Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2644-1209
Case Report(ISSN: 2644-1209) 
Atypical Presentation of Ocular Toxoplasmosis with Exudative Retinal Detachment Volume 1 - Issue 3
Priyanka1* and Amber Kumar2
- 1MS, FMRF(Uvea), Sankara Nethralya, India
- 2Assistant Professor, AIIMS, India
Received: April 27, 2018; Published: May 03, 2018
Corresponding author: Priyanka, MS, FMRF (Uvea), Sankara Nethralya, Chennai
DOI: 10.32474/TOOAJ.2018.01.000112
Abstract
Subretinal fluid, a common clinical pathological entity, is seen in a variety of ocular disorders. Though inflammation is associated with the development of subretinal fluid, toxoplasmosis is an unusual causative agent. A 54 year old lady presented with atypical ocular findings of exudative retinal detachment due to toxoplasmosis. The diagnosis was misinterpreted first as sarcoidosis based on HRCT chest picture, later on diagnosed as ocular toxoplasmosis on correlating clinical presentation, fundus fluorescein angiography (FFA), optical coherence tomography (OCT) findings and serology. Patient was managed with a combination of oral anti Toxoplasma drugs, and oral corticosteroids.
Keywords: Subretinal fluid; Toxoplasma; optical coherence tomography
Abbreviation: OCT: Optical Coherence Tomography; FFA: Fluorescein Angiography; SRF: Sub Retinal Fluid; IVMP: Intravenous Methyl Prednisolone
Introduction
Toxoplasmosis is a common ophthalmic disorder and is said to cause a considerable number of cases of posterior ocular inflammation. Different investigators have considered toxoplasmosis to be the cause of 16-70% of cases of posterior uveitis [1,2]. Subretinal fluid (SRF) is a clinical finding. It is seen in a variety of eye diseases, with the list of associated ocular disorders growing as fluorescein angiography (FFA) has become more of a routine procedure for examining the posterior pole. The diagnosis of ocular toxoplasmosis can be made on the basis of clinical findings alone [3]. In the year 1969, Freidman and Knox [4] described the following three clinical presentations of active toxoplasmic retinochoroiditis (which occurs due to inflammatory response to activation of congenital toxoplasmosis [5]:
a) Large destructive active retinitis with associated vitritis (most common).
b) Punctate inner areas of retinitis with minimal associated edema and vitreous reaction.
c) Deep retinal punctate lesions with subretinal exudate (most unusual) associated with a minimal amount of vitreous reaction and with turbid subretinal fluid or blood
When these lesions heal, they lead to scars with an atrophic, “punched out” appearance and variable pigmentary changes. In 1969 Friedmann and Knox described an uncommon form of toxoplasmosis associated with macular subretinal fluid or blood [3]. Very few cases of toxoplasmosis have been reported with associated subretinal fluid, especially from India. We wish to add this case to the relatively small number of well documented instances of ocular toxoplasmosis presented with subretinal fluid.
Case report
A 54 year old female presented with complains of gradual and progressive diminution of vision in left eye for last 5 days. She had no history of uveitis or tuberculosis or contact with pets. She was hypertensive for last 4 year controlled on regular medications. On examination her best corrected visual acuity was 6/9 in right eye and 1/60 in left eye. Intraocular pressures were normal in both eyes. Anterior segment examination of both eyes and fundus in the right eye was unremarkable. Fundus of the left eye revealed disc edema, vitritis with massive subretinal fluid (SRF). Left eye OCT showed subfoveal fibrin with retinal thickening. SRF noted inferior and nasal to fovea and inferior to disc. Foveal thickness of left eye revealed 756 micron and of right eye 165 micron. FFA revealed disc leakage and pooling of dye temporal to disc of left eye in late phase. HRCT chest revealed few nodular lesion and fibrobronchiectatic changes with calcific foci in both lung fields with negative mantoux test and negative sputum for acid fast bacilli. This case was misinterpreted first as sarcoidosis although ACE level was normal and was prescribed intravenous methyl prednisolone (IVMP) for 3 consecutive days followed by oral steroid. There was no improvement in vision and OCT showed same degree of disc edema and subretinal fluid even after 3 days of IVMP (Figures 1 & 2).
Figure 1: Fundus photo: Right eye unremarkable. Left eye showing disc edema , vitritis and massive subretinal fluid involving macula FFA : Left eye revealing disc leakage with pooling of dye in late phase. OCT: Left eye OCT revealing subfoveal fibrin with retinal thickening. SRF inferior and nasal to fovea and inferior to disc. Foveal thickness in left eye was 756 micron and 165 micron in right eye.
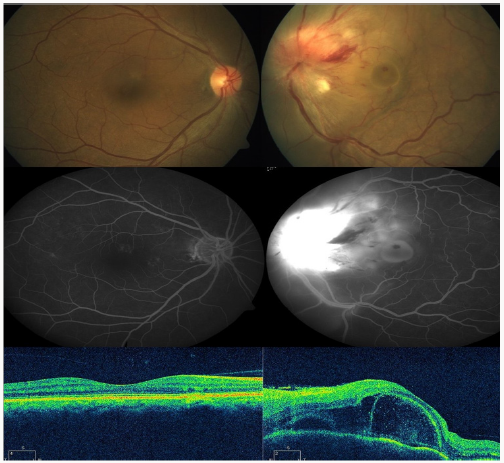
Figure 2: Fundus photo: Left eye showing normal optic disc with reduced SRF FFA: Left Eye showing disc staining and scar temporal to disc in late phase OCT: Left eye showing minimal subretinal fibrin, SRF and retinal thickening. Foveal thickness of left eye decreased to 314 micron.
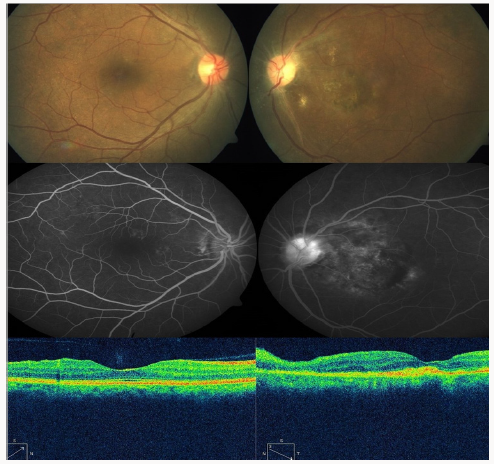
Patient was further revaluated for other causes. IgM antitoxoplasma was positive and IgG was negative, suggestive of recent infection. Based on the clinical presentation, fundus fluorescein angiography, OCT, and positive serology, the patient was diagnosed as atypical ocular toxoplasmosis with exudative retinal detachment. The patient was managed with sulfamethoxazole (800 mg) & trimethoprim (160 mg) tablet twice daily and tab clindamycin tablet 300 mg 4 times daily for 6 weeks along with tapering of oral prednisolone. At 4 week follow up she showed improvement in OCT and FFA findings with restoration of visual acuity to 6/24 in left eye. OCT showed decrease in subretinal fibrin, SRF and retinal thickening. Foveal thickness of left eye decreased to 314 micron. On regular follow up for next 2 year no residual or recurrence of retinochoroiditis was noted.
Discussion
Exudative retinal detachment is often under diagnosed in ocular toxoplasmosis. This case was an atypical presentation of ocular toxoplasmosis with exudative retinal detachment based on the presence of subretinal fluid and misinterpreted as sarcoidosis. HRCT chest findings of few nodular lesion and fibrobronchiectatic changes with calcific foci in both lung fields were old healed lesion, but patient had no flare up of lung infection on follow up. In this case positive serology for toxoplasma and response to treatment confirmed the diagnosis.
References
- Schlaegel TF (1979) Toxoplasmosis. In: Duane TD, ed. Clincal Ophthalmology. Hagerstown: Harper and Row 4: 1-16.
- Cassady JV (1960) Toxoplasmic retinochoroiditis. Trans Am Ophthalmol Soc 58: 392-431.
- Noble KG, Carr RE (1982) Toxoplasma retinochoroiditis. Ophthalmology 89: 1289-1290.
- Friedmann CT, Knox DL (1969) Variations in recurrent active toxoplasmic retinochoroiditis. Arch Ophthalmol 81: 481-493.
- Desmonts G, Couvreur J (1974) Toxoplasmosis in pregnancy and its transmission to the fetus. Bull N Y Acad Med 50(2): 146-159.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...