Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2644-1209
Review Article(ISSN: 2644-1209) 
Capsule Contraction Syndrome: Incidence, Pathogenesis, Prevention and Treatment Alternatives Volume 2 - Issue 2
Ayse Gul Kocak Altintas*
- University of Health Sciences, Turkey
Received:January 29, 2019; Published: February 07, 2019
Corresponding author: Ayse Gul Kocak Altintas, University of Health Sciences, Ankara Ulucanlar Eye Education and Research Hospital, Ankara, Turkey
DOI: 10.32474/TOOAJ.2019.02.000131
Abstract
Capsule contraction syndrome (CCS) is a rare but serious complication after cataract surgery. Several systemic and ocular factors such as Pseudoexfoliation syndrome, uveitis, high myopia, diabetes mellitus, advanced age, trauma, and previous vitreoretinal surgery promote capsular contraction. Surgical factors including small capsulorhexis size, IOL materials and design play an important role to development of CCS and IOL dislocation. Surgical enlargement of the anterior capsule can be performed in severe cases as an initial treatment or when the YAG capsulotomy is ineffective.
Keywords:Capsule contraction syndrome; Capsule shrinkage; Capsulectomy; YAG capsulotomy
Introduction
Capsule contraction syndrome (CCS) develops due to myofibroblastic metaplasia of the anterior cuboidal lens epithelia cells (LECs) and transformation to actine positive smooth muscle. This fibrotic change cause anterior capsular opacification (ACO) and capsular contraction that leads to significant shrinkage of both capsulectomy opening and equatorial capsular bag diameter. Progressive contraction of anterior myofibroblastic cells can cause imbalance between centrifugal and centripetal forces on the zonules which may results in malposition of the capsulectomy opening, angulation of the haptics or optic edges of IOL even the entire IOL. It may cause the capsular complex displacement or total IOL luxation into the vitreous cavity due to zonular dehiscence. ACO, the most innocent form of CCS without capsular bag shrinkage, obstructs peripheral retinal examination [1-3].
Incidence and Presenting Time
Even the peripheral ACO seen frequently after the phaco surgery the CCS presented with the reduction in the free optic zone and even complete occlusion of the capsulorhexis incision due to capsulorrhexis phimosis or IOL decantation is an uncomment complication. According to Zinkernagel et al. [4]. retrospective study the incidence of CCS was 1.5%, they observed 4 eyes with visually significant CCS out of 268 eyes. Tsinopoulos et al. [5] had been reported the insidence of CCS was 5%. They observed ACO with capsulorrhexis phimosis and IOL decentralization in eight eyes with a single-piece hydrophilic acrylic aspheric IOL out of 243 eyes, two to four months after surgery. The incidence of surgical intervention for repositioning or IOL exchange because of IOL dislocation was ranged between 0.2% and 3%. Mönestam et al. [6] reported 0.6% of the patients need reposition surgery for dislocated IOL 10 years after initial surgery.
CCS usually develops 3 to 6 months after phacoemulsification surgery as an reparation reaction of anterior capsule opening. Kumar et al. [7] reported two cases with the ages of 83 and 74 year has IOL dislocation within the bag 3 and 6 months after surgery, respectively.
Cochener et al. [8] reported that capsular shrinkage was faster at 30 to 150 days which shows slowly continuous progression 5 months after the surgery. Choi et al. [9] reported that the area of free optic zone of the anterior capsule significantly decreased from 1 week to 2 months postoperatively and further slowly but continuous reduction was observed from 2 months to 6 months in 236 eyes. According to their study the mean areas of the anterior capsule opening was 20.69±1.50 mm2 at 1 week which decreased to 17.17±3.23 mm2 at week 2, in a single-piece hydrophilic acrylic IOL which has a two-loop plate haptic at a 180° interval around the optic while free anterior optic zone was 21.43±1.09 mm2 at week 1, shrinked to 19.86±1.58 mm2 6 months after surgery in another type of hydrophilic acrylic IOL which has hydrophobic surface properties and a plate-shaped haptic. Their observation showed that the reduction was greatest in the first post-operative 2 months. But Coelho et al. [10] reported a 58-year-old patient with subluxation of the IOL, at postoperative third year. Long term observations of showed that CCS is a choronic progressive exaggerated reparative process of anterior capsule.
Pathogenesis
Prostoglandines, interleukins; IL-1 and IL-6, basic fibroblast growth factor, produced by residual lens epithelial cells (LES), increased in humor aqueous after cataract surgery that stimulate proliferation of cuboidal lens epithelial cells by alterations in cell to cell contact interactions. Transforming growth factor-βs (TGF- βs), is the key cytokine in developing scar formation in capsular opening, it elevates in the aques humor after surgery. TGF-βs upregulates TGF-βRII, the type II receptor for TGF-β2, expression in LECs which might play an important role in transdifferentiation of LECs into myofibroblasts [11-14].
Zhang et al. [12] observed shrunken membrane consisted of multiple layers of spindle-like LECs proliferation and excessive fibrous extracellular matrix in histopathological examination of contracted anterior capsule. Their study indicated that TGF-β2 concentrations in humor aques in high myopic eyes with CCS were higher than those without high myopia. Eyes had dense cataract had also higher TGF-β2 expression in aqueous humor after cataract surgery and it can increase the risk of CCS. According to their study eyes with high myopia and dense cataract have predisposition for CCS by increasing TGF-β2.
Risk Factors
Contraction of capsular opening due to myofibroblastic metaplasia, was strongly correlated with several ocular and systemic factors which either increased inflammatory reaction on anterior chamber or leading to instability of the blood-aqueous barrier such as diabetes mellitus, uveitis, retinitis pigmentosa. Zonular weakness due to advanced age, trauma, high myopia, certain connective tissue disorders and previous vitreo-retinal surgery are predispositing factors for IOL displacement in CCS. Pseudoexfoliation syndrome (PEX), has dual predisposition factor as increased anterior chamber inflammation by increased vascular permeability and has fragile zonules with weak stretching capability that cause zonular dehisces [2,3,7,9,13-16].
Surgical risk factors such as small capsulorhexis size, insufficient residual lens epithelial cells cleaning, increased surgical trauma, IOL design and materials play important role in the pathogenesis of CCS [2,16-21]. Weak adhesion between anterior capsule and IOL optic may allow space for active proliferation and migration of LECs. Increasing LECs exposure to several cytokines in the aqueous humor cause excessive synthesis of extracellular matrix, increase the fibrotic proliferation and finally anterior capsular shrinkage. IOL with hydrophobic acrylic optic material have shown stronger attachment to anterior capsule and by this way it prevents epithelial cells proliferation and migration on the optic surfaces. Hydrophilic optic have less adhesion to anterior capsule comparing to hydrophobic acrylic IOL and shown more frequent capsular phimosis than hydrophobic varieties [19,20]. IOL with silicone or hydrogel optics have the weakest anterior capsuler adhesion and shown the most frequent CCS. One-piece acrylic IOLs with sharpoptic edge prevents LES migration on the optic surfaces comparing to round-edge optics. On the other hand, Sacu et al. [21] reported that neither the material nor the haptic design of hydrophobic IOLs affected the development of CCS.
Prevention and Treatment
To prevent CCS, several preventing manipulation should be taken such as polishing of the posterior capsule, cortical material and anterior capsular epithelial cells removal as much as possible, careful attention should be paid to perform surgery with minimal trauma. Postoperative inflammation should be reducing with correct treatment. Close monitoring is essential for early diagnosis, because fibrotic contraction and malposition present with refractive error change and visual acuity detoriation [3,8,15,16].
CCS may initially present with pseudophakic lenticular astigmatism due to IOL folding or displacement of the optic or irregular astigmatism due to capsular opacification [22]. Page and Whitman [23] reported that patient’s refractive error shift of up to 1.0 D in either sphere or cylindrical, indicates the possibility of early capsular contraction that affecting the IOL position. They recommended neodymium yttrium–aluminum–garnet (Nd YAG) laser capsulotomy for preventing further contraction. Nd:YAG laser can create radial opening in the edge of capsular phimosis and perform significant circular enlargement, it can be effective in resolving the capsular synechiae of the haptics [24]. Deokule et al. [25] reported that the Nd YAG laser capsulotomy was successful in 78% cases out of 32 patient and failed in 7 cases (22.0%). They observed re-phimosis 5 cases and progressive IOL decentration in 2 cases. Kim et al. [26] reported a case underwent YAG anterior capasulotomy due to a total occlusion of the anterior capsulorhexis opening and the capsulotomy site remained clear 2 years after the treatment. In contrast Altintas et al. [27] reported a significant re-fimosis in case with Behçet ‘s disease, several months after Nd- YAG capsulotomy with prominent folding of both haptic and optic edge over the central part of IOL and they had to perform surgical capsulectomy for recalcitrant capsular closure.
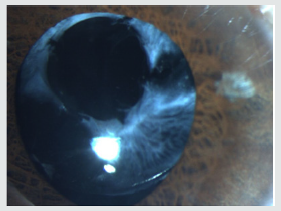
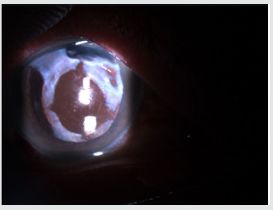
Wang et al. [28] presented a 63-year-old woman who had ciliary body detachment and secondary hypotony in both eyes caused by CCS, successfully treated with Nd: YAG laser. They reported that timely Nd: YAG laser anterior capsulotomy relaxes the contracted capsule, resolves the ciliary body detachment and prevents serious complications. Nd-YAG laser capsulotomy can prevent further capsular contraction in eyes with different IOL type in many cases (Figure 1a &1b & 2).
Figure 1a: Capsule contraction syndrome (CCS) in eyes with Capsule Tension Ring (CTR) before treatment.
Even the Nd: YAG capsulotomy is the first choice for capsular phimosis it may have several complications such as IOL pitting, anterior chamber inflammation and secondary glaucoma due to residual fibrotic material in the anterior chamber. Cystoid macular oedema may occur when the excessive laser energy was used mainly in thick membrane [29].
Gerten and coworker [30] and Schweitzer et al. [31] suggested femtosecond laser for capsulotomy extension that may offer advantages over the, Neodymium: YAG laser in CCS. Timothy et al. [32] reported that if the patient had a significant refractive change, such as more than 1.0 D of refractive spheric or astigmatic change, a YAG capsulotomy may not help for refractive correction or prevention of the further contraction. In this situation, they recommend surgical intervention such as a viscodissection and exiting of the fibrotic capsule. Surgical treatment can be performed as tangential cuts with the microscissors or manual extension of the capsulorhexis by oblique cutting with curved microscissors than peeling the fibrotic capsule. Excitation and enlarging the anterior capsule with vitrector are another choice to restore clear visual axis [33].
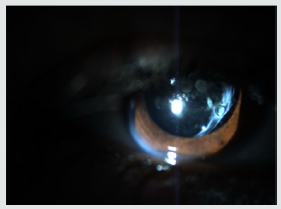
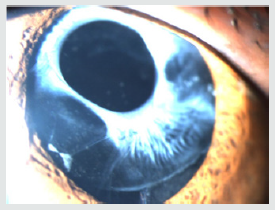
Page and Whitman [32] reported that insertion of a Capsule Tension Ring (CTR) could be most effective in correcting the IOL position and preventing further contraction in eyes with severe CCS. In contrast Altintas et al. [33] reported a case, age of 8 had ectopic lens and pupilla, developed CCS with significant reduction of total equatorial diameter of capsular bag, folding of both haptics over the optics and banding over each other both ends of CTR one year after cataract surgery even without posterior capsular opacification. According to their presentation CTR does not prevent development of CCS. Similarly, Sudhir et al. [34] and Moreno-Montañés et al. [35] reported capsulorhexis phimosis in eyes with endocapsular ring implantation. CTR may increase resistance to tractional force from capsular contraction, it does not always prevent capsular shrinkage. Furthermore Altintas et al. [36] reported three cases with PEX at the age of 72, 76, 79 who developed severe CCS and IOL subluxation with capsular tension ring (CTR) in the fibrotic capsular bag 3, 2.5 and 8 years after uneventful phacoemulsification respectively. This observation showed that CTR does not prevent IOL subluxation in long term follow up in eyes with the PEX (Figure 3).
Conclusion
Anterior capsule opening often contracts to some degree in most eyes underwent even uneventful phacoemulsification surgery with perfect continuous curvilinear capsulorrhexis. The degree of this contraction is related to several predictors such as surgical materials and manipulation or concurrent ocular risk factors. Close monitoring and early diagnosis of CCS is essential for timely treatment and prevention of severe complications such as complete anterior capsule contraction and IOL dislocation mainly in eyes with suspected zonular defect.
References
- Balestrazzi A, Malandrini A, Martone G, Marigliani D, Caporossi T, et al. (2014) Capsule Contraction Syndrome with a Microincision Foldable Hydrophilic Acrylic Intraocular Lens: Two Case Reports and Review of the Literature. Case Rep Ophthalmol 5(3): 329-335.
- Aose M, Matsushima H, Mukai K, Katsuki, Gotoh N, et al. (2014) Influence of intraocular lens implantation on anterior capsule contraction and posterior capsule opacification. Journal of Cataract & Refractive Surgery 40(12): 2128-2133.
- Altintas AG and Dal D (2010) Capsule contraction syndrome in Behcet’s disease. Int J Ophthalmol 3(4): 358-360.
- Zinkernagel M, Papazoglou A, Patel CK (2013) Bimanual anterior segment revision surgery for anterior capsule contraction syndrome associated with anterior flexion of intraocular lens haptics. Eye (Lond) 27(12): 1388-1390.
- Tsinopoulos IT, Tsaousis KT, Kymionis GD, Symeonidis C, Grentzelos MA, et al. (2010) Comparison of anterior capsule contraction between hydrophobic and hydrophilic intraocular lens models. Graefes Arch Clin Exp Ophthalmol 248(8): 1155-1158.
- Mönestam EI (2009) Incidence of dislocation of intraocular lenses and pseudophakodonesis 10 years after cataract surgery. Ophthalmology 116(12): 2315-2320.
- Kumar A, Freeman M, Kumar V, Ramanathan US (2008) In the bag IOL dislocation following uncomplicated phacoemulsification. Cont Lens Anterior Eye 31(2): 103-106.
- Cochener B, Jaccq PL, Colin J (1999) Capsule contraction after continuous curvilinear capsulorhexis: Poly (methyl methacrylate) versus silicone intraocular lenses. J Cataract Refract Surg 25 (10): 1362-1369.
- Choi M, Lazo MZ, Kang M, Lee J, Joo CK (2018) Effect of number and position of intraocular lens haptics on anterior capsule contraction: A randomized, prospective trial. BMC Ophthalmol 18(1): 78.
- Coelho RP, Zanatto MC, Paula JS, Romão E (2005) Spontaneous late inthe- bag intraocular lens dislocation after can-opener capsulotomy: case report. Arq Bras Oftalmol 68(6): 864-866.
- Zhu XJ, Chen MJ, Zhang KK, Yang J, Lu Y (2016) Elevated TGF-β2 level in aqueous humor of cataract patients with high myopia: Potential risk factor for capsule contraction syndrome. J Cataract Refract Surg 42(2): 232-238.
- Zhang K, Zhu X, Chen M, Sun X, Yang J, et al. (2016) Elevated Transforming Growth Factor-β2 in the Aqueous Humor: A Possible Explanation for High Rate of Capsular Contraction Syndrome in High Myopia. J Ophthalmol 2016: 5438676.
- Banh A, Deschamps PA, Gauldie J, Overbeek PA, Sivak JG, et al. (2006) Lens-specific expression of TGF-beta induces anterior subcapsular cataract formation in the absence of Smad3. Investigative Ophthalmology and Visual Science 47(8): 3450-3460.
- Hayashi Y, Kato S, Maeda T, Kaiya T, Kitano S (2005) Immunohistologic study of interleukin-1, transforming growth factor-β, and α-smooth muscle actin in lens epithelial cells in diabetic eyes. Journal of Cataract and Refractive Surgery 31(11): 2187-2192.
- Werner L, Pandey SK, Escobar-Gomez M, Visessook N, Peng Q, et al. (2000) Anterior capsule opacification: A histopathological study comparing different IOL styles. Ophthalmology 107(3): 463-471.
- Gao Y, Dang GF, Wang X, Duan L, Wu XY (2015) Influences of anterior capsule polishing on effective lens position after cataract surgery: A randomized controlled trial. Int J Clin Exp Med 8(8): 13769-13775.
- Kim SY, Yang JW, Lee YC, Kim SY (2013) Effect of haptic material and number of intraocular lens on anterior capsule contraction after cataract surgery. Korean J Ophthalmol 27(1): 7-11.
- Hayashi K, Hayashi H (2005) Comparison of the stability of 1-piece and 3-piece acrylic intraocular lenses in the lens capsule. J Cataract Refract Surg 31(2): 337-342.
- Tsinopoulos IT, Tsaousis KT, Kymionis GD, Symeonidis C, Grentzelos MA, et al. (2010) Comparison of anterior capsule contraction between hydrophobic and hydrophilic intraocular lens models. Graefes Arch Clin Exp Ophthalmol 248(8):1155-1158.
- Tsinopoulos I, Symeonidis C, Frangou E, Dimitrakos SA (2008) Capsule contraction syndrome in eight cases of hydrophobic one-piece intraocular lens implantation. Clin Exp Optom 91(5): 469-472.
- Sacu S, Menapace R, Findl O (2006) Effect of optic material and haptic design on anterior capsule opacification and capsulorrhexis contraction. Am J ophthalmol 141(3): 488-493.
- Zéboulon P, Gatinel D (2018) Unusual Internal Astigmatism Due to Severe Capsule Contraction Syndrome. J Refract Surg 34(1): 65-67.
- Page TP, Whitman J (2016) A stepwise approach for the management of capsular contraction syndrome in hinge-based accommodative intraocular lenses. Clin Ophthalmol 10: 1039-1046.
- Altintas AGK, Ilhan C (2018) Haptic Reposition with Laserposterior Capsulotomy in Eyes with Capsular Contraction without Anterior Capsular Phimosis. Madridge J Ophthalmol 3(1): 39-41.
- Deokule SP, Mukherjee SS, Chew CK (2006) Neodymium: YAG laser anterior capsulotomy for capsular contraction syndrome. Ophthalmic Surg Lasers Imaging 37(2): 99-105.
- Kim HD, Kim JM, Jung JJ (2017) Complete occlusion of anterior capsulorhexis after uneventful cataract surgery, treated with YAG laser capsulotomy. BMC Ophthalmol 17(1): 233.
- Altintas AGK, Dal D, Simsek S (2008) Significant intraocular lens folding due to severe capsular contraction. Jpn J Ophthalmol 52(2): 134-136.
- Wang W, Chen M, Wang Y, Yao K (2015) Bilateral capsule contraction syndrome-induced ciliary body detachment. Cataract Refract Surg 41(2): 468-470.
- Wesolosky JD, Tennant M, Rudnisky CJ (2017) Rate of retinal tear and detachment after neodymium: YAG capsulotomy. J Cataract Refract Surg 43(7): 923-928
- Gerten G, Schultz M, Oberheide U (2016) Treating capsule contraction syndrome with a femtosecond laser. J Cataract Refract Surg 42(9): 1255- 1261.
- Schweitzer C, Tellouck L, Gaboriau T, Leger F (2015) Anterior capsule contraction treated by femtosecond laser capsulotomy. J Refract Surg 31(3): 202-204.
- Page TP, Whitman J A (2016) Stepwise approach for the management of capsular contraction syndrome in hinge-based accommodative intraocular lenses. Clin Ophthalmol 10: 1039-1046.
- Altintas AGK, Ozcan PY, Koklu G (2014) Unusual features of developed capsule contraction syndrome in long term follw up period. Journal of Glaucoma-Cataract 9(3): 210-214.
- Sudhir RR and Rao SK (2001) Capsulorhexis phimosis in retinitis pigmentosa despite capsular tension ring implantation. J Cataract Refract Surg 27(10): 1691-1694.
- Moreno-Montañés J, Sánchez-Tocino H, Rodriguez-Conde R (2002) Complete anterior capsule contraction after phacoemulsification with acrylic intraocular lens and endocapsular ring implantation. J Cataract Refract Surg 28(4): 717-719.
- Altintas AGK, Omay AE,Celik S (2017) Spontaneous Late Intraocular lens and capsule tension ring dislocation. Turk J Ophthalmol 47(2): 106-109.