Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6695
Review Article(ISSN: 2637-6695) 
Student Nurses Knowledge of Breastfeeding and Lactation: A Literature Review Volume 3 - Issue 3
Lizy Mathew1, Karen F Phillips1* and Linda M Salvesen2
- 1Department of Nursing, College of Science and Health, William Paterson University, USA
- 2Nursing Librarian, Cheng Library, William Paterson University, USA
Received: March 08, 2022; Published: March 18, 2022
Corresponding author: Department of Nursing, College of Science and Health, William Paterson University, 300 Pompton Rd, Wayne, NJ 07470, USA
DOI: 10.32474/LOJNHC.2022.03.000161
Abstract
Breastfeeding has long been considered as the optimal feeding method for all infants and the American Academy of Pediatrics (AAP) recommends exclusive breastfeeding for at least the first six months [1]. As well, the Centers for Disease Control (CDC) agrees that breastfeeding is the best source of nutrition for infants [2] and the World Health Organization (WHO) concurs the exclusive breastfeeding that exclusive breastfeeding is the unequalled infant feeding method for the first six months [3]. Breastfeeding support and education are considered to be key elements of breastfeeding success [2]. Breastfeeding support from health professionals can be effective in influencing a mother’s decision to initiate and maintain breastfeeding Yang et al. [4]. Despite this knowledge, the research indicates that many nursing programs do not include breastfeeding education in their current curriculum. A literature review was examined that included 11 studies published between the years of 2013 and 2020 that utilized an educational intervention for nursing students on breast feeding. The purpose of the literature review was to examine whether the educational interventions increased student knowledge of breastfeeding, benefits of breast feeding, and attitude towards breastfeeding. The results of the literature review suggested that even a brief educational intervention could improve students’ knowledge and attitude towards breastfeeding and continued education will increase student confidence in supporting breastfeeding mothers, thereby improving breastfeeding support.
Keywords: Breastfeeding; Benefits of Breastfeeding; Educational Interventions on Breastfeeding; Lactation
Introduction
Breastfeeding has long been touted as the optimal feeding choice for all infants. The American Academy of Pediatrics (AAP) recommends exclusive breastfeeding for at least the first six months and continued as long as the mother-infant dyad deem it mutually beneficial [1]. As well, the Centers for Disease Control (CDC) agrees that breastfeeding is the best source of nutrition for infants [2]. The World Health Organization (WHO) concurs that exclusive breastfeeding is the unequalled infant feeding method for the first six months and continued until at least two years or more [3]. Exclusive breastfeeding can reduce the risk of certain health conditions [1]. Studies have shown an association between breastfeeding and increased health benefits for both mothers and infants. Breastfeeding has been linked to better maternal and newborn outcomes worldwide [1-3]. As well, exclusive breastfeeding of infants has been found to promote cognitive development and protect against infectious diseases such as diarrhea or pneumonia [3]. An association has been noted between breastfeeding mothers and a reduced risk of type two diabetes, breast cancer, and ovarian cancer [2,3]. Key components to breastfeeding success threaded through the literature are breastfeeding support and education [2]. Breastfeeding support from healthcare professionals has been found to be a factor in a mother’s decision to breastfeed [4,5]. Although considered a natural act, breastfeeding is a learned behavior [3]. The need for breastfeeding support from caregivers and healthcare workers led to the development of the Ten Steps to Successful Breastfeeding developed by WHO and UNICEF [3]. The emergence of the Ten Steps to Successful Breastfeeding led to the development of a breastfeeding counseling course to offer education and training to healthcare personnel who work with breastfeeding women in an effort to improve breastfeeding initiation and continuation [3].
Background
Nursing education aims to promote positive health practices among the general population as well as among nurses themselves [6]. Breastfeeding is considered one of these important health practices [6]. Breastfeeding support from health professionals can be effective in influencing a mother’s decision to initiate and maintain breastfeeding [4]. A key reason cited for premature cessation of breastfeeding is inadequate support from healthcare providers [7]. As such, increasing health professional confidence in clinical lactation skills is key to improving maternal and child health outcomes [7]. Healthcare providers, including nursing students, do not always get the education and training to feel confident in assisting breastfeeding mothers [4, 8]. The research depicts either no breastfeeding education or limited education in new graduate nurses. This in turn impacts their confidence in their ability to provide the necessary guidance and support [9]. Studies demonstrate when mothers felt unprepared to breastfeed, breastfeeding initiation and continuation rates go down [8]. Since nutrition is critical in the first year of life, it becomes essential that undergraduate curriculum provide education in breastfeeding to assist students in acquiring the necessary skills and knowledge [10]. This literature review indicates that many nursing programs do not include breastfeeding education in current curriculum. This is significant because nurses are the primary caregivers for postpartum/breastfeeding mothers [9]. Breastfeeding research shows that targeted breastfeeding education, didactic and clinical, has significantly increased breastfeeding knowledge [9,11]. As such, it is important that health care professionals including nurses, who spend the majority of time with the patients, be able to offer consistent, accurate knowledge regarding breastfeeding and lactation [8]. Despite these findings breastfeeding education is not a standard in nursing program curriculum [9].
Findings
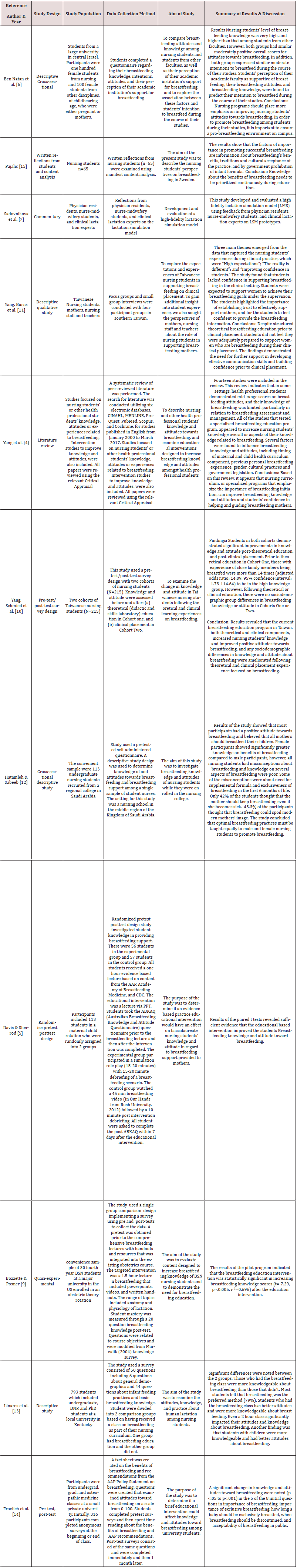
This review of the literature was done to examine whether educational interventions increased student nurses’ knowledge of breast feeding, benefits of breast feeding, and attitude towards breastfeeding. Although the literature search provided many articles in regard to breastfeeding support and education, this review looked at 11 studies published between the years of 2013 and 2020 that included an educational intervention aimed at improving breastfeeding knowledge. One study by Yang, Burns, et al. [11] revealed that despite structured theoretical breastfeeding education, students did not feel confident in supporting breastfeeding in a clinical setting. A study by Ben Natan et al. [6] surveyed female students and found that the support received from campus were predictive of female students’ intention to breastfeed even though students had very high knowledge and positive attitude towards breastfeeding. Another study by Hatamleh & Sabeeb [12] revealed a greater knowledge of breastfeeding in female nursing students than male students but concluded that breastfeeding education should be provided equally to males and females to better promote breastfeeding. A large study by Linares et al. [13] showed that even a two hour class significantly impacted student attitudes and knowledge about breastfeeding. Similar results were noted in a study by Froelich et al. [14] which indicated that even a brief educational intervention could affect knowledge and attitude toward breast feeding. A literature review conducted by Yang et al. [4] examined nursing students’ or other health professional students’ knowledge, attitudes or experiences related to breastfeeding. Findings suggested that nursing curriculum can improve breastfeeding knowledge, students’ attitudes, and students’ confidence in helping and guiding breastfeeding mothers. A study by Davis and Sherrod [5] and another study by Bozzette & Posner [9] revealed that an educational based intervention improved the students’ breastfeeding knowledge and attitude toward breastfeeding. As well, a study by Pajalic [15] showed that in addition to breastfeeding benefits, information on traditions and cultural acceptance of breastfeeding should be included in nursing education (Table 1).
Conclusion
Breastfeeding is the optimal method of infant feeding [1] and has been associated with health benefits for both the mother and infant [1-3]. Breastfeeding success has been associated with the components of education and support [2]. Inadequate support from healthcare professionals has been linked to earlier breastfeeding cessation [7]. Nurses have been noted as the primary caregivers for breastfeeding women [9]. Many nursing programs do not include breastfeeding education in the curriculum impacting new graduate nurse’s ability to provide assistance to breastfeeding mothers. The purpose of the literature review was to examine articles pertinent to the breastfeeding knowledge of nursing students to determine if an educational intervention could improve nursing student’s attitudes and knowledge of breastfeeding and lactation. Eleven studies were reviewed where an educational intervention was provided to nursing students. All studies reviewed suggested that even a brief educational intervention could improve students’ knowledge and attitude towards breastfeeding and continued education will increase student confidence in supporting breastfeeding mothers.
References
1. American Academy of Pediatricians (AAP) (2012) Breastfeeding and the Use of Human Milk 129(3): e827-e841.
2. Centers for Disease Control (CDC) (2021) About Breastfeeding.
3. World Health Organization (WHO) (2022) Breastfeeding.
4. Yang SF, Salamonson Y, Burns E, Schmied V (2018) Breastfeeding knowledge and attitudes of health professional students: A systematic review. International Breastfeeding 13(8): 1-11.
5. Davis A, Sherrod R (2015) Effects of an Educational intervention on baccalaureate nursing students’ knowledge and attitude in providing breastfeeding support to mothers. International Journal of Childbirth Education 30(4): 8-12.
6. Ben Natan M, Haikin T, Wiesel R (2018) Breastfeeding knowledge, attitudes, intentions, and perception of support from educational institutions among nursing students and students from other faculties: A descriptive cross-sectional study. Nurse Education 68: 66-70.
7. Sadovnikova A, Chuisano SA, Ma K, Grabowski A, Stanley KP, et al. (2020) Development and evaluation of a high-fidelity lactation simulation model for health professional breastfeeding education. International Breastfeeding 15(1): 8.
8. Vandewark A (2014) Breastfeeding attitudes and knowledge in Bachelor of Science nursing candidates. Journal of Perinatal Education 23(3): 135-141.
9. Bozzette M, Posner T (2013) Increasing student nurses’ knowledge of breastfeeding in baccalaureate education. Nurse Education in Practice 13(3): 228-233.
10. Yang SF, Schmied V, Burns E, Salamonson Y (2019) Breastfeeding knowledge and attitudes of baccalaureate nursing students in Taiwan: A cohort study. Women and Birth: Journal of the Australian College of Midwives 32(3): e334-e340.
11. Yang S, Burns E, Salamonson Y, Schmied V, (2019) Expectations and experiences of nursing students in supporting new mothers to breastfeed: A descriptive qualitative study. Journal of Clinical Nursing, 28(11-12): 2340-2350.
12. Hatamleh W, Sabeeb Z (2015) Knowledge and Attitude toward Breastfeeding among Nursing Students. Journal of Natural Sciences Research 5(16): 147-152.
13. Linares A, Parente A, Coleman C (2018) Attitudes, practices, and knowledge about human lactation among nursing students. Clinical Lactation 9(2): 59-65.
14. Froelich J, Boivin M, Rice D, McGraw K, Munson E, et al. (2013) Influencing university students’ knowledge and attitudes toward breastfeeding. Journal of Nutrition Education and Behavior 45(3): 282-284.
15. Pajalic Z (2014) Nursing students' views on promoting successful breastfeeding in Sweden. Global Journal of Health Science 6(5): 63-69.
Editorial Manager:
Email:

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...