Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6695
Research Article(ISSN: 2637-6695) 
How to Follow the Cancer Risk of Women with Breast Implants Volume 2 - Issue 3
Richard M Fleming1*, Matthew R Fleming1, Tapan K Chaudhuri2 and William C Dooley3
- 1FHHI-OmnificImaging-Camelot, Los Angeles, CA, USA
- 2Eastern Virginia Medical School, Norfolk, VA, USA
- 3Oklahoma University Health Science Center, Oklahoma City, Oklahoma
Received: November 05, 2019; Published: November 12, 2019
Corresponding author: Imani Behzad, Department of Operating Room, School of Paramedicine, Hamadan University of Medical Sciences, Hamadan, Iran
DOI: 10.32474/LOJNHC.2019.02.000137
Abstract
Background: Breast implants are now recognized to be associated with a variety of potential problems, including inflammatory changes – both locally and systemically–precancerous and cancerous changes. Monitoring these changes are particularly problematic in the face of breast implants. Molecular breast imaging (MBI) using FMTVDM* provides a unique method for measuring changes in breast tissue in these individuals. This study examines that potential.
Methods: Eighteen breast implants were evaluated in women who had undergone implantation for a variety of reasons. These women underwent measurement of regional blood flow (RBF) and metabolism differences to determine the extent of inflammation, precancerous and cancerous changes.
Results: Measured changes in RBF and metabolism were not influenced by breast implants. Among the 18 breast implant studies; there were 4 instances of inflammation (22%), 5 (28%) instances of precancerous changes and 1 (5%) instance of breast cancer.
Conclusions: MBI using FMTVDM provides a non-invasive ability to measure changes in breast tissue in women who have undergone breast implantation. The measured monitoring of these changes allows clinicians a tool to make clinical decisions regarding either the need to remove the breast implant or provide alternative treatment options.
Keywords: FMTVDM; Breast Cancer; Inflammation; Breast Implants
Abbreviations: FMTVDM: The Fleming Method for Tissue and Vascular Differentiation and Metabolism
Introduction
The risk of inflammatory changes, potential autoimmune diseases and breast cancer in women with breast implants are now well recognized [1-6]. Given the prevalence of breast implants and the likelihood that they will not become a thing of the past, it is important that clinicians be able to monitor the overall health of the women and men with breast implants by measuring changes in breast health [7-9]. This study investigated the prevalence of inflammatory changes in women with breast implants and monitored those changes by measuring metabolic and Regional Blood Flow (RBF) differences associated with inflammatory and cancerous breast changes using The Fleming Method for Tissue and Vascular Differentiation and Metabolism molecular breast imaging.
Method
Patient Enrollment
Eighteen breast implants were interrogated in women with breast irregularities. The women volunteered to undergo FMTVDM Molecular Breast Imaging (MBI), to measure changes in breast tissue RBF and metabolism, to determine if there was evidence of inflammation, precancerous changes or cancer. Their mammography findings were compared along with the information already known about the extent of their breast health. All components of FMTVDM are already FDA approved - including the enhancement of Regional Blood Flow (RBF) and metabolic differences, isotopes and camera. Each woman signed an informed consent agreeing to participate in the nuclear imaging protocol. All personal identifying information was redacted to protect patient identification.
Breast Imaging
Prior to imaging, the nuclear technologist calibrated the Siemens Orbiter camera according to patent instructions to guarantee quantitative calibration of the camera in addition to customary qualitative controls. Patients arrived in the overnight fasting state and were prepared for imaging with placement of an intravenous catheter through which a vasodilator (enhancement) was given, followed by the imaging isotope and flush as previously described [7-9].
Patient Records
Patients provided inter alia detailed medical records, including prior biopsy results, mammography results, family history of cancer, any prior False Positive or False Negative (FPFN) results from prior testing including but not limited to mammography, smoking history, current medications, any diagnosis of dense breasts and breast implants.
Measurement of RBF and Metabolic Differences - Maximal Count Activity (MCA)
Following image acquisition, Regions of Interest (ROI) were drawn around the acquired breast images and the measured scintillation activity of RBF and metabolic differences was obtained (MCA).
Table 1: Patient data and diagnostic information for 18-breast implants.
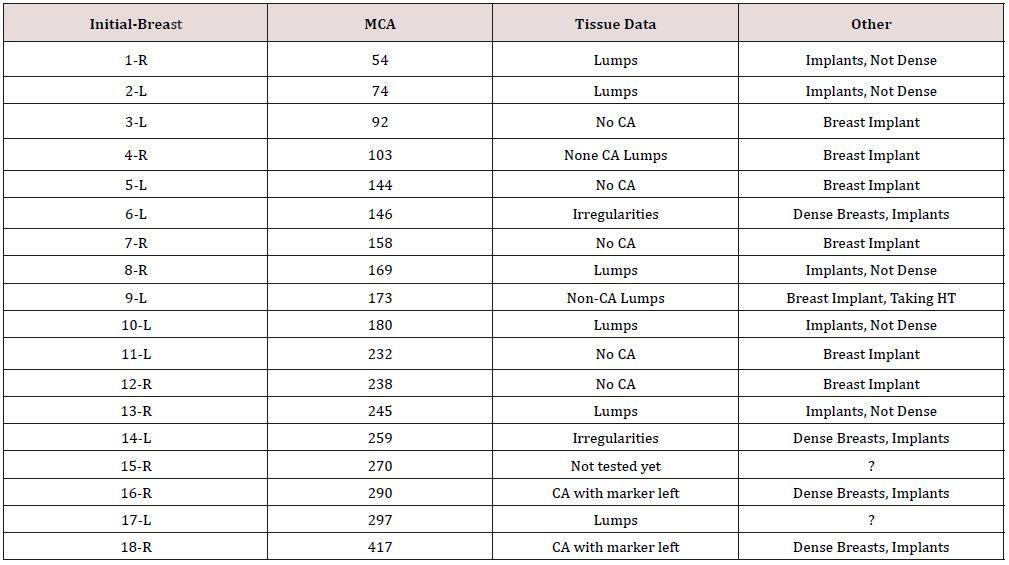
DB = Dense Breasts (Yes, No? =Uncertain), FP=incorrect mammogram, HT=Hormone Therapy
Discussion
While the sample size was relatively small, it provided adequate information to demonstrate that changes in breast tissue inflammation, precancerous and cancerous changes are measurable in women with breast implants. In this study, onethird of the implants were associated with precancerous or cancer changes in the breast and twenty two (22%) percent were associated with inflammation. There was one instance of breast cancer. While the purpose of this study was not to conclude that the breast implants were the cause of the changes in breast tissue, it demonstrated the ability to measure the tissue changes occurring behind the breast implants. Women will undoubtedly continue to have breast implants for a variety of reasons. Perhaps the most clinically important are women who have undergone reconstructive surgery post mastectomy for the treatment of breast cancer. In these women there is a particular risk for recurrence of cancer, which becomes more difficult to evaluate in the presence of breast implants presenting a special challenge for clinicians [10,11]. Breast implants do not affect MCA measurement as the isotope is not taken up into the implants, allowing clear measurements to be obtained in the presence of breast implants [7]. Thus, allowing these women, and men, to be safely monitored for evidence of tissue change in the face of breast implants.
Conclusion
Using FMTVDM, women and men with breast implants can be monitored for changes in breast tissue including inflammation, precancerous and cancer change–alerting clinicians to possible concerns and the need for implant extraction [2] or other treatment The Fleming Method for Tissue and Vascular Differentiation and Metabolism.
Acknowledgment
FMTVDM is a utility patent issued to first author. All figures reproduced with expressed consent of first author. The authors wish to thank David L Prothro, MD of Nevada Arrhythmia Services Inc. in Reno, Nevada for independently conducting patient studies and providing results.
References
- Bizjak M, Selmi C, Praprotnik S, Bruck O, Perricone C, et al. (2015) Silicone implants and lymphoma: The role of inflammation. J Autoimmun 65: 64-73.
- De Boer M, Colaris M, Van Der Hulst RRWJ, Cohen Tervaert JW (2017) Is explantation of silicone breast implants useful in patients with complaints? Immunol Res 65(1): 25-36.
- Orciani M, Sorgentoni G, Olivieri F, Mattioli Belmonte M, Di Benedetto G, et al. (2017) Inflammation by Breast Implants and Adenocarcinoma: Not Always a Bad Company. Clin Breast Cancer 17(4): 286-292.
- Cohen Tervaert JW, Colaris MJ, Van Der Hulst RR (2017) Silicone implants and autoimmune rheumatic diseases: Myth or reality. Curr Opin Rheumatol 29(4): 348-354.
- Leberfinger AN, Behar BJ, Williams NC, Rakszawski KL, Potochny JD, et al. (2017) Breast Implant Associated Anaplastic Large Cell Lymphoma: A Systematic Review. JAMA Surg 152(12): 1161-1168.
- Collett DJ, Rakhorst H, Lennox P, Magnusson M, Cooter R, et al. (2019) Current Risk Estimate of Breast Implant-Associated Anaplastic Large Cell Lymphoma in Textured Breast Implants. Plast Reconstr Surg 143(S3): 30S-40S.
- The Fleming Method for Tissue and Vascular Differentiation and Metabolism (FMTVDM) using same state single or sequential quantification comparisons. Patent Number 9566037.
- Fleming RM, Dooley WC (2002) Breast enhanced scintigraphy testing distinguishes between normal, inflammatory breast changes, and breast cancer: A prospective analysis and comparison with mammography. Integ Ca Ther 1(3): 238-245.
- Fleming RM, Fleming MR (2019) The Importance of Thinking about and Quantifying Disease like Cancer and Heart Disease on a “Health -Spectrum” Continuum. J Compr Cancer Rep 3(1): 1-3.
- Remacle S, Lifrange E, Nizet JL (2015) Management of breast cancer in a woman with breast implants. Rev Med Liege 70(1): 32-36.
- Cho EH, Shammas RL, Phillips BT, Greenup RA, Hwang ES, et al. (2017) Breast Cancer after Augmentation: Oncologic and Reconstructive Considerations among Women Undergoing Mastectomy. Plast Reconstr Surg 139(6): 1240-1249.
Editorial Manager:
Email:

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...