Lupine Publishers Group
Lupine Publishers
Research ArticleOpen Access
Comparative Study between Mohindra Retinoscopy and Subjective Refraction, in Young Adults with Accommodative Excess Volume 2 - Issue 3
Cátia Almeida1, Andresa Fernandes1* and Amélia Fernandes Nunes1,2*
- 1Clinical and Experimental Center of Vision Sciences, Universidade da Beira Interior, Portugal
- 2Center for Research in Health Sciences, ubiMedical, Universidade da Beira Interior, Portugal
Received:September 09, 2019; Published: October 15, 2019
Corresponding author: Amélia Fernandes Nunes, Center for Research in Health Sciences, Universidade da Beira Interior, Portugal
DOI: 10.32474/TOOAJ.2019.02.000140
Abstract
Purpose: The aim of this study was to compare the results of three refractive techniques: Autorefractor (AR), Mohindra Retinoscopy (MR) and Monocular Subjective (MS) and study the differences between the results of Mohindra Retinoscopy and Monocular Subjective test, in subjects with accommodative excess.
Methods: The refractive measurements were taken with the open field AR (Grand Seiko WAM-5500), the monocular subjective refraction and MR, and measures of accommodative flexibility and Monocular Estimated Method (MEM) were also taken, in 85 right eyes of 85 healthy university students. (22.3±2.4 years).
Results: Statistically significant differences were found on the spherical equivalent for the three techniques, with the Friedman statistical test (N=85; χ_F^2=42.771; p<0.0001). The MR is the technique that provide more positive results and the AR the most negative. Regarding astigmatic components there was no statistically significant differences found between the techniques, with de Friedman statistical test. Data were also analyzed based on accommodation function and there were no statistically significant differences found between subjects with accommodative excess and subjects with normal accommodation, for the spherical equivalent (N=74; H=1.785; p=0.410), and for J0 component (N=74; F=0.948; p=0.392), with the Kruskal-Wallis statistical test.
Conclusion: These results revealed significant differences between the three refractive techniques in young adults, independently of accommodative state. The open field AR overestimated some degree of accommodation during the refractive measurements and the MR was the technique that presented more positive results, even in subjects with normal accommodative function. Regarding astigmatic components, all the techniques provide similar results.
Keywords:Mohindra retinoscopy; accommodative excess; monocular subjective refraction; refractive state; university students
Abbreviations:Accommodative Excess (AE); Visual Acuity (VA); diopters (D); Monocular Estimation Method retinoscopy (MEM); Autorefractor (AR); Mohindra Retinoscopy (MR); Monocular Subjective (MS); Monocular Accommodative Facility (MAF); Early Treatment Diabetic Retinopathy Study (ETDRS); Minnesota Low Vision Reading Test (MNREAD); spherical equivalent (SE)
Introduction
The accommodative excess (AE) is the most prevalent dysfunction among the university students [1]. In this dysfunction, the patient hyper-accommodates, which implies an excessive accommodative convergence [2]. The excessive use of accommodative convergence will result in a pseudomyopia, what means a temporary transition from refraction towards myopia [3- 7]. As such, in individuals with accommodative excess, due to hyperaccommodation, there is a tendency to obtain more myopic results in the techniques of subjective refraction, which are the techniques usually used in clinic [2,8]. Other clinical signs found in subjects with AE are low astigmatisms against the rule, variable visual acuity (VA), failure or difficulty in relaxation of accommodation and low values on Monocular Estimation Method retinoscopy (MEM) (accommodative response without delay or with advance) [2,8]. In order to obtain a correct ocular refraction without the influence of accommodation, cycloplegic refraction should be used. The active principle of the drugs used is to relax and paralyze accommodation [2,3]. Cycloplegic retinoscopy, in addition to Subjective refraction, is a technique considered standard in the measurement of the refractive state [9]. However, it is associated with temporary symptoms of blurred vision, photophobia and discomfort due to paralysis of the accommodation. In addition, Cycloplegic Retinoscopy is contraindicated in people with heart problems, primary glaucoma, people prone to glaucoma (narrow anterior chamber angle), and hypersensitivity to any of the excipients of the drug [9-11].
According to Mohindra, the Mohindra Retinoscopy is a good substitute technique for Cycloplegic Retinoscopy and provides similar results when used the correct correction factor, without the disadvantages indicated, a fact supported by other authors [9,12,13]. Recently, the use of open field autorefractor has become a widely used technique for measuring refractive state [9]. There is scientific evidence showing that the use of the autorefractor, without cycloplegics, has a reasonable precision when compared to the values obtained by Cycloplegic Retinoscopy and Subjective Refraction [9,14-17]. However, there are also studies that show that the autorefractors without cycloplegics, fails to completely neutralize patients accommodation. In these studies, the results obtained by open field autorefractor leaded to a reduction in the accuracy of measurements between 0.01 and 0.38 diopters (D) towards myopia. This fact is especially relevant in people with large accommodative reserves [9,17-19]. The aim of this study was to compare the results of three non-cycloplegics refractive techniques: Autorefractor (AR), Mohindra Retinoscopy (MR) and Monocular Subjective refraction (MS), in university students. The purpose of this study was to evaluate the results of MR and the results of MS technique, to understand if the accommodation is being compensated, in addition to patients ametropia.
Methods
The data acquisition was performed between October 2017 and January 2018, at the Optometry Laboratory and the Clinical and Experimental Center of Vision Sciences. The project complied with the directives of the Helsinki Declaration and was approved by the Ethics Committee (CE-UBI-Pj-2018-002). Participants signed a free and informed consent, after knowing the nature of the study. A total of 85 university students’ volunteers (37 women and 48 men), aged between 18 and 30 years (mean age of 22.3±2.4 years), were evaluated. None of the subjects had strabismus, amblyopia, previous history of refractive surgery or pregnancy. Participants were also excluded from taking medication that would interfere with accommodative function. Inclusion factors were the achievement of usual visual acuity better or equal to 0.1 logMAR and presentation for optometric evaluation without contact lenses. Refractive and accommodative measures were taken. In order to study the refractive function.
The following acquisitions were made:
a) Refractive and accommodative measures were taken. In order to study the refractive function, the following acquisitions were made: Monocular habitual VA at 4 meters, using wellcontrasted ETDRS charts for far vision.
b) Mohindra Retinoscopy (MR), using test glasses, loose lenses, and esquiascopia rules.
c) Monocular Subjective Refraction (MS), using a CSO LCD monitor, in logMAR scale, test glasses and loose lenses. and
d) Autorefractor (AR), using the Grand Seiko WAM-5500 open-field autorefractor (Japan) with visual stimulus at far of 1.0 logMAR.
The following clinical tests were performed for the study of the accommodative function:
a) Monocular Accommodative Facility (MAF), performed on the habitual compensation of the subjects, using lens flippers of ±2.00 D and MNREAD chart with a stimulus of 0.2 logMAR; and
b) MEM, using an accommodative stimulus of 0.2 logMAR and spherical lenses.
The MR and the MS were performed by different researchers, to guarantee a greater veracity of the results, since the researchers didn’t know the value of one of the refractive techniques. MR was performed in a completely dark room after the volunteer had his eyes closed for five minutes to allow relaxation of accommodation. The measurement was taken in the right eye over the test glasses and it was used a combination of spherical and cylindrical loose lenses, with the left eye occluded. The volunteers were instructed to look right into the light of retinoscope, that was 50 centimeters away. After de procedure of retinoscopy, a value of +1.25 D was withdrawn from the final result.
Results
Considering the usual refraction of the volunteers who participated in this study, 44.7% had myopia, 52.9% were emmetropic, and 2.4% had hyperopia. The spherical equivalent of the usual refraction was divided according to criteria provided by the American Academy of Optometry [20,21]. The usual refractive error of the sample ranged from -7.75 to +2.25 spherical diopters. The maximum magnitude of astigmatism was -3.75 cylindrical diopters. For the comparative study between the results of the different refractive techniques used in this work, the powers obtained in sphero-cylindrical form were converted to their vector components according to Thibos [22]. The spherical equivalent (SE) and the astigmatic components in horizontal/vertical (J0) and oblique (J45) directions were calculated according to the expressions:
SE = S + c/2
J0 = − c/2 × cos(2×axis)
J45 = −C/2 × sin(2 × axis)
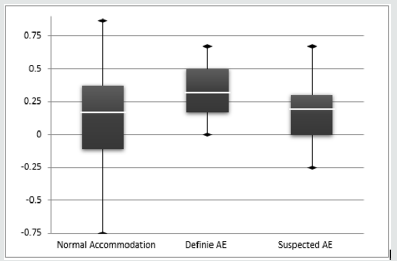
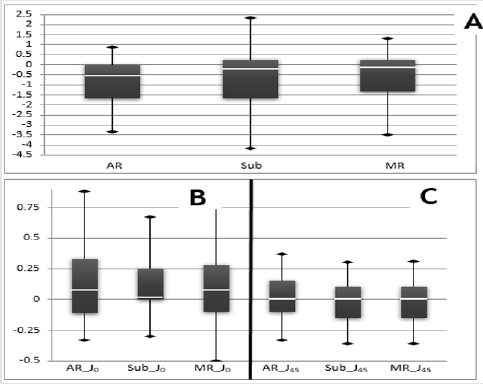
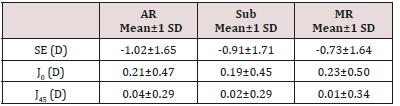
The graphs of (Figure 1) show the distribution of the values for the SE (part A), J0 (part B) and J45 (part C) components, obtained by each of the refractive techniques: AR, MS and MR. With respect to the SE component, it can be observed that of the three refractive techniques used, the open field AR was the method that presented more myopic values. The MR presented median results very similar to those of MS, although with slightly more positive values. Regarding the J0 component, it is observed that the median is slightly more positive in MR. The MS test presented median values very similar to the open field AR, for the J0 component. With respect to J45 component, the results are similar in all three refractive techniques. (Table 1) reports the mean and standard deviation of the SE, J0 and J45 components of the three refractive techniques. It is possible to observe that the mean differences between the techniques are around ±0.25 D, and MR presents slightly more positive values and the AR the more negative for the SE component. The comparison of the results of the three refractive techniques shows that for the SE component, the AR provides more myopic values, whereas the MR gives more hypermetropy values, and for the J0 and J45 components the techniques provide similar results. The differences found through the Friedman test, for the SE component are statistically significant, (2,85=42.771, p<0.0001) and the multiple mean comparisons reveals that there are statistically significant differences between all pairs of techniques. For the J0 component, the interpretation of the statistically test result (2,85=6.607, p=0.037) indicates that this component also presents significant differences, however through the multiple mean comparison test it is verified that there is no statistical evidence to state that there are differences between any pair of techniques. For the J45 component the differences between the techniques are not significant (2,85=5.801, p=0.055).
Table 1: Descriptive statistics (mean±SD) for the SE, J0 and J45 components, of the three refractive techniques.
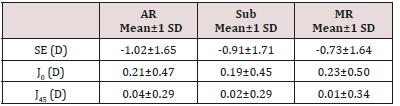
Figure 1: Distribution of the values related to SE (part A), J0 (part B) and J45 (part C) components.
In order to analyze the relationship between the accommodative state and refraction, the sample was stratified according to the accommodative state in the following categories: normal accommodation, definite accommodative excess, suspected accommodative excess, and other types of accommodative alterations. To carry out this division, the MAF and MEM test standards were used and are summarized in (Table 2). In this analysis, only the categories of normal accommodation, suspected accommodative excess and definite accommodative excess were considered, excluding subjects who presented other types of accommodative alterations. In order to compare the results of the refractive techniques, as a function of the accommodative state, two new variables, ΔSE and ΔJ0, were created, characterized by the difference between MR results and the MS results, for the SE component and for the J0 component, respectively. Only the SE and J0 components were studied since they are the parameters mentioned in the literature as those that can be associated with the accommodative excess that is, pseudomyopia and low astigmatism against the rule. (Table 3) shows the mean difference and the level of statistical significance among refractive techniques.
Table 3: Mean difference and the level of statistical significance for the ΔSE and ΔJ0, of the three refractive techniques.
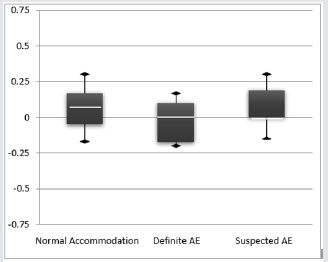
In order to graphically analyze these small differences between accommodative groups, the box plots of the SE and J0 components are shown in (Figures 2 & 3), respectively. The comparison of the results of the MR and MS techniques, as a function of the accommodative state, shows that for the SE component (ΔSE = MR-MS) the subjects with definite AE are those with higher mean values, meaning that the value obtained by the MS tends to be more myopic than the one obtained by MR. for the component J0 (ΔJ0 = MR-MS), the subjects with definite AE present lower average values, meaning that the results obtained by the MS tend to be more positive (presence of astigmatism against the rule) than those obtained by MR. Despite the differences observed graphically, there was no statistical evidence that those differences were statistically significant, for none of the components, SE (H2,74=1.785, p=0.410) and J0 (F2,74=0.948, p=0.392).
Discussion
The most prevalent spherical ametropia found in this study was myopia, with the low magnitude being the most frequent, which agrees with what is reported in the literature, for the same classification criteria for ametropia [23,24]. In relation to astigmatism, there was a greater predominance of astigmatism with the rule, a fact that has also been announced by other authors in young populations [25-28]. Regarding the accommodative state, the sample was divided according to the accommodative state in normal accommodation, definite accommodative excess, suspected accommodative excess and other accommodative alterations. Of the 85 volunteers, 11.8% were classified as having definite accommodative excess, 28.2% with suspected accommodative excess, 47.1% with normal accommodation and 12.9% with other accommodative alterations. The frequency rate found has a value within the same order of magnitude as those indicated by Porker et al, although slightly higher, a situation that is expected, as reported in the literature, due to the change in visual habits derived from the increasing use of new technologies and the increase of hours of intensive study that a higher education requires [1,29]. The main objective of this study was to determine if subjects with an accommodative excess presented differences between the refractive results obtained by an objective technique and a subjective one, performed routinely in clinical practice. As a subjective technique, we used the subjective test because it was considered the standard refractive examination and as objective technique, we used the MR because it is considered the objective refractive technique that presents values closer to those of the Cycloplegic Retinoscopy [9,15,30]. The identification of subjects with accommodative excess was based on the interpretation of the results of the MEM test and the MAF test, following the criteria suggested by other authors [31- 33].
The results revealed significant differences in SE component between three refractive techniques, and these differences were found to be identical in all groups, regardless of the accommodative state of the volunteers. The open-field AR tends to overestimate some degree of accommodation during refractive measurements, in university students, providing slightly more myopic values than the other techniques, which is also found by other authors and is well documented in the scientific literature [9,17,34,35]. Comparing the open field AR and MS techniques, although statistically significant differences were found through the Friedman test and the multiple mean comparison, these differences present a mean variation of ±0.11 D. These results are in line with those reported by Sheppard and others, who found differences between these two techniques ranging from 0.01 to 0.38 D, with the open field AR presenting the most negative values [35]. The results of this work showed that MR was the technique that provided less myopic results. Even in subjects with normal accommodation, the differences between MR and MS were around ±0.18 D. MR provided less myopic values than the MS, which coincides with the mentioned by Natarajan et al. This author concludes that although the values are similar, MR provides slightly higher values, possibly due to the accommodative tone of +0.75 D [36]. A single accommodative tonus value may not be advisable for all age groups and further studies should be conducted in relation to this. The results of this present study showed that for the age group of university students, the accommodative tone value of +0.75 D may not be the most adequate, since more hypermetropic values were obtained with the MR, compared to MS. Regarding the astigmatic components, no statistically significant differences were found between the refractive techniques. This means that all the techniques used provided similar results in relation to astigmatism, which is in line with found by Mohindra [37].
These results show that there are statistically significant differences for the SE component throughout the sample, with MR providing more positive results for all individuals, around ±0.25 D, regardless of the accommodative state. Although the findings are statistically significant, clinical routine may be interpreted as having little significance. However, the results of this study showed that the prescription of university students may be overvaluing myopia. Since myopia is the refractive error most prevalent globally, it is strongly related to the excessive use of the near vision [24,38,39]. University students make use of near vision because of the intensive study hours a high education requires. As such, this greater accommodative effort may influence refractive outcomes. The accommodation factor is quite controlled in children, however, there doesn’t seem to be much interest in being controlled in older age groups. Given the changes in lifestyles, increased use of near vision, and increased rates of myopia, university students are expected to present accommodative reserves that may interfere with manual refraction, if they are not controlled. More studies within this area are needed to study the effect of accommodation on refraction in young adults using cycloplegic refraction. As future work, one aspect that deserves attention is to verify if the correction factor of +1.25 D proposed by Mohindra, in this age group, is updated, considering that this study happened in the year of 1977, and until the date there are not studies that verify if it is a good correction factor, in order to minimize the influence of working distance and tonic accommodation. Another aspect that should by studied is the effect of accommodation on refraction in young adults and students, because of the great use of the near work.
References
- Porcar E, Martinez Palomera A (1997) Prevalence of general binocular dysfunctions in a population of university students. Optom Vis Science 74(2): 111-113.
- Scheiman M, Wick B (2014) Clinical management of binocular vision : Heterophoric, Accommodative, and Eye Movement Disorders (4th edn), Wolters Kluwer/Lippincott Williams & Wilkins, Philadelphia, USA.
- Seaber JH (1966) Pseudomyopia in Exodeviations. Am Orthopt J 16(1): 67-72.
- Jayakumar M, Kaul S, Jayakumar N (2012) Pseudomyopia in intermittent exodeviation. Indian J Ophthalmol 60(6): 578-579.
- Stratos AA, Peponis VG, Portaliou DM, Stroubini TE, Skouriotis S, et al. (2011) Secondary Pseudomyopia Induced by Amisulpride. Optom Vis Science 88(11): 1380-1382.
- Jones R (1990) Physiological Pseudomyopia: Optometry and Vision Science. Optom Vis Sci 67(8): 610-616.
- Chan R, Paul M, Trobe JD (2002) Spasm of Accommodation Associated with Closed Head Trauma: Journal of Neuro-Ophthalmology. J Neuro-Ophthalmology 22(1): 15-17.
- Elliott DB (2007) Clinical procedures in primary eye care. (3rd edn).
- Choong YF, Chen AH, Goh PP (2006) A Comparison of Autorefraction and Subjective Refraction With and Without Cycloplegia in Primary School Children. Am J Ophthalmol 142(1): 68-74.
- Vasudevan B, Ciuffreda KJ, Meehan K, Grk D, Cox M (2016) Comparison of objective refraction in darkness to cycloplegic refraction: A pilot study. Clin Exp Optom 99(2): 168-172.
- Yeotikar NS, Bakaraju CR, Reddy RPS, Prasad K (2007) Cycloplegic refraction and non-cycloplegic refraction using contralateral fogging: a comparative study. J Mod Opt 54(9): 1317-1324.
- Mohindra I, Molinari JF (1979) Near retinoscopy and cycloplegic retinoscopy in early primary grade schoolchildren. Am J Optom Physiol Opt 56(1): 34-38.
- Borghi RA, Rouse MW (1985) Comparison of refraction obtained by “near retinoscopy” and retinoscopy under cycloplegia. Am J Optom Physiol Opt 62(3): 169-172.
- Steele G, Ireland D, Block S (2003) Cycloplegic autorefraction results in pre-school children using the Nikon Retinomax Plus and the Welch Allyn SureSight. Optom Vis Sci 80(8): 573-577.
- Davies LN, Mallen EAH, Wolffsohn JS, Gilmartin B (2003) Clinical evaluation of the Shin-Nippon NVision-K 5001/Grand Seiko WR-5100K autorefractor. Optom Vis Sci 80(4): 320-324.
- Harvey EM, Miller JM, Wagner LK, Dobson V (1997) Reproducibility and accuracy of measurements with a hand held autorefractor in children. Br J Ophthalmol 81(11): 941-948.
- Wesemann W, Dick B (2000) Accuracy and accommodation capability of a handheld autorefractor. J Cataract Refract Surg 26(1): 62-70.
- Zhao J, Mao J, Luo R, Li F, Pokharel GP, et al. (2004) Accuracy of noncycloplegic autorefraction in school-age children in China. Optom Vis Sci 81(1): 49-55.
- Barry JC, König HH (2001) Non-cycloplegic screening for amblyopia via refractive findings with the Nikon Retinomax hand held autorefractor in 3 year old kindergarten children. Br J Ophthalmol 85(10): 1179-1182.
- Goss DA, Grosvenor T, Keller JT, Marsh-Tootle W, Norton T, et al. (2006) Care of the Patient with Myopia. American Optometric Association.
- Moore BD, Augsburger AR, Ciner EB, Cockrell DA, Fern K, et al. (2003) Care of the Patient with Hyperopia. American Optometric Association.
- Thibos LN, Horner D (2001) Power vector analysis of the optical outcome of refractive surgery. J Cataract Refract Surg 27(1): 80-85.
- Hirsch MJ (1961) A longitudinal study of refractive state of children during the first six years of school-a preliminary report of the Ojai study. Am J Optom Arch Am Acad Optom 38: 564-571.
- Matamoros E, Ingrand P, Pelen F, Bentaleb Y, Weber M, et al. (2015) Prevalence of Myopia in France: A Cross-Sectional Analysis Medicine (Baltimore) 94(45).
- Heidary G, Ying GS, Maguire MG, Young TL (2005) The association of astigmatism and spherical refractive error in a high myopia cohort. Optom Vis Sci 82(4): 244-247.
- Rezvan F, AbbasAli Yekta B, Hassan Hashemi B, Shiva Mehravaran B, Ostadimoghaddam H, et al. (2011) The Association between Astigmatism and Spherical Refractive Error in A Clinical Population. Iranian Journal of Ophthalmology 23(4): 37-42.
- Mandel Y, Stone RA, Zadok D (2010) Parameters Associated with the Different Astigmatism Axis Orientations. Invest Ophthalmol Vis Sci 51(2): 723-730.
- Farbrother JE, Welsby JW, Guggenheim JA (2004) Astigmatic axis is related to the level of spherical ametropia. Optom Vis Sci 81(1): 18-26.
- Gur S, Ron S, Heicklen-Klein A (1994) Objective evaluation of visual fatigue in VDU workers. Occup Med 44(4): 201-204.
- Elliott DB (2017) What is the appropriate gold standard test for refractive error? Ophthalmic Physiol Opt 37(2): 115-117.
- Allen PM, O Leary DJ (2006) Accommodation functions: Co-dependency and relationship to refractive error. Vision Res 46(4): 491-505.
- Rouse MW, London R, Allen DC (1982) An evaluation of the monocular estimate method of dynamic retinoscopy. Am J Optom Physiol Opt 59(3): 234-239.
- Wick B, Gall R, Yothers T (2002) Clinical testing of accommodative facility: part III. Masked assessment of the relation between visual symptoms and binocular test results in school children and adults. Optometry 73(3): 173-181.
- Lowery JP, Joachim A, Olson R, Peel J, Pearce NN (2005) Autorefraction vs. Retinoscopy: A comparison of non cycloplegic measures in a pediatric sample. J Behav Optom 16(1): 3-8.
- Sheppard AL, Davies LN (2010) Clinical evaluation of the Grand Seiko Auto Ref/Keratometer WAM-5500. Ophthalmic Physiol Opt 30(2): 143-151.
- Natarajan M, Sowbhagya H, Hemalatha B, Santosh P (2016) A novel method to screen and correct refractive errors in a camp scenario. Eur J Biomed Pharm Sci 3(4): 525-537.
- Mohindra I (1977) Comparison of near retinoscopy and subjective refraction in adults. Am J Optom Physiol Opt 54(5): 319-322.
- Williams KM, Verhoeven VJM, Cumberland P, Bertelsen G, Wolfram C, et al. (2015) Prevalence of refractive error in Europe: the European Eye Epidemiology (E(3)) Consortium. Eur J Epidemiol 30(4): 305-315.
- Muhamedagic L, Muhamedagic B, Halilovic EA, Halimic JA, Stankovic A, et al. (2014) Relation between near work and myopia progression in student population. Mater Sociomed 26(2): 100-103.