Lupine Publishers Group
Lupine Publishers
Review ArticleOpen Access
Anterior Scleritis Volume 3 - Issue 5
Priyanka*, Mansi Kishnani, Ulka Srivastava and Shubhangi Dubey
- Department of Ophthalmology, Chirayu medical college and hospital, Bhopal, India
Received:February 20, 2023; Published:March 03, 2023
Corresponding author: Priyanka, Department of Ophthalmology, Chirayu medical college and hospital, Bhopal, India
DOI: 10.32474/TOOAJ.2023.03.000175
Abstract
Scleritis refers to chronic painful inflammatory diseases of the sclera that can also involve cornea and underlying uveal tract. Pathogenic mechanisms in scleritis are poorly understood, but enzymatic degradation of collagen fibrils by infiltrating leukocytes seems to be a key feature. Although a majority of these cases are immune mediated and at least half of these are associated with underlying systemic illnesses. About 5-10 % of cases are due to infectious causes. Infectious scleritis is often initially managed as autoimmune due to the similarity of its presentation leading to poor outcome. Careful clinical history taking, detailed ocular examination, appropriate investigation and timely intervention has improved the long-term outcome for patients with this disease.
Introduction
Scleritis refers to a heterogeneous group of diseases characterized by inflammation of the sclera, which may also involve the adjacent episcleral, cornea and underlying uveal tract [1]. It is associated with significant ophthalmic and systemic morbidity if not appropriately diagnosed and treated leading to the progressive destruction of the eye and other associated ophthalmic complications [2]. The presence of scleritis can be the initial manifestation of a potentially lethal systemic vasculitis or only sign of active systemic disease of an already diagnosed inflammatory disorder [3]. Women are more commonly affected than men, with a peak incidence in the fifth decade. Symptoms may include tearing, photophobia, and pain on accommodation. Infection is an important but rare cause of the scleritis, occurring in about 5–10% of all cases [4]. Geographical location should be considered, as infectious scleritis is more commonly seen in the southern area of the United States [5]. However, infectious scleritis is often initially managed as autoimmune due to the similarity of its presentation, potentially worsening its outcome. Anterior scleritis remains a therapeutic challenge for ophthalmologists. The improved diagnosis of underlying systemic autoimmune conditions and advent of more potent immunosuppressive agents have produced more effective treatments for scleritis, thereby limiting both ocular and systemic morbidity.
Etiology And Pathogenesis
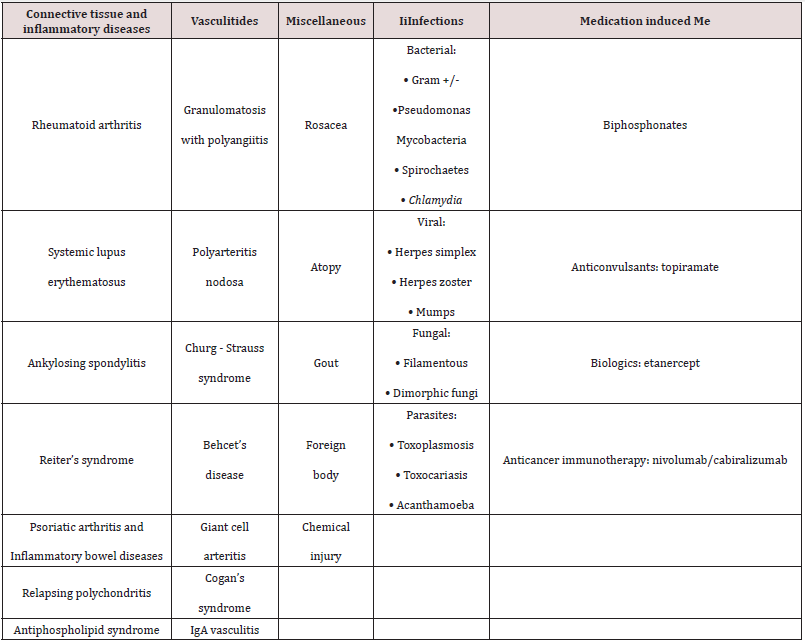
The various classification is based mainly on the clinical appearance, etiology and anatomical location. The earliest classification was proposed by Watson and Hayreh . More recently, Sen et al. reclassified the disease based on standardized digital photographs [6]. Around 15–59% of patients may present with scleritis as the first manifestation of a systemic immune mediated disease [7-9]. Rheumatoid arthritis (RA) and granulomatosis with polyangiitis (GPA) are the most common among them [10]. Various studies from Western literature report 5‑10% incidence of infectious etiology as compared to about 17% in the Indian study [11,12].The prevalence of infectious etiology correlate with the geographical location and livelihood patterns of the population. In developing countries with agriculture as the major occupation, microbial scleritis has a higher incidence due to increased rate of trauma [13]. To differentiate infectious scleritis with autoimmune scleritis is a challenge for the ophthalmologist without relevant laboratory investigations due to similarity in initial presentation. Among 50-60 % of patients have underlying diseases including immune‑mediated disease, medication‑induced as well as miscellaneous entities (Table 1). The pathology and pathogenesis of scleritis are multifactorial and complex. In infectious scleritis, replicating organisms directly invade leading to the destruction of the tissue and immune reactions triggered by the infective agent [14]. In autoimmune disorders, a hypersensitivity reaction is generated against autoantigens leading to cellular immunological attack against healthy tissue and vessels. This results in the activation of local mechanisms leading to the degradation of proteoglycans and collagen, which eventually results in the thinning and loss of scleral tissue [15,16] An imbalance between levels of collagen-degrading matrix metalloproteinases and tissue inhibitors of matrix metalloproteinases is likely to contribute to the process of degradation [17]. In non‑infectious scleritis, scleral biopsy is rarely indicated for diagnostic purposes as it might worsen the inflammation and threaten the stability of the globe.
Clinical Features
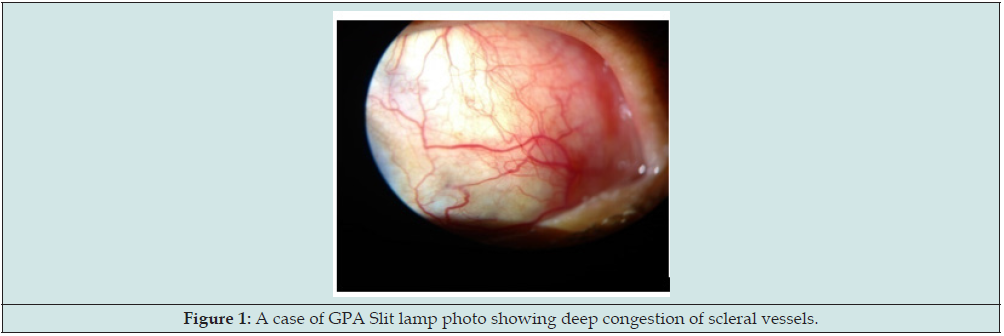
Clinical signs and symptoms at presentation are variable depending on the degree and site of inflammation. Scleritis occurs more commonly anterior to the equator due to more abundant anterior vascular supply. Anterior scleritis is a sight-threatening eye disease, characterized by acute or chronic red eye and insidious, deep, boring pain that localizes to the sclera but is often referred to the temple and jaw. [18,19].Watson and Hayreh classification is useful in determining the severity of the inflammation and as a guide for further treatment. Anterior scleritis can be divided into diffuse, nodular, necrotizing and necrotizing without inflammation (scleromalacia perforans). The inflammation of diffuse scleritis is generalized with insidious onset . Upon resolution the sclera may look bluish due to rearrangement of the collagen fibrils without thinning. About 45% of patients with anterior diffuse scleritis and 40–50% with nodular scleritis will have an associated disease, RA being the most common [20-22]. Uveal tissue may appear due to thin and translucent overlying sclera and need careful monitoring to see progression to necrotizing scleritis. Necrotizing scleritis is the most severe form of scleritis with significant ocular morbidity and also sign of the onset of potential lethal systemic vasculitis. 60–90% patients have an underlying systemic disease, most common granulomatosis with polyangiitis[GPA](Figure 1) and RA. The damaged sclera will become translucent due to thinning, leaving the choroid covered by conjunctiva or residual thinned scleral tissue. The protrusion of choroid can occur with trauma or increased intraocular pressure. Scleromalacia perforans is almost always seen in patients with long-standing RA. The scleral tissue changes colour from white to yellow and becomes absorbed and disintegrated, leading to exposure of the underlying choroid [23]. Necrotizing scleritis is the most common presentation of infectious scleritis, with yellowish or reddish hue of the nodule due to underlying suppuration. Fibrous tissue band with scleral thinning indicate previous infectious etiology, unlike immune lesions which heal with only scleral thinning. An initial apparent response followed by subsequent worsening when the patient has been started on immunosuppressants alone especially topical corticosteroids should alert the clinician to the possibility of an infectious etiology [24,25]. The lack of improvement with immunosuppressants and resolution only on starting antiviral therapy, presence of corneal scars are clinical indicators for viral disease. Tuberculous scleritis may be the result either of a direct MTB scleral invasion but more often is caused by an immune mediated process [26-29]. Diagnosis of tuberculous scleritis requires scleral biopsy. The patient should be thoroughly investigated to look for primary focus with Mantoux test, sputum examination and high resolution chest CT. The infection can originate either from exogenously by trauma or ocular surgeries, or endogenously in immunocompromised via intravenous drug use. Debilitating ocular or systemic diseases, contact lens use, intravenous narcotic addiction, and chronic topical corticosteroid use increase the risk of fungal infection. In all cases of suspected fungal scleritis, microbiological diagnosis should be made before starting therapy. Often, multiple biopsies are required to reach to the diagnosis. Visual prognosis in fungal scleritis is often poor because of delayed diagnosis, poor penetration of the available antifungal’s agents into the avascular sclera and non-availability of fungicidal agents.
Diagnosis
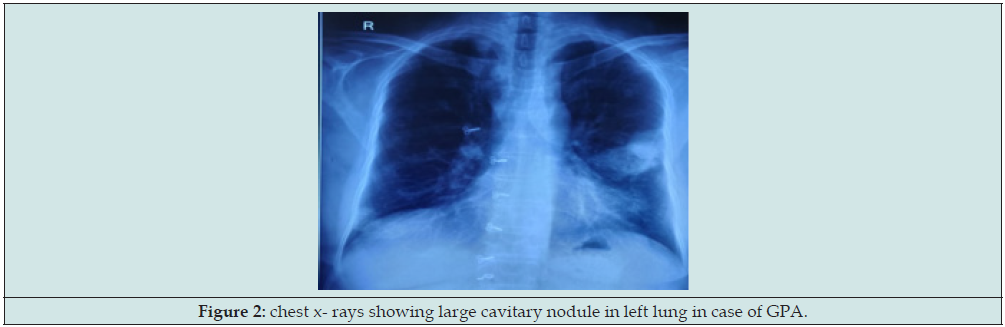
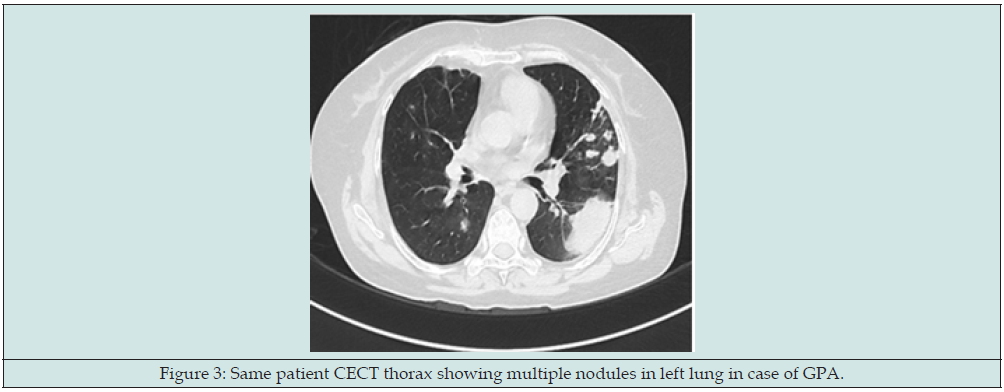
Scleritis presents with a characteristic violet-bluish hue with scleral edema and dilatation. On slit-lamp biomicroscope, inflamed scleral vessels often have a criss-crossed pattern and cannot be moved with a cotton-tipped applicator, which differentiates from more superficial episcleral vessels. The conjunctival and superficial vessels may blanch with 2.5-10% phenylephrine but deep vessels are not affected. The evaluation of a patient with scleritis requires a systemic evaluation with a thorough medical history, in addition to a full ophthalmic examination. Infectious etiologies also should be considered with history of trauma or surgical insult. Approximately 50–60% of patients with scleritis will have an underlying associated disease . Of these, 50% will be an autoimmune connective tissue or vasculitic disease. Therefore, early diagnosis and treatment is critical. Complete rheumatologic examination including joints, skin, cardiovascular, respiratory and renal systems, can be critical. Obtaining a chest x-ray for evidence of GPA (Figures 2 & 3), tuberculosis, or sarcoidosis is important as a first line evaluation. Antineutrophil cytoplasmic antibody testing is essential for evaluating Wegener granulomatosis. A positive c-ANCA in a patient with scleritis is specific for Wegener granulomatosis [30,31]. Serology for syphilis (rapid plasma reagin) [RPR] and rheumatoid factor for rheumatoid arthritis and antinuclear antibody suggestive of SLE, rheumatoid arthritis should also be performed routinely. Erythrocyte sedimentation rate in patients with suspected giant cell arteritis; angiotensin-converting enzyme and lysozyme levels for sarcoidosis; and HLA-B27 for patients with suspected ankylosing spondylitis, may be helpful. In cases of suspected infectious scleritis, conjunctival scrapings and serology for herpes viruses are performed [32]. In cases where there is adjoining keratitis or an ulcerated scleral nodule with visible slough or plaque at the base of the ulcer, samples for microbiology can be taken by corneal or scleral scrapings for collection and inoculation of the purulent material. Specimens obtained from cornea, conjunctiva and episclera should be stained for Grams, Giemsa and 1% acid fast staining along with cultures on blood, chocolate and Sabouraud’s dextrose agar. Scleral or sclerocorneal biopsy is advised if smears and cultures of scrapings are negative after 48 hours and there is no clinical response or patient is not improving on the initial broad‑spectrum antimicrobial therapy.
Management
The primary aim of the treatment of scleral inflammation is to control the inflammatory process to relieve the symptoms. However, the effective management of a case of scleral inflammation involves timely diagnosis, identification of underlying systemic or local cause, if any and prevention of complications. The most commonly used treatment strategy for non-infectious anterior scleritis was outlined recently by Jabs et al.[33] The first line of treatment for no necrotizing anterior scleritis is topical administration of corticosteroids and oral nonsteroidal anti-inflammatory agent. Patients with necrotizing and no necrotizing scleritis not responding to NSAIDs should be started on oral prednisone at 1 mg/kg/d. Intravenous corticosteroids are sometimes needed as in cases with threatened scleral or corneal perforation in necrotizing scleritis. It is mandatory to rule out any infective etiology before commencement of therapy. Immunosuppressive agents are also used if inflammation recurs during prednisone taper at doses too high for long-term treatment, if significant side effects are incurred during prednisone therapy, or if a systemic condition requires immunosuppressive agents. Necrotizing scleritis, particularly associated with autoimmune diseases almost always requires systemic immunosuppressive therapy, not only for ocular involvement, also for life threatening systemic complications. Various immunosuppressants have been tried for treatment of scleritis and these include antimetabolites (methotrexate, azathioprine, and mycophenolate mofetil), alkylating agents (chlorambucil and cyclophosphamide), T-cell inhibitors (cyclosporine and tacrolimus). Methotrexate has the most widespread usage due to its relatively safe profile dosage.
Treatment of scleritis associated with necrotizing systemic vasculitis should be prompt and effective. Treatment in such patients should be guided both by the ophthalmic response and control of the underlying disease. Tectonic surgical procedures rarely may be required to preserve the integrity of the globe. Patch grafts might need to be performed along with systemic immunosuppression in cases of extensive scleral melts and uveal show. Management of infectious scleritis remains challenging, with approximately 60% of the eyes with infectious keratoscleritis resulting in complete loss of vision or removal of the eye, largely due to poor penetration of antibiotics into the nearly avascular sclera [34]. While awaiting microbiological results, broad spectrum fortified antimicrobial therapy, covering both Gram positive and Gram negative organisms should be started and the therapy should be modified based on the initial smear results and subsequent culture and sensitivity results. If microorganisms are not isolated despite repeated testing, and histopathological study reveals an inflammatory picture, autoimmune scleritis must be suspected, and therapy with oral corticosteroids, immunosuppressive, or biologics should be considered under antibiotic coverage as a last resort. Numerous management options have been described including topical fortified antibiotics, subconjunctival antibiotics, cryotherapy, lamellar or penetrating corneoscleral graft, and subpalpebral irrigation to allow for continuous delivery of highly concentrated antibiotics [35]. Indications for surgery in either infectious or autoimmune scleritis include biopsy for suspected infectious scleritis, repair of corneal and scleral defects, repair of globe perforation, and repair of uveal prolapse with impending perforation in necrotizing scleritis. In cases of severe scleral necrosis, rapid progression or with multifocal abscesses not responding to medical treatment, surgical debridement of scleral abscess and irrigation with either 2.5% betadine solution or with broad spectrum antibiotics or antifungals such as 2% voriconazole has been recommended. These measure help in reducing necrotic tissue and the infective load, thereby increasing drug penetration. The overall visual outcome in infectious scleritis is generally worse than autoimmune probably due to delay in diagnosis or aggressive nature of associated microbes.
Conclusion
Scleritis refers to a heterogeneous group of diseases which is associated with significant ophthalmic and systemic morbidity. Systemic and/or local immunosuppression in cases of autoimmune anterior scleritis results in decreased pain and fewer visually significant complications such as keratitis, uveitis and glaucoma. Proper diagnosis and appropriate immunosuppression may prove to be life saving for patients with underlying autoimmune disease. Although anterior scleritis is often a chronic disease, prompt diagnosis in collaboration with rheumatologists reduces ocular and systemic morbidity. Subconjunctival corticosteroid therapy for nonnecrotizing autoimmune scleritis and continuous subpalpebral antibiotic irrigation for infectious scleritis are promising therapies that require further study. History of trauma or recent surgery with subsequent nodular and ulcerative type of scleritis will be easy to diagnose as infectious scleritis. However, there is diagnostic dilemmas for those case where the clinical picture is equivocal or there is no antecedent history in favour of either diagnosis. In these instances, subtle signs and response to therapy need to be used for definite diagnosis regarding the etiology of the scleritis. The two conditions infectious and inflammatory scleritis closely mimic each other and a thorough knowledge of the subtle differences is necessary in order to reach a timely diagnosis. Diagnostic delay can lead to a poor outcome either due to the destruction caused by the uncontrolled infection or due to propagation of the infection with the use of corticosteroids which may have been started for presumed immune mediated scleritis.
References
- Okhravi N, Odufuwa B, McCluskey P, Lightman S (2005) Scleritis, Surv Ophthalmol 50(4): 351-363.
- Watson PG, Hayreh SS (1976) Scleritis and episcleritis, Br J Ophthalmol 60(3): 163-167.
- Foster CS, Forstot SL, Wilson LA (1984) Mortality rate in rheumatoid arthritis patients developing necrotizing scleritis or peripheral ulcerative keratitis, Ophthalmology 91(10): 1253.
- Jain V, Garg P, Sharma S (2009) Microbial scleritis-experience from a developing country Eye 23(2): 255-261.
- Hodson K, Galor A, Karp K, et al. (2013) Epidemiology and visual outcomes in patients with infectious scleritis, Cornea 32(4): 466-472.
- Sen HN, Sangave AA, Goldstein DA, Suhler EB, Cunningham D, et al. (2011) A standardized grading system for scleritis. Ophthalmology 118(4): 768-7671.
- Sainz de la Maza M, Molina N, Gonzalez‑Gonzalez LA, Doctor PP, Tauber J, et al. (2012). Clinical characteristics of a large cohort of patients with scleritis and episcleritis. Ophthalmology 119(1): 43-50.
- Sainz de la Maza M, Foster CS, Jabbur NS (1995) Scleritis associated with systemic vasculitic diseases. Ophthalmology 102(4): 687-692.
- Gu J, Zhou S, Ding R, Aizezi W, Jiang A, ET AL (2013) Necrotizing scleritis and peripheral ulcerative keratitis associated with Wegener’s granulomatosis. Ophthalmol Ther 2(2): 99-111.
- Sainz de la Maza M, Tauber J, Foster CS (2012) The Sclera. Springer‑Verlag, New York, USA.
- Ho YF, Yeh LK, Tan HY, Chen HC, Yeong‑Fong, et al. (2014) Infectious scleritis in Taiwan—A 10‑year review in a tertiary‑care hospital. Cornea 33(8): 838-843.
- Sainz de la Maza M, Jabbur NS, Foster CS (1994) Severity of scleritis and episcleritis. Ophthalmology 101(2) :389-96.
- Jain V, Garg P, Sharma S (2009) Microbial scleritis: Experience from a developing country. Eye 23(2): 255-261.
- Ramenaden ER, Raiji VR (2013) Clinical characteristics and visual outcomes in infectious scleritis: A review. Clin Ophthalmol 7: 2113‑21
- Wakefield D, Di Girolamo N, Thurau S, et al., (2013) Scleritis: Immunopathogenesis and molecular basis for therapy, Progress in Retinal and Eye Research 35: 44-62.
- Young RD and Watson PG (1984) Microscopical studies of necrotising scleritis. II. Collagen degradation in the scleral stroma. Br J Ophthalmol 68(11): 781-789.
- Di Girolamo N (1997) Increased expression of matrix metalloproteinases in vivo in scleritis tissue and in vitro in cultured human scleral fibroblasts. Am J Pathol 150(2): 653-666.
- Watson PG, Hayreh SS (1976) Scleritis and episcleritis. Br J Ophthalmol 60(3): 163-191.
- Watson PG (1974) Treatment of scleritis and episcleritis. Trans Ophthalmol Soc UK 94: 76-79.
- Jabs DA, Mudun A, Dunn JP, Marsh MJ (2000) Episcleritis and scleritis: clinical features and treatment results, Am J Ophthalmol 130(4): 469-476.
- Sainz M, Molina N, Gonzalez LA, Joseph Tauber, C Stephen Foster, et al. (2012) Clinical characteristics of a large cohort of patients with scleritis and episcleritis, Ophthalmology 119(1): 43-50.
- Hakin KN, Watson PG (1991) Systemic associations of scleritis, Int Ophthalmol Clin 31: 111-129.
- Sainz de la Maza M, Tauber J, Foster CS (2012) Clinical considerations of episcleritis and scleritis. In: Sainz de la Maza M, Tauber J, Foster CS, The Sclera, Second Edition, New York: Springer 102-132.
- Murthy SI, Reddy JC, Sharma S, Sangwan VS (2015) Infectious Scleritis. Curr Ophthalmol Rep 3(3): 147‑1
- Gonzalez LAG, Molina‑Prat N, Doctor P, Tauber J, Sainz de la, et al. (2012) Clinical features and presentation of infectious scleritis from herpes viruses: A report of 35 cases. Ophthalmology 119(7): 1460-1464.
- Lane J, Nyugen E, Lim L, Stawell R, Hodgson L, et al. (2019) Clinical features of scleritis across the Asia‑Pacific region. Ocular Immunol Inflamm 27(6): 920-926.
- Bloomfield SE, Mondino B, Gray GF (1976) Scleral tuberculosis. Arch Ophthalmol 94(6): 954-956.
- Agarwal A, Majumder PD (2019) Tubercular posterior scleritis: A case report and review of literature. Indian J Ophthalmol 67(8): 1362‑136
- Murugan SB (2019) Commentary: Tubercular posterior scleritis‑Nuances in practice! Indian J Ophthalmol 67(8): 1366‑136
- Soukiasian SH, Foster CS, Niles JL (1992) Diagnostic value of anti-neutrophil cytoplasmic antibodies in scleritis associated with Wegener’s granulomatosis. Ophthalmology 99(1): 125-132.
- Akpek EK, Thorne JE, Qazi FA (2004) Evaluation of patients with scleritis for systemic disease. Ophthalmology 111(3): 501-506.
- Barr CC, Davis H, Culbertson WW (1981) Rheumatoid scleritis. Ophthalmology 88(12): 1269-1273.
- Jabs DA, Mudun A, Dunn J (2000) Episcleritis and scleritis: clinical features and treatment results. Am J Ophthalmol 130(4): 469-476.
- Reynolds MG, Alfonso E (1991) Treatment of infectious scleritis and keratoscleritis. Am J Ophthalmol 112(2): 543-547.
- Hessburg PC (1982) Pseudomonas corneoscleral ulcers. Am J Ophthalmol 93(2): 256-257.