion and stereopsis may be recovered along with the orthoptic alignment of the eyes. A variety of combination of VT activities is recommended by different authors depending on the age of onset, the diagnostic factors, the cognitive capacity of the patient and the cooperation with the therapist. Furthermore, VT procedures are different in infants, whose therapy is passive, rather than in children and adults. As far as the differences in VT procedures in children from 6 ~ 7 years of age and adults is concerned, a similar approach is observed by the different authors, yet with minor variations not only in the order of activities, but also in incorporating other exercises. Moreover, different VT procedures apply in both adults and children, when other abnormalities, such as amblyopia and abnormal retinal correspondence co-exist along with the strabismus problem. VT activities must be carefully selected when intractable diplopia is considered to be a possible result. Hopefully, more research in the neural mechanisms and causes of strabismus, vision therapy procedures and studies investigating the changes in the affected brain areas before and after vision therapy, shall occur in the future. This will pave the way for better understanding both the strabismus problem and the influence of VT treatment in the brain.
References
- Katz LC, Shatz CJ (1996) Synaptic activity and the construction of cortical circuits. Science 274(5290): 1133-1138.
- Zhang, LI, Poo MM (2001) Electrical activity and development of neural circuits. Nat Neurosci 4: 1207-1214.
- Colonnese MT, Shen J, Murata Y (2017) Uncorrelated Neural Firing in Mouse Visual Cortex during Spontaneous Retinal Waves. Front Cell Neurosci 11: 289.
- Tychsen L (2005) Can ophthalmologists repair the brain in infantile esotropia? Early surgery, stereopsis, monofixation syndrome, and the legacy of Marshall Parks. J AAPOS 9(6): 510-521.
- Walton M, Pallus A, Fleuriet J, Mustari MJ, Tarczy Hornoch K (2017) Neural mechanisms of oculomotor abnormalities in the infantile strabismus syndrome. J Neurophysiol 118(1): 280-299.
- Press LJ (1997) Applied Concepts in Vision Therapy. Santa Ana: Optometric Extension Program Foundation Inc. Mosby-Yearbook Inc.
- Vidal Lopez J (2018) Handbook of Vision Therapy. Published by SAERA school of advanced education, research and accreditation, SL.
- Bui Quoc E, Milleret C (2014) Origins of strabismus and loss of binocular vision. Front Integr Neurosci 8: 71.
- Milleret C, Bui Quoc E (2018) Beyond Rehabilitation of Acuity, Ocular Alignment, and Binocularity in Infantile Strabismus. Front Syst Neurosci 12: 29.
- Sengpiel F, Blakemore C (1996) The neural basis of suppression and amblyopia in strabismus. Eye (Lond) 10: 250-258.
- Jampolsky A (1955) Characteristics of suppression in strabismus. AMA Arch Ophthalmol 54(5): 683-696.
- Kutsarova E, Munz, M, Ruthazer ES (2017) Rules for Shaping Neural Connections in the Developing Brain. Front Neural Circuits 10: 111.
- Maples WC, Bither M, (2006) Treating the trinity of vision development: infantile esotropia, amblyopia, anisometropia. Optometry and Vision Development 37(3): 123-130.
- Funari K (2020) Vision therapy’s role in basic intermittent exotropia: a case report. Vision Development & Rehabilitation 6(1): 64-73.
- Guibor GP (1934) Practical details in the orthoptic treatment of strabismus. Arch Ophthalmol 12(6): 887-901.
- McGillivray J (1942) Orthoptic Treatment of Strabismus. Canadian Medical Association Journal 46(3): 265-267.
- Lundlam WM (1961) Orthoptic treatment of strabismus. A study of one hundred forty-nine non-operated, unselected, concomitant strabismus patients completing orthoptic training at the Optometric Center of New York. Am J Optom Arch Am Acad Optom 38: 369-388.
- Cook LD, (2004) Optometric management of patients with incomitant strabismus. Journal Of Behavioral Optometry 15(1): 10-16.
- Press JL (2002) The interface between ophthalmology and optometric vision therapy. Binocul Vis Strabis Q 17(1): 6-11.
- Peddle A, Han E, Steiner A (2011) Vision therapy for basic exotropia in adults: 2 case studies. Optometry 82(8): 467-474.
- Adams DL, Economides JR, Sincich LC, Horton JC (2013) Cortical metabolic activity matches the pattern of visual suppression in strabismus. J Neurosci 33(9): 3752-3759.
- Chino YM, Shansky MS, Jankowski WL, Banser FA (1983) Effects of rearing kittens with convergent strabismus on development of receptive-field properties in striate cortex neurons. Journal of Neurophysiology 50(1): 265-286.
- Jurcoane A, Choubey B, Muckli L, Sireteanu R (2007) A pilot study for investigating cortical binocularity in humans using fMRI adaptation. Strabismus 15(1): 33-37.
- Ma MM, Kang Y, Chen C, Su C, Tian Z, et al. (2021) Vision therapy for intermittent exotropia: A case series. J Optom 14(3): 247-253.
- Noorden GK (1988) A reassessment of infantile esotropia. XLIV Edward Jackson memorial lecture. Am J Ophth 105(1): 1-10.
- Pallus A, Walton M, Mustari M (2018) Activity of near-response cells during disconjugate saccades in strabismic monkeys. J Neurophysiol 120(5): 2282-2295.
- Pederzolli JM (2019) The power of effective vision therapy. EC Ophthalmology 10(5): 379-381.
- Schnider CM, Ciuffreda KJ, Selenow A (1985) Orthoptic effects on accommodation and related visual functions in an adult alternating esotrope. Ophthalmic Physiol Opt 5(4): 425-433.
- Schmidt KF, Löwel S (2008) Strabismus modifies intrinsic and inter-areal connections in cat area 18. Neuroscience 152(1): 128-137.
- Sengpiel F, Jirmann KU, Vorobyov V, Eysel UT (2006) Strabismic suppression is mediated by inhibitory interactions in the primary visual cortex. Cereb Cortex 16(12): 1750-1758.
- Tychsen L, Lisberger SG (1986) Maldevelopment of visual motion processing in humans who had strabismus with onset in infancy. J Neurosci 6(9): 2495-2508.
- Tychsen L, Wong AM, Foeller P, Bradley D (2004) Early versus delayed repair of infantile strabismus in macaque monkeys: II. Effects on motion visually evoked responses. Invest Ophthalmol Vis Sci 45(3): 821-827.
- Tychsen L (2007) Causing and curing infantile esotropia in primates: the role of decorrelated binocular input (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc 105: 564-593.
- Upadhyaya S, Meng H, Das VE (2017) Electrical stimulation of superior colliculus affects strabismus angle in monkey models for strabismus. Journal Of Neurophysiology 117(3): 1281-1292.