Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6695
Research Article(ISSN: 2637-6695) 
The Implications for Nursing Care of Frail Elderly with Limited Self-Management Abilities: A Cross-Sectional Study in the Netherlandsc Volume 3 - Issue 1
Petra Boersma, Anne Marie Vaalburg, Marjolein Albers, Carin JM de Boer, Robbert JJ Gobbens*
- Faculty of Health, Sports and Social Work, Inholland University of Applied Sciences, Amsterdam, The Netherlands
Received: April 12, 2021; Published: April 27, 2021
Corresponding author: Robbert JJ Gobbens, Zonnehuisgroep Amstelland, Amstelveen, The Netherlands Department Family Medicine and Population Health, Faculty of Medicine and Health Sciences, University of Antwerp, Antwerp, Belgium
DOI: 10.32474/LOJNHC.2021.03.000153
Abstract
Aim: To gain insight into the relationship between self-management abilities (taking initiatives, investment behaviour, variety, multifunctionality, self-efficacy, positive frame of mind) and physical, psychological and social frailty. Design: A cross-sectional study.
Methods: 145 community-dwelling older people receiving home care completed a questionnaire on sociodemographic factors, the Self-Management-Ability-Scale and the Tilburg Frailty Indicator. After determining correlations, sequential multiple linear regression analyses were executed.
Results: All self-management abilities are negatively associated with physical frailty; five (except multifunctionality) are negatively associated with psychological frailty. Variety in resources and positive frame of mind are negatively associated with social frailty. Sociodemographic characteristics, chronic diseases and self-management abilities together significantly explain participants’ physical (34.9%), psychological (21.4%) and social (43.9%) frailty. After controlling for sociodemographic characteristics and chronic diseases, the self-management abilities together significantly explain 11 per cent of psychological and 6.8 per cent of social frailty. Having a positive frame of mind significantly negatively influences social frailty.
Keywords:Nursing, Frailty; Older People; Self-Management; Community Care
Introduction
Population aging is occurring throughout the world [1]. A risk of getting older is becoming frail, which implies vulnerability [2]. Currently, there is a wide variety of conceptual definitions of frailty; in addition, no universally accepted operational definition of the concept of frailty exists [3]. On the one hand, frailty is operationalized narrowly, focusing mainly on the physical domain - e.g., the phenotype of frailty [4], the FRAIL scale [5]. On the other hand, there are broader operational definitions of frailty, including the psychosocial domain, such as the Frailty Index [6], the Edmonton Frail Scale [7], and the Tilburg Frailty Indicator (TFI) [8]. The prevalence of frailty is common in later life, and women are more sensitive to frailty than men [2]. Due to the different operational definitions of frailty [2] found that the prevalence of frailty differs widely between studies. Previous studies have shown that frail older people have a higher risk of disability [9], falls [4], hospitalization [4], institutionalization [10], lower quality of life (Kojima et al., 2016) and mortality (Vermeiren et al., 2016) compared to non-frail older people. It is therefore important to prevent older people from becoming frail. In order to achieve this goal, a good understanding of the determinants of frailty is necessary. Besides greater age and sex (women), well-known determinants of frailty are chronic diseases, low socio-economic status, and having a bad lifestyle (e.g. sedentary behaviour) [11]. Another possible determinant is the extent to which an older person has self-management abilities. Self-management is an ongoing process to cope and live with a chronic disease [12]. Self-management aims to help these individuals to maintain wellness in their foreground perspective instead of disease [13]. As in many other countries in the world, the population of older people is also growing in the Netherlands [1]. Moreover, the number of frail older people aged 65 years or older is forecast to grow from 700,000 in 2010 to more than a million in 2030 [14]. In the Netherlands, the community nurse has an important task in caring for and supporting frail elderly. The ageing population, leading to increased pressure on the healthcare system and a shifting view on healthcare, has led to a revival of nurses’ role and position in the community: supporting older people to live independently and participate in society as actively as possible is being emphasized. In this way, nurses aim to ensure that elderly maintain a certain level of wellbeing, and by focusing on prevention and care and treatment at home, medical costs are avoided. To achieve this, nursing care should be provided from a holistic perspective, and adopting a multidimensional definition of frailty, including interventions supporting self-management in the elderly, is needed in the community. A longitudinal study by [15] among 111 community-dwelling elderly showed that investing in community health nurses may be beneficial for both their self-management abilities and their quality of life. However, knowledge about how to improve the self-management abilities of frail elderly in the community is lacking [15]. According to [16], four perspectives of nurses on self-management support can be distinguished, seen from both the viewpoint of dependent elderly and nurses: the coaching, clinician, gatekeeper and educator perspectives. These perspectives can support nurses to encourage self-management abilities in their frail elderly patients.
Evidence on the associations between the self-management abilities of community-dwelling elderly and multidimensional frailty is lacking. There are only a few studies available using the concepts of both self-management and frailty. One of these was conducted by [16], whose cross-sectional study consisted of 869 elderly aged 70 years or older living in Rotterdam, the Netherlands. For measuring self-management abilities and frailty, the short version of the Self-Management Ability Scale (SMAS-S) [17] and the TFI [8] (Gobbens et al., 2010b) were used, respectively. [18] demonstrated that self-management and frailty were associated with poor health (p<0.05), adjusted for age, sex, marital status and education. An earlier study among 99 patients (≥ 65 years) recruited from wards of the University Hospital Groningen and a family practitioner’s practice showed that frailty, assessed with the Groningen Frailty Indicator (GFI) [20], and self-management, assessed with the Self-Management Ability Scale (SMAS-30) [21], were associated with wellbeing [20]. Knowledge about the associations between self-management abilities in older people and their frailty (physical, psychological, social) can help specify the nature of community nurses’ tasks in terms of intervening in self-management abilities aiming to prevent or delay the onset of frailty.
Research Question
The aim of this study is to gain more insight into the relationship between self-management in community-dwelling older people and frailty. The corresponding research question is: What are the associations between the six abilities of self-management (taking initiatives, investment behaviour, variety, multifunctionality, selfefficacy, positive frame of mind) and the three frailty domains (physical, psychological, social)?
Design and Methods
Design
For this study a cross-sectional design was used.
Participants
All community-dwelling people who received homecare from Amstelland Thuiszorg at that time were asked to participate in this study. No specific selection criteria were used. Data were gathered by a written questionnaire containing questions regarding sociodemographic factors, the SMAS-30 for measuring self-management and the TFI for measuring frailty. Approximate 600 persons receiving home care were asked to fill in the questionnaire and 145 persons did so (24.2%). The community nurses were asked the participants to fill in the questionnaire and to help people who were not able fill in the forms.
Data Collection
This data was collected in October 2015. The questionnaire contained two measures: The Self-Management Ability Scale (SMAS- 30, version 2) for assessing management abilities, and the Tilburg Frailty Indicator (TFI) for assessing multidimensional frailty. Also, questions referring to chronic diseases and sociodemographic characteristics of the participants were asked.
Self-Management Ability Scale (SMAS-30 version 2)
Self-management abilities were measured using the SMAS-30. The SMAS-30, version [22] is based on the self-management of wellbeing (SMW) theory [23] and developed to measure six selfmanagement abilities which are important for elderly people when they pursue successful ageing even when their resources decline [21]. The six core self-management abilities are: 1) the ability to ensure multifunctionality of resources; 2) the ability to maintain variety in resources; 3) the ability to keep a positive frame of mind; 4) the ability to invest in resources for longer term benefits; 5) the ability to be self-efficacious with regard to managing resources; and 6) the ability to take the initiative. These six abilities, according to the social production functions (SPF) theory, are related to the dimensions of comfort, stimulation for physical wellbeing, affection, behavioural confirmation and status for social wellbeing [24]. The SMAS-30 consists of 30 items; each core self-management ability contains 5 items. Each item is answered on a Likert scale ranging from 1 (never) to 6 (very often). All six core self-management ability scores were converted to a score between 0 and 100 [22].
Tilburg Frailty Indicator (TFI)
The TFI was administered to describe people’s frailty [8]. The TFI is a self-reported questionnaire and does not include performancebased tests. The TFI describes frailty in terms of the physical, psychological and social domains, these domains containing eight, four and three components, respectively. The physical domain includes questions about physical health, walking with difficulty, problems maintaining body balance and body weight, a lack of hand strength, problems with hearing and seeing, and physical tiredness. The psychological domain includes questions about problems with memory, being gloomy, feelings of nervousness or anxiety, and coping with problems. The social domain contains questions about living alone, loneliness and social support. Scores for the TFI range from 0 to 15; for the physical, psychological, and social domains the score ranges are 0 - 8, 0 - 4, and 0 - 3, respectively. People with a total TFI score equal to or above 5 are considered as frail.
Validity Reliability and Rigour
The internal consistency for the SMAS-30 is high (α = 0.90). Cronbach’s α for the subscales ranged from 0.63 to 0.77. The construct validity of the SMAS-30 was supported by meaningful associations with other constructs [21-22]. Reliability for the TFI is moderate to good for total frailty and the physical and psychological domains (Cronbach’s α are 0.73; 0.70 and 0.63, respectively), and low for the social domain (0.34) [3] (Gobbens et al., 2010b; Sutton et al., 2016). The 15 items and the frailty domains (physical, psychological, social) of the TFI correlated as expected with validated measures, demonstrating both convergent and divergent construct validity of the TFI. The predictive validity of the TFI and its physical domain was good for quality of life and the adverse outcomes disability and receiving personal care, nursing and informal care [3,8,30] (Gobbens et al., 2010b; Gobbens, van Assen, Luijkx, & Schols, 2012; Sutton et al., 2016).
Chronic Diseases
Sixteen chronic diseases that often occur in elderly people were examined by self-report: diabetes mellitus, cerebrovascular accidents, myocardial infarction, other serious cardiac disease, cancer, migraine, hypertension, peripheral arterial disease, chronic obstructive pulmonary disease (COPD), psoriasis, urinary incontinence, dementia, depression, arthrosis, rheumatoid arthritis and Parkinson’s disease.
Sociodemographic Characteristics
We asked participants to provide information on the sociodemographic characteristics of age, gender, marital status, level of education and ethnicity.
Ethical Considerations
Medical ethics approval was not necessary as particular treatments or interventions were not offered or withheld from the respondents. The integrity of the respondents was not encroached upon as a consequence of participating in this study, which is the main criterion in medical ethical procedures in the Netherlands [25]. In addition, the ethical commission of Amstelland Thuiszorg approved the study. Written informed consent for the collection and use of the information was obtained from all respondents.
Data Analysis
Data were analysed with SPSS for Windows, version 24.0 (IBM Corp., Armonk, NY, USA). Firstly, the characteristics of the participants were determined with descriptive statistics. Subsequently, correlations were determined between the three domains of frailty (physical, psychological and social) and the six abilities of self-management. Moreover, we examined the correlations between the total score on the TFI and the total score on the SMAS-30. Correlations were considered to be small, medium or large with coefficients of 0.1, 0.3 or 0.5, respectively [26]. Finally, with sequential multiple linear regression analyses, we assessed the effect of the individual frailty domains of the TFI on the six abilities of self-management of the SMAS-30. These analyses consisted of three blocks: the first block contained the sociodemographic characteristics of the participants, the second contained the number of chronic diseases, and the third contained the six abilities of self-management. The second and third blocks enabled testing the effect of chronic diseases and the individual frailty domains on self-management abilities, after controlling for all other variables in the model. All statistical tests were conducted two-sided with an alpha level of 0.05.
Results
Background Characteristics
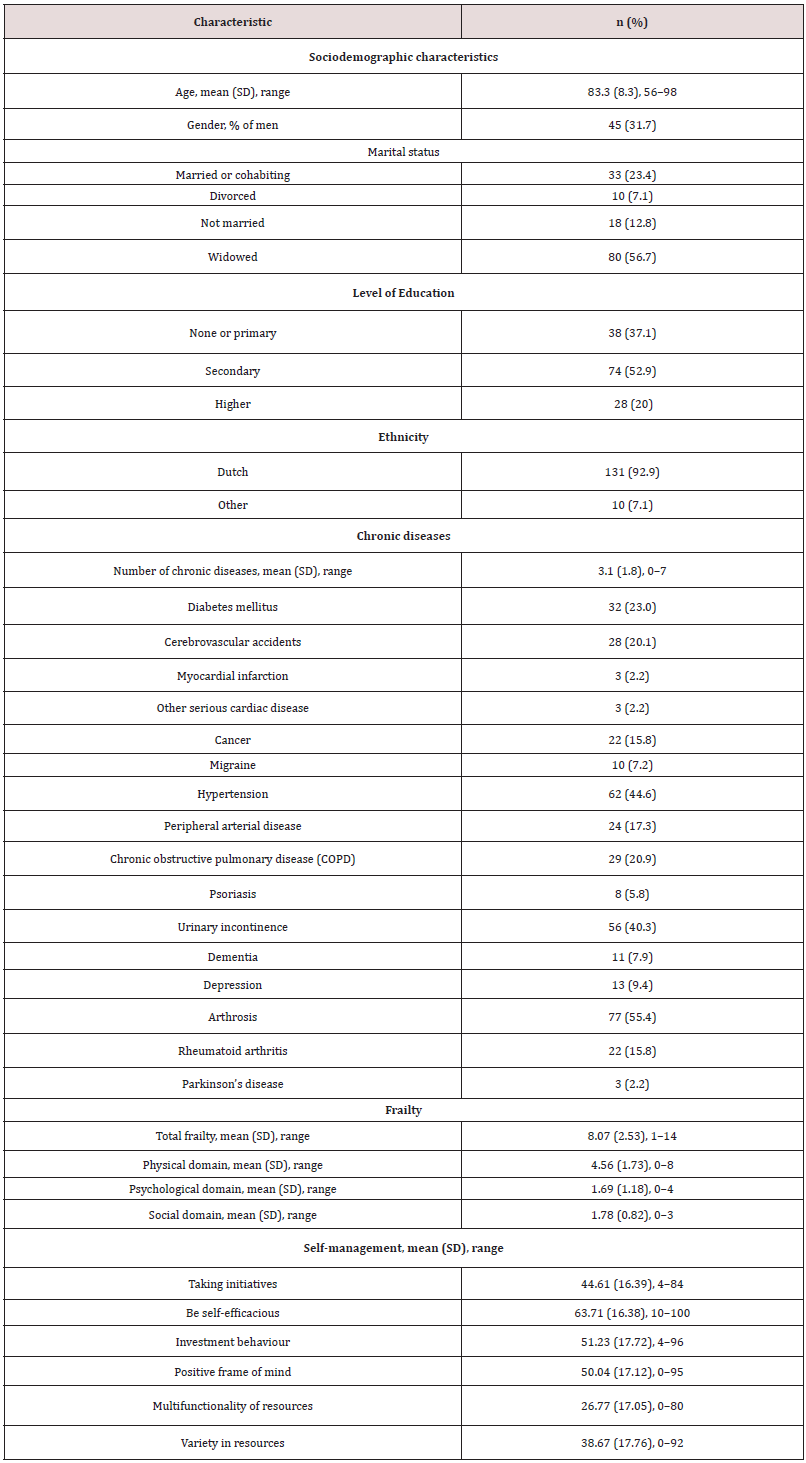
Table 1 describes the characteristics of the participants. The mean age was 83.3 (SD 8.3); 45 (31.7%) of the participants were male and 33 (23.4%) were married or cohabiting. On average, the participants had three chronic diseases (range 0-7); their mean total frailty was 8.07 (SD 2.53); and the mean frailty of the physical domain was 4.56 (SD 1.73), which is relatively high.
Table 1: Participant characteristics (N = 142), regarding sociodemographic characteristics, chronic diseases, frailty and self-management.
Correlations Between Self-Management Abilities and Frailty Domains
The correlation between total frailty and total self-management was -0.421 (p<0.001). Table 2 shows that all significant correlations were small to medium (ranging between -0.177 and -0.408). All six self-management abilities were significantly negatively correlated with the physical frailty domain. Five of the six self-management abilities were also significantly correlated with the psychological frailty domain. The multifunctionality of resources ability showed no significant correlation with the psychological and social frailty domains. The positive frame of mind and variety in resources abilities of self-management correlated negatively with the social frailty domain; the other four abilities (taking initiatives, being self-efficacious, investment behaviour, multifunctionality) did not correlate (Table 2).
Table 2: Correlations between frailty domains and self-management abilities.
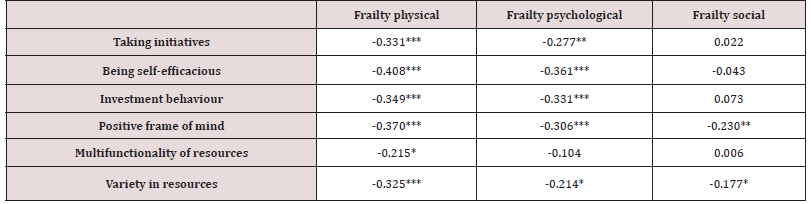
*** Correlation is significant at the 0.001 level
** Correlation is significant at the 0.01 level
* Correlation is significant at the 0.05 level
Effects of Self-Management Abilities on Frailty Domains
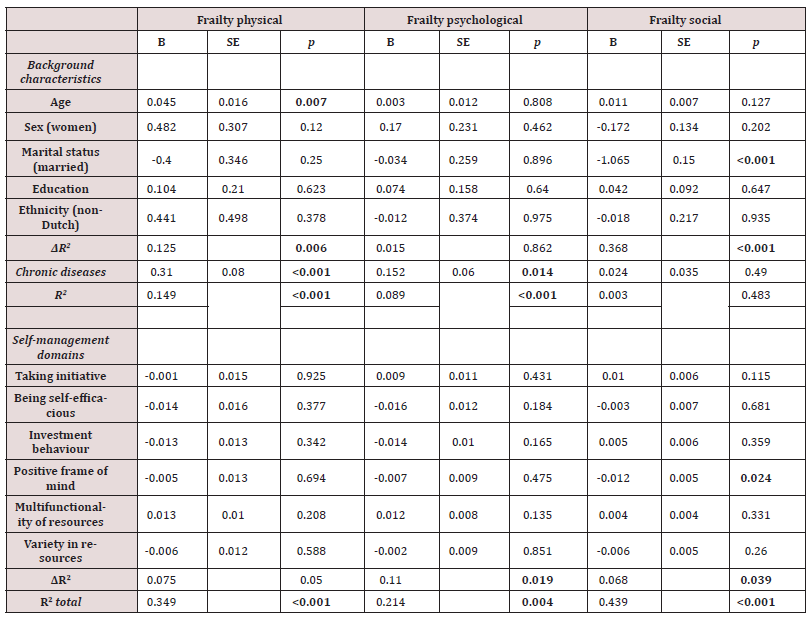
Table 3 presents the results of the sequential multiple linear regression analysis. The row ΔR2 indicates how much of the variance in the three frailty domains (physical, social and psychological) was explained by the three blocks (sociodemographic characteristics of the participants, chronic diseases, and the six abilities of selfmanagement), and shows the extent to which (the increased) explained variance was statistically significant. All variables in the model, the background characteristics, chronic diseases and the six self-management abilities together significantly explained 34.9 per cent, 21.4 per cent and 43.9 per cent of participants’ physical, psychological and social frailty, respectively.
Table 3 also shows that the background characteristics together significantly explained 12.5 per cent of physical frailty and 36.8 per cent of social frailty. Having two or more chronic diseases significantly explained 14.9 per cent of physical frailty and 8.9 per cent of being socially frail, after controlling for background characteristics. In addition, after controlling for background characteristics and chronic diseases, the six self-management abilities together significantly explained 11 per cent of psychological frailty and 6.8 per cent of social frailty. In this sample, the six selfmanagement abilities together did not significantly explain physical frailty (p=0.050). Of the five background characteristics, and after controlling for all variables, age was significantly negatively associated with physical frailty, and being married was significantly negatively associated with social frailty. Table 3 also shows that having a positive frame of mind is the only self-management ability which significantly influences social frailty. None of the other selfmanagement abilities significantly influenced participants’ physical or social frailty.
Table 3: Effect of background characteristics, chronic diseases, and self-management domains on frailty domains: regression analysis.
Discussion and Implications
vThe aim of this study was to increase our knowledge about the associations between the self-management abilities of older people and their physical, psychological and social frailty. This knowledge can help community nurses to develop or specify interventions to strengthen the self-management abilities of the older people they care for, aiming to prevent or delay the onset of frailty. This study was carried out among 145 Dutch community-dwelling people who received home care from Amstell and Thuiszorg, and is the first study to examine the relationship between self-management abilities, measured with the SMAS-30, and frailty, measured with the TFI. The present study has shown a significant relationship between the six self-management abilities and physical frailty. These results are in accordance with the studies by [18-27].
Op het Veld et al. (2015) and found a significant relationship between the SMAS-S (short version) and physical frailty measured with the Fried criteria [4] (Fried et al., 2001). The sample in the study by [27] was younger than the sample in our study [17]. found a significant negative association between self-management abilities (measured with the short version of the SMAS-S) and frailty (measured with the TFI) in older people with poor health. In our study, we did not measure poor health: instead, we measured the number of chronic diseases of the participants. Also, the participants in our study were older people receiving home care, with a higher mean age (83.3 versus 77.9 years) and a higher mean score of total frailty (8.07 versus 4.9) compared to the participants in the study by Cramm et al. (2014) [18]. The people participating in our study had on average 3.1 (range 0-7) chronic diseases. Steverink [29] concluded in their study that a study population with a mean of 3.1 chronic diseases is high. Although the mean age of their study population was lower (76.5), not all participants received care and they included nine diseases instead of seven, it is conceivable that the participants in our sample also had poor health and are therefore comparable with the participants in the study by Cramm et al. (2014). [18]. As described in the background section, frail older people experience a lower quality of life (Kojima et al., 2016) [10]. People with more self-management abilities report better health and experience more feelings of happiness (Steverink, 2016) [28]. Our results showed that five of the six selfmanagement abilities (not multifunctionality of resources) are also negatively associated with feeling psychologically frail, and the self-management abilities of having a positive frame of mind and variety of resources are also negatively associated with social frailty. [15] Cramm and Nieboer (2017) describe that community nurses have the possibility to influence the self-management abilities of frail elderly, leading to a higher quality of life. To support the selfmanagement of the patient, it is necessary that nurses change their attitude (Alleyne, Hancock, & Hughes, 2011) [31]. To influence self-management abilities effectively, it is first of all important that nurses have a person-centred approach for all individuals who live with frailty to fit their own needs (Abbasi et al., 2018) [32], but they also need to express a coaching role and see the patient as an equal partner in healthcare (McDonald, Rogers, & Macdonald, 2008; Wilson, Kendall, & Brooks, 2006) [33,34]
Van Hooft et al. (2015) [16] examine the role of the coach and describe three other perspectives of nursing in self-management support: the clinician, gatekeeper and educator perspective. The nurse as coach supports the patient’s daily life activities, whereas the nurse as clinician aims to achieve adherence to treatment. The goal of self-management support from the gatekeeper perspective is to reduce healthcare costs. Finally, the nurse as educator focuses on instructing patients in managing the illness [16]. Another intervention, the Dutch course ‘Grip and Glance’ for communitydwelling elderly people developed by, aims to help people to identify which of the six resources of self-management they would like to take steps to improve. This intervention makes people aware of the possibility of contributing to their own feeling of wellbeing: after all, self-management is about knowing what makes you happy and feel well and knowing what to do to achieve this, which also positively influences the experienced quality of life. Effective interventions applied by community-dwelling nurses are developed and examined all over the world, individually or group-based, and intervene in self-management abilities with the aim of preventing or delaying the development of physical frailty (Apóstolo et al., 2018) [35].
In contrast to the study by Cramm and colleagues (2014) [18], the results of the regression analysis in our study show that in addition to the background variables, chronic diseases and all six self-management abilities measured with the SMAS-30 together influence the extent to which the people who receive homecare are physically, psychologically and socially frail, as measured with the TFI. Cramm and colleagues (2014) found a negative relationship between self-management abilities and poor health and a positive relationship between poor health and total frailty, but they did not analyse whether self-management abilities had an effect on frailty in older people. Our results also showed that the six self-management abilities together influence psychological and social frailty, but not physical frailty, after controlling for background characteristics and chronic diseases. More specifically, the self-management ability of having a positive frame of mind influences social frailty in older people receiving home care. In another study, Cramm and colleagues (2012a) [19] also found a relationship between having a positive frame of mind and depression. It is relevant to have insight into interventions which can be executed by the community nurses to positively influence the positive frame of mind of older people. Zou, Cao, Geng, and Chair (2019) [36]. found in their systematic review that mindfulness-based interventions seem to positively influence feelings of depression and anxiety and improve healthrelated quality of life. The interventions described in this study were executed by trained nurses. Nowadays, mindfulness training or meditation exercises are also digitally available. Duraimani (2019) [37]. found that people with chronic diseases who did meditation using the mindfulness meditation application experienced significantly less stress and anxiety. Participants in this study were mostly not older people: 19 of the 122 participants were between 56 and 68 years old. It is questionable if the older people in our sample are able to use digital applications, but this will change quickly in the coming years. In the near future, all older people will use a mobile phone, which provides our community nurses with more opportunities to strengthen the self-management abilities of their elderly patients.
This study has some limitations. Firstly, we used a crosssectional research design to determine the influence of selfmanagement abilities on the frailty of community-dwelling older people; because of this design, we cannot draw causal relations between these two concepts. Secondly, although we were satisfied with the 145 patients participating in our sample, we realize that 462 community-dwelling patients under Thuiszorg Amstelland did not fill in the questionnaires, so the response rate for this study is low. For this reason, and because we have only approached patients of this specific care organization which is located in a specific region of the Netherlands (Amstelveen and surroundings), we have to be careful about generalizing the results. On the other hand, despite the small sample, we did find significant results. Another limitation is that the present study was a self-report study, which could lead to socially desirable answers. It is positive, however, that the SMAS- 30 and the TFI are validated instruments (Gobbens et al., 2010a, 2010b; Schuurmans et al., 2005; Sutton et al., 2016) [3, 8, 11, 21].
In conclusion, the present study showed that self-management abilities of older people receiving home care are significantly negatively associated with frailty. The six self-management abilities together influence the psychological and social frailty of older people. Community nurses have the task of stimulating and supporting the self-management abilities of the older people they care for. Supporting interventions for strengthening the self-management abilities of older people need to focus on their personal goals and interests, and subsequently work according to a plan focusing on possibilities [22]. Older people with a positive frame of mind are more able to influence their social frailty positively. (Digital) interventions focusing on mindfulness meditation can help them to maintain this positive frame of mind. Community nurses are able to coach older people to start this trainings, advising them to do small exercises or using a mindfulness meditation app.
References
- United Nations Department of Economic and Social Affairs (2015).
- Collard RM, Boter H, Schoevers RA, Oude Voshaar RC (2012) Prevalence of frailty in community-dwelling older persons: A systematic review. Journal of the American Geriatrics Society 60(8): 1487-1492.
- Sutton JL, Gould RL, Daley S, Coulson MC, Ward EV, et al. (2016) Psychometric properties of multicomponent tools designed to assess frailty in older adults: A systematic review. BMC Geriatrics 16(1): 55.
- Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, et al. (2001) Frailty in older adults: Evidence for a phenotype. The Journals of Gerontoloy Series A Biological Sciences and Medical Sciences 56(3): 146-156.
- Morley JE, Malmstrom TK, Miller DK (2012) A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. Journal of Nutrition. Health and Aging, 16(7): 601-608.
- Mitnitski AB, Mogilner AJ, Rockwood K (2001) Accumulation of deficits as a proxy measure of aging. The Scientific World Journal 1 p. : 323-336.
- Rolfson DB, Majumdar SR, Tsuyuki RT, Tahir A, Rockwood K (2006) Validity and reliability of the Edmonton Frail Scale. Age and Ageing 35(5): 526-529.
- Gobbens RJ, van Assen MA, Luijkx KG, Wijnen-Sponselee MT, Schols JM (2010b) The Tilburg Frailty Indicator: Psychometric properties. Journal of the American Medical Directors Association 11(5): 344-355.
- Vermeiren S, Vella Azzopardi R, Beckwee D, Habbig AK, Scafoglieri A, et al. (2016) Frailty and the prediction of negative health outcomes: A meta-analysis. Journal of the American Medical Directors Association 17(12): 1163.e1161-1163.e1117.
- Kojima G, Iliffe S, Jivraj S, Walters K (2016) Association between frailty and quality of life among community-dwelling older people: A systematic review and meta-analysis. Journal of Epidemiology and Community Health 70(7): 716-721.
- Gobbens RJ, van Assen MA, Luijkx KG, Wijnen Sponselee MT, Schols JM (2010a) Determinants of frailty. Journal of the American Medical Directors Association 11(5): 356-364.
- Lorig KR, Holman H (2003) Self-management education: History, definition, outcomes, and mechanisms. Annals of Behavioral Medicine 26(1): 1-7.
- Paterson BL (2001) The shifting perspectives model of chronic illness. Journal of Nursing Scholarship, 33(1): 21-26.
- van Campen C, Ras M, den Draak M (2011) Estimate of the number of frail older persons up to the year 2030. In C. van Campen (Ed.), Frail older persons in the Netherlands (pp. 69–80). The Hague: The Netherlands Institute for Social Research.
- Cramm JM, Nieboer AP (2017) Self-management abilities and quality of life among frail community-dwelling individuals: The role of community nurses in the Netherlands. Health & Social Care in the Community 25(2): 394-401.
- van Hooft SM, Dwarswaard J, Jedeloo S, Bal R, van Staa A (2015) Four perspectives on self-management support by nurses for people with chronic conditions: A Q-methodological study. International Journal of Nursing Studies 52(1): 157-166.
- Cramm JM, Strating MM, de Vreede PL, Steverink N, Nieboer AP (2012) Validation of the self-management ability scale (SMAS) and development and validation of a shorter scale (SMAS-S) among older patients shortly after hospitalisation. Health and Quality of Life Outcomes 10 p. : 9.
- Cramm JM, Twisk J, Nieboer AP (2014) Self-management abilities and frailty are important for healthy aging among community-dwelling older people: A cross-sectional study. BMC Geriatrics 14: 28.
- Cramm JM, Hartgerink JM, de Vreede PL, Bakker TJ, Steyerberg, et al. (2012a) The relationship between older adults’ self-management abilities, well-being and depression. European Journal of Ageing 9: 353-360.
- Schuurmans H, Steverink N, Lindenberg S, Frieswijk N, Slaets JP (2004) Old or frail: What tells us more? The Journals of Gerontology Series A Biological Sciences and Medical Sciences 59(9): 962-965.
- Schuurmans H, Steverink N, Frieswijk N, Buunk BP, Slaets JP, et al. (2005) How to measure self-management abilities in older people by self-report. The development of the SMAS-30. Quality of Life Research 14(10): 2215-2228.
- Steverink N (2009) Self-Management Ability Scale SMAS-30 / version 2. Background, manual and scoring [Self-Management Ability Scale: SMAS-30/versie 2. Achtergrond, handleiding en scoring]. Rijksuniversiteit Groningen en Universitair Medisch Centrum Groningen.
- Steverink N, Lindenberg S, & Slaets JPJ (2005) How to understand and improve older people's self-management of wellbeing. European Journal of Ageing 2(4): 235.
- Nieboer AP, Lindenberg S, Boomsma A, Van Bruggen AC (2005) Dimensions of wellbeing and their measurement: The SPF-IL Scale. Social Indicators Research 73 p. : 313-353.
- Central Committee on Research Involving Human Subjects (2010).
- Cohen J (1988) Statistical power analysis for the behavioral sciences (2nd ed.). Lawrence Erlbaum Assoc Inc.
- Op het Veld LPM, van Rossum E, Kempen GIJM, de Vet HCW, Hajema KJ, et al. (2015) Fried phenotype of frailty: Cross-sectional comparison of three frailty stages on various health domains. BMC Geriatrics 15 p. : 77.
- Steverink N (2016) The power of social relationships: The influence of social relationships on self-management skills, health and well-being [De kracht van sociale relaties: De invloed van sociale relaties op zelfmanagementvaardigheid, gezondheid en welbevinden]. Groningen: Rijksuniversiteit, Groningen.
- Gobbens RJJ, Renn I (2018) Effects of frailty and chronic diseases on quality of life. Clinical Interventions in Aging 13 p. : 325-334.
- Gobbens R, van Assen M, Luijkx KG, Schols J (2012) The predictive validity of the Tilburg Frailty Indicator: Disability, health care utilization, and quality of life in a population at risk. Gerontologist 52(5): 619-631.
- Alleyne G, Hancock C, Hughes P (2011) Chronic and non-communicable diseases: a critical challenge for nurses globally. International Nursing Review 58(3): 328-331.
- Abbasi M, Rolfson D, Khera AS, Dabravolskaj J, Dent E, et al. (2018) Identification and management of frailty in the primary care setting. Canadian Medical Association Journal 24(190): 1134-1140.
- McDonald R, Rogers A, Macdonald W (2008) Dependence and identity: nurses and chronic conditions in a primary care setting. Journal of Health, Organisation and Management 22(3): 294-308.
- Wilson PM, Kendall S, Brooks F (2006) Nurses responses to expert patients: the rhetoric and reality of self-management in long-term conditions: a grounded theory study. International Journal Nursing Studies, 43(7): 803-818.
- Apóstolo J, Cooke R, Bobrowicz Campos E, Santana S, Marcucci M, et al. (2018) Effectiveness of interventions to prevent pre-frailty and frailty progression in older adults: A systematic review. JBI Database of Systematic Reviews and Implementation Reports, 16(1): 140-232.
- Zou H, Cao X, Geng J, Chair SY (2019) Effects of mindfulness-based interventions on health-related outcomes for patients with heart failure: A systematic review. European Journal of Cardiovascular Nursing, 147451511988194.
- Duraimani SL (2019) A cross-sectional and longitudinal study of the effects of a mindfulness meditation mobile application platform on reducing stress and anxiety. International Journal of Yoga 12(3): 226-232.
Editorial Manager:
Email:

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...