Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6695
Review Article(ISSN: 2637-6695) 
Effects of Ozone, Particulate Matter10 and Oxides of Nitrogen on Respiratory Health (COPD and asthma) in Nigeria: A Systematic Review Volume 3 - Issue 4
Christabel Ihedike* and Jonathan Ling
- Faculty of Health Sciences & Wellbeing, University of Sunderland, United Kingdom
Received: September 11, 2022; Published: September 23, 2022
Corresponding author: Christabel Ihedike, Faculty of Health Sciences & Wellbeing, University of Sunderland, United Kingdom
DOI: 10.32474/LOJNHC.2022.03.000166
Abstract
Background:Nigeria has the largest population of any African country, with 190 million people, and has the largest economy in Africa. Nigeria has become one of the most polluted countries in the globe as a result of recent industrial and population development, coupled with lax regulatory enforcement and a rapid rise in the urban population. This has led to increased emissions of particulate matter, nitrogen oxides, and other pollutants, with consequent harm to the respiratory health of many. This paper is a systematic review of empirical research on air pollution, specifically from ozone, particulate matter, and nitrogen oxides, and their effect on respiratory health in Nigeria.
Methods: Through systematic searching, published research on the effects of air pollution caused by ozone, particulate matter, and nitrogen oxide on respiratory health in Nigeria were obtained from the Discover, PubMed, Google Scholar, and Web of Science databases.
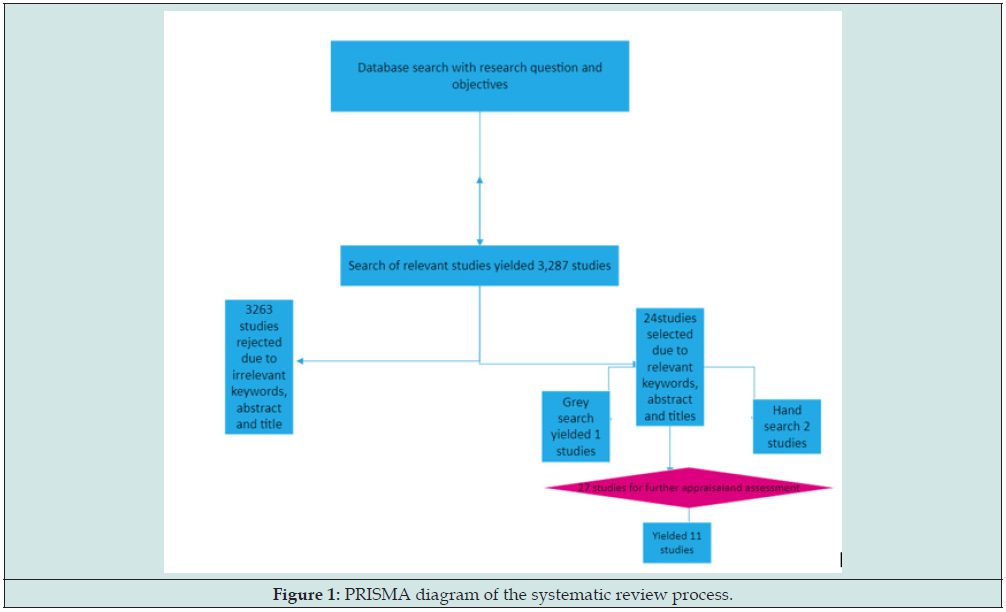
Results: In total, 3,287 publications were returned. The outcome was refined to include only studies with keywords, abstracts, and titles in the last 10 years 27 publications returned. The studies were further appraised for relevance, quality, and studies conducted in Nigeria only, and 11 studies were produced.
Conclusion: The effect of ozone, PM, and nitrogen oxides on respiratory health such as COPD and asthma in Nigeria has risen in the past few years but no study on the effects of O3, PM10, and NOx on Respiratory Health (COPD and asthma) in Nigeria. This review recommends the need for national, state, and local epidemiological data and vital strategies to mitigate the health burden in Nigeria. Global research networks of nations with high pollution levels and scarce resources are critical for generating public support for reducing air pollution and engaging in green technology.
Keywords: Air Pollution; Asthma; Nigeria; COPD; O3; PM; NOX
Introduction
Air pollution is one of this generation’s greatest scourges, not only for its impact on climate change but also on respiratory health due to increased sickness and mortality. Several pollutants play a major role in human disease. Particulate Matter (PM) penetrates the respiratory system via breathing and triggers respiratory and cardiovascular disease, nervous system and reproductive problems, and cancer [1]. Ground level ozone is toxic, damaging the cardiovascular and respiratory systems. Nitrogen oxide is also classified as a hazardous air pollutant. The illnesses caused by the chemicals mostly affect the respiratory system, including Chronic Obstructive Pulmonary Disease (COPD), asthma, bronchiolitis, and lung cancer. The best way to solve this issue is via increased awareness and a multidisciplinary approach by scientific professionals; national and international bodies to confront and provide solutions to air pollution. Air quality in developing nations such as Nigeria is unsafe and has repeatedly been observed to be higher than the WHO standard, with 9 out of 10 breathing polluted air in developing countries such as Nigeria (WHO, 2018). Despite declines in air pollution in most countries, poor outdoor air quality remains a major health threat in Nigeria [2] (WHO, 2018; Global Burden of Disease, 2019; Health Effects Institute, 2020). Because of this, this study is dedicated to a systematic review of such problems in Nigeria.
Particulate Matter (PM): Particulate matter is composed of microscopic liquid or solid particles that may be inhaled and have a detrimental effect on health [3]. Particulate matter is produced in the atmosphere resulting from chemical interactions between various contaminants. PM is composed of organic compounds (benzene, dioxins, polycyclic aromatic hydrocarbons, and 1-3 butadiene) and inorganic compounds (chlorides, carbon, nitrates, metals, and sulphates) [3]. Particle penetration is highly dependent on their size [4]. After inhalation, particles 10
m in diameter (PM10) may enter the lungs and potentially reach the bloodstream. PM5 particles, owing to their microscopic size, are associated with more severe health consequences than PM10. Numerous studies have shown a link between particulate matter and unfavorable health consequences, focusing on either acute (short-term) or chronic (long-term) PM exposure. Numerous epidemiological studies on the health consequences of PM have been conducted. Long-term exposure to PM is associated with cardiovascular illness and neonatal mortality. Respiratory illnesses and immune system dysfunctions are widespread in Nigeria [5]. Those with asthma, diabetes, pneumonia and cardiovascular and respiratory illnesses are more susceptible and sensitive to the effects of PM.
Ozone: Ozone (O3) is produced is formed by a chemical process between nitrogen oxides and volatile organic compounds (VOCs) emitted by natural sources and/or anthropogenic activities. It occurs in the stratosphere, but it may also occur due to photochemical smog chain reactions in the troposphere [6]. Ozone levels above cities are modest compared to the increasing levels in metropolitan regions in Nigeria. Ozone is typically absorbed via inhalation and also interferes with the function and integrity of the skin barrier. Ozone’s toxic effects have been documented in metropolitan areas worldwide, producing morphologic, biochemical, immunological, and functional problems [7-10].
Nitrogen Oxide: Nitrogen oxide is a contaminant associated with traffic as it is produced by automobile engines [11,12]. It is a respiratory irritant that penetrates deeply into the lung, causing respiratory problems such as coughing, dyspnoea, wheezing, bronchospasm, and pulmonary edema at high concentrations. Concentrations over 0.2ppm lead to detrimental effects in humans. In comparison, concentrations greater than 2ppm appear to impact T-lymphocytes, especially CD8+ and NK cells, responsible for immunological response [12]. Lengthy exposure to high levels of nitrogen dioxide has been implicated in the development of chronic lung illness as well as irritation of the eyes, throat, and nose [13]. This study conducted a laborious review of existing studies that have reported on the effect of Ozone, Particulate Matter10, and Oxides of Nitrogen on Respiratory Health (COPD and asthma) in Nigeria with the aim of recognising and generating an understanding of the effect of these pollutants of COPD and asthma.
Methodology
Systematic reviews
A comprehensive and exhaustive overview of recent literature collected from multiple databases and relating to a research topic is given in systematic reviews. The papers were retrieved from Scopus, PubMed, Discover, Google Scholar, and Web of Science databases.
Eligibility
Studies examining respiratory impacts (NOx, PM, and O3) on humans were considered. All the studies considered looked at the effect of air pollution on respiratory health, which a special interest in particulate matter, nitrogen oxides, and ozone in Nigeria. Duplicates of studies were eliminated, and abstracts were independently reviewed, with any disputes addressed by bringing in a second investigator. The final studies were chosen by inclusion criteria that have tried to regulate the main confounding factors (such as meteorological trends and season and smoking and prevailing medical issues for cohorts) and had recorded respiratory health outcomes. The research did not put any limitations on research design; however, only publications in English were included.
Search Strategy
Searchstrategy and selection criteria: A systematic search of the literature on the effect of air pollutants (O3, PM10 and NOx) on COPD and asthma was conducted. The following databases were searched: PubMed, EMBASE, and Discover. Peer-reviewed journals and panel papers from organizations on air pollution associated with O3, PM10, and NOx were reviewed.
Inclusion criteria:
To achieve the aim of this systematic review, the following criteria were used in the selection of the relevant publications and reports.
a) There were no restrictions on publication dates and online database search to include studies conducted on same air pollutants.
b) The study reported any effect of O3, PM10 and NOx associated with COPD and asthma conditions in Nigeria.
c) The study adopted a quantitative research method.
The search on Discover, PubMed, Web of Science, EMBASE, and Biomedical databases, on all peer-reviewed time series and published panel papers, produced a total of 3,287 articles. The outcome was refined to include only studies with keywords, abstracts, and titles. Subsequently, abstracts and titles of studies included were reviewed for relevance so that studies without the effect of O3, PM10, and NOx were excluded, and 22 studies were found. Fewer journals on either O3, PM10, and NOx were found when the search was restricted to studies conducted in Nigeria. A manual and grey search method was used to note studies that might not have been noticed and ensure that the search was exhaustive on all studies conducted in Nigeria. This approach yielded 27 studies and 27 studies were further appraised for relevance and quality. The appraisal entailed reading the 27 articles, and this was carried out using the Cochrane Library’s recommended principles (transparency, methodological rigor, and reproducibility) (Cochrane, 2007). Based on the recommended principles, the studies were examined for reliability and validity, and the areas of appraisal included but were not limited to the sampling method, data collection, sample size, study population, and statistical process used in the analysis and its significance. At the end of the appraisal and assessment, 11 studies were included in this systematic review based on the recommended principles. Figure 1 below is a PRISMA diagram of the systematic review procedure.
Data Extraction
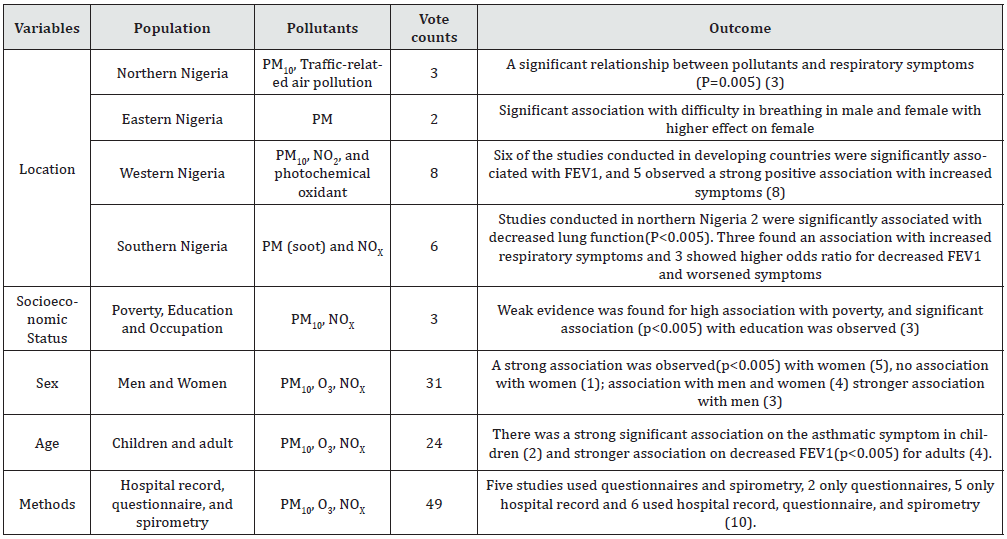
The data were extracted and stored in a database. Study design and population demographics, research time, type of respiratory events, pollutant type, area, confounders addressed, city, exposure classification technique, analytical methodologies, and effect estimations by pollutant, outcome, and related lag time were all extracted from each study. Ten percent of the extracted research data were first examined and found no discrepancies. The remaining data were then examined and validated from the retrieved data. To demonstrate the effects of NOx, PM, and O3 on respiratory health, any information regarding the same was analyzed. A narrative method was adopted in synthesizing the findings from the included studies. This method was ideal for considering the data from the selected studies to review the effects of O3, NOx, and PM10 on COPD and asthma patients in Nigeria. The researcher carried out the data extraction independently, although this was cross-checked by the supervisory team to ensure that all the data extracted were relevant. An agreement was reached on the final data extracted and used in the synthesis. The information extracted included: population description, location, study timeframe, year of publication, sample, results, study design, setting, and number and type of participants. As the systematic review aimed at identifying the effect of O3, PM10, and NOx on COPD and asthma, and considering the data obtained, a vote count approach was chosen as the most appropriate for synthesizing the data in this systematic study.
The vote count is a quantitative method consisting of sorting, counting, and identifying a particular variable(s) in all the included studies. Vote counting uses the frequencies or percentages of these variables in the data set to make valuable conclusions by considering the outcome and strength of the statistical test for significance (Light and Smith, 1971; Heyvaert, Hannes, and Onghena, 2016). As presented in Table 1, the variables used for the vote counting of the extracted data were the location of the study, the ethnicity of the study population, socioeconomic status of the study populations of the study population, age of study, and methods used in the studies. Moreover, the vote count method can either count the number of studies with negative or positive direction with or without statistical significance (Bushman, 1994). Although with this approach, there is a number of disadvantages vote-counting in one direction does not provide the quantity of difference between the groups (effect size) or vote counting gives the same weight to different studies, therefore, the ambiguity around the statistical significance and underpowered assessments in clinically significant but statistically not significant effects would be counted as “no effect.
In order to overcome these disadvantages, more explicit analytical approaches of vote count reporting were explored:
a) The number of studies showing direction and strength of association.
b) Including the age, sex socioeconomic status and sensitive population
c) The number of studies showing statistically significant effects.
This allows for assessing the likely association, and effects in all studies included. By utilizing these more explicit approaches we include relevant information from all the reviewed studies. As such, vote count method provided a useful platform for this systematic review and this method has been widely used in medicine (Cook et al., 1992; Hölzel et al., 2011) and public health (Gerrard et al., 1996; Flodgren et al., 2011).
Risk of Bias
Due to the lack of a standardized documented framework to assess bias in environmental epidemiological data, the risk of bias was assessed concerning the following biases determined a priori: selection bias, detection bias, exposure categorization bias, and the confounding variables addressed. Some exposure categorization bias was anticipated in most included studies as many epidemiological data often employ fixed-site surveillance as a proxy for personal exposure. This review assigned a medium risk of exposure bias to studies that determined exposure status using more than three fixed-site monitors but a high risk to those that utilized three or less. Low risk was assigned to studies that utilized atmospheric modelling or human exposure assessments. Studies that lacked clinical validation or used ICD coding to quantify health outcomes were considered high risk of detection bias. In contrast, those lacking representative research populations were considered to be at high risk of selection bias. Lastly, publications that did not account for at least three major confounding variables, seasonality, weather, influenza, long-term trends, and demographic and lifestyle factors, were given a high risk of bias.
Results
Different studies on air pollution that affect respiratory health in different ages and countries have been searched by the systematic review. Many studies assessed O3, NOx, and PM10 on COPD and asthma symptoms in developed countries and China but none have reviewed these three pollutants O3, NOx, and PM10 effect on COPD and asthma in Nigeria. This research aimed to research the effects of ozone, particulate matter, and nitrogen oxides on respiratory health in Nigeria. The Discover, PubMed, Google Scholar, and Web of Science databases were utilized to retrieve relevant papers [15]. The search queries included keywords identified in current published systematic reviews (Orellano et al., 2017). The consolidated results of the search queries were then filtered by introducing exclusion and limitation components.
General findings on effects of O3, PM10, and NOX on Respiratory Health in Nigeria
Ozone (O3)
Through oxidative damage and inflammation, ozone is known to induce a bronchial inflammatory response and airway hyper-responsiveness, as seen in most studies reviewed. Even though air pollutants like PM10 and NOx have shown declining trends in average concentrations in recent years in Nigeria and other parts of the world, ozone concentrations have not. In many parts of the globe, short-term exposure to high levels of ozone has been linked to increased death rates and respiratory problems [6,12,29], Due to the difficulties in modelling ozone exposure and connecting individual exposures to health outcome data, the long-term impacts of ozone have received less attention than the short-term effects. Long-term ozone exposure has been linked to an elevated risk of respiratory death, according to [29]. Several studies also linked long-term ozone exposure to a worsening of lung function and the development of emphysema. The following studies confirmed that ozone had a great influence on respiratory health [6,28,29].
PM10
There is compelling evidence that short-term exposure to PM10 causes respiratory difficulties, but PM2.5 is a greater risk factor for mortality than the coarser PM10, especially when exposure is prolonged [16]. Susceptible populations, such as those with a pre-existing heart condition, the elderly, and youngsters, are more vulnerable. Exposure to PM, for example, affects children’s lung development, impairments in lung function and decreased overall lung growth, leading to a long-term lung function deficit [11]. Orellano et al., 2017). There is no evidence of a safe amount of exposure or a level below which there are no negative health consequences, from the studies reviewed. The fact that the exposure is both widespread and involuntary adds to the importance of this health factor. There is currently insufficient data to distinguish variations in the impacts of particles with diverse chemical compositions or originating from distinct sources at the population level. However, the evidence supporting the dangers of ignition PM is more robust than for PM from other sources. Numerous chemical compounds, including PM which are known carcinogens are now believed to play a role in health effects associated with black carbon in PM, especially respiratory health Schreiber [3,12,17].
NOX
Inhaling air with a high concentration of nitrogen oxides can irritate an individual’s respiratory system airways. Short-term exposures may aggravate respiratory illnesses, especially asthma, resulting in respiratory symptoms and hospital admissions. Exposure to higher nitrogen oxides for longer periods of time may influence the development of asthma. PM10 and ozone are formed when oxides of nitrogen (NOx) and other hydrocarbon combine with other substances in the air. Both are toxic when breathed, owing to their impacts on the respiratory system. [12,17] showed how nitrogen oxides contribute to respiratory complications.
Effects of PM10, O3, and NOX on Different Populations
Although ozone is linked with unfavorable health effects, little is documented about vulnerable groups or sensitive populations. However, a study conducted by [18] showed that children diagnosed with bronchiolitis and bronchopneumonia in 98 Homes in Lagos Nigeria were exposed to average concentrations of CO, SO2, and benzene [18] added from the findings in their study using senior secondary school students, that cough and asthma are most frequently reported with more than 10% bronchitis prevalence from traffic and open burning air pollution. Also, [19] showed that particle matter exposure is more likely to harm those with heart or lung problems, children, and older individuals. Moreover, several studies reviewed those individuals with asthma, children, and the elderly, are at a higher risk of adverse health consequences from nitrogen oxides [14,20,21].
Previous Studies in Nigeria
Emissions from vehicles, solid waste incineration, and industrial pollutants all contribute to Nigeria’s poor air quality, according to the WHO. Pollution levels in Nigeria vary seasonally according to the [22,23] WHO, (2014 & 2015) with the greatest levels occurring during Nigeria’s dry season, which is usually from November to March. The cities of Onitsha, Umuahia, Kaduna, and Aba all have persistently serious air pollution [24]. Environmental health hazards are becoming a major issue in Nigeria as a result of a variety of environmental problems, including air pollution, flooding, water pollution, oil spills, erosion, deforestation, and desertification [25]. Significant environmental factors include ambient air pollution, home air pollution, and water, hygiene, and sanitation, all of which have been declining over an extended period of time [25]. In comparison, PM10 pollution, lead exposure, and ozone pollution all show a continuous increase in their association with mortality and disability-adjusted life years (DALYs) in Nigeria, suggesting a serious issue in an ecological health-related risk scenario. As a result, ecologically sustainable economic practices and policies should be considered critical for the public and policymakers to improve population health in Nigeria.
The discoveries of [26] contribute to the scant existing research on the detrimental respiratory health effects of ambient air pollution on city transport operators in certain Nigerian cities. Other confounding variables working synergistically to produce a more severe and harmful impact are self-evident. The findings have significant policy implications aimed at decreasing urban ambient air pollution, including improved air quality management [26]. This may involve the creation of a central pollution management board, the monitoring of individual exposure in order to assess the health effects of air pollution, and the avoidance of construction in cities with high levels of air pollution.
Discussion
In 2012, air pollution claimed 3 million lives, accounting for 5.4 percent of all fatalities worldwide. In the same year, about 25 percent of respiratory infection fatalities were caused by lung cancer, 8 percent by chronic obstructive pulmonary disease (COPD), and approximately 18 percent by respiratory infection induced by air pollution [27]. According to one study, the effect of air pollution on premature deaths in Nigeria may double by 2050 [28] (Bauer et al., 2019). A 10μ/m-3 rise in PM10 resulted in a significant rise in COPD mortality and exacerbations that may be significantly decreased via air pollution management [17]. Cohort research in China found that the risks of death and years of life lost were directly related to the ambient concentrations of air pollution [16]. Therefore, to safeguard the respiratory public’s health and individuals with chronic respiratory illnesses in Nigeria, the establishment of long-term regulations for ozone and PM should be considered.
Gaps in Literature
Only a few studies included critical analytic components, such as specific components that have been associated with a higher risk of disease/mortality compared to other chemicals found in these should be included in future research. Additionally, few studies included either of the three air pollutants (NOX, O3, and PM10) in a single publication. Moreover, most papers did not do deep analyses of the effects of the pollutant on respiratory health. The few studies that accounted for the impact of the pollutants on respiratory health had very limited data on the population and pre-existing health conditions such as asthma. On a more positive note, some studies [4,6,12,16,17,28,29] examined the effects of NOX, O3, and PM10 on respiratory health. However, none of these studies examined the effect of these pollutants (NOX, O3, and PM10) o respiratory health patients in Nigeria.
Implications and Recommendation
As seen from this review, air pollution has the potential to harm the health of the general population, and be particularly harmful to children, the elderly, and people with pre-existing cardiovascular or respiratory conditions. Measures to decrease environmental air pollution should be considered. The arguments for action to decrease air pollution may take various forms, including urban planning, technical advancements (e.g. banning the use of leaded petrol, open burning, proper waste management, designing of lower emission cars), the implementation of warning systems, and new policies. This approach must operate at the population level in Nigeria, with precautionary policies, as well as at the interpersonal level, by educating and informing the vulnerable population about how to reduce their exposure to the discussed pollutants (O3, PM10, and NOX). Some health advantages may be achieved at the population level in Nigeria by enacting particular policies, such as congestion charges in major cities and ending open solid waste burning. However, before spending large sums of public money on ineffective preventive initiatives, determining the impact on human health of exposure to major air contaminants in different states is crucial as different states suffer from different air pollutants in Nigeria such as the case of soot in Rivers state [29-32] Other frequent causes of pollution should also be considered such as living with a smoker, or open burning, for example, exposes a person to toxicant levels similar to those seen in a highly polluted city [33-49]. To safeguard the respiratory public’s health and individuals with chronic respiratory illnesses in Nigeria, the establishment of long-term regulations for ozone and PM should be considered.
Conclusion
The findings of this study demonstrate the effect of O3, PM and NOx and how research activity is engaging with the global air pollution crisis. Additionally, the research activity reflects the degree to which Nigeria has responded responsibly to this global issue. NGOs should utilize such research to compel politicians and political campaigns in Nigeria to adopt environmental and industrial objectives aimed at improving air quality. Nations with high levels of air pollution and thus poor air quality should invest in research in this area to give health authorities a foundation for better action. Establishing national and regional research centers to monitor air quality and air pollution is critical to providing evidence for action. These institutes may bring together experts from various fields to cooperate on translating research findings into national goals and policies. At the national level, nations must implement stringent air quality standards. Industries and health authorities must collaborate to adopt steps that substantially decrease particulate matter, oxides of nitrogen, and ozone levels. Because air pollution is a worldwide hazard to public health, research collaborations between developed and developing countries with high levels of air pollution must be strengthened. Finally, since air pollution has a respiratory impact on the general public and especially those with underlying respiratory conditions such as COPD and asthma there is a need to educate and raise public knowledge about this problem.
References
- Singh N (2020) Air Pollution Exposure Studies Related to Human Health. In Air Pollution and Environmental Health p. 141-177.
- Global Burden of Disease (2019) Viewpoint Collaborators. Five insights from the Global Burden of Disease Study pp. 1135-1159.
- Martins V, Faria T, Diapouli E, Manousakas MI, Eleftheriadis K, et al. (2020) Relationship between indoor and outdoor size-fractionated particulate matter in urban microenvironments: Levels, chemical composition and sources. Environmental Research 183: 109203.
- Ohlwein S, Kappeler R, Joss MK, Künzli N, Hoffmann B (2019) Health effects of ultrafine particles: a systematic literature review update of epidemiological evidence. International Journal of Public Health 64(4): 547-559.
- Wambebe NM, Duan X (2020) Air Quality Levels and Health Risk Assessment of Particulate Matters in Abuja Municipal Area, Nigeria. Atmosphere 11(8): 817.
- Fares S, Conte A, Chabbi A (2018) Ozone flux in plant ecosystems: new opportunities for long-term monitoring networks to deliver ozone-risk assessments. Environmental Science and Pollution Research25(9): 8240-8248.
- Kumagai K, Lewandowski R, Jackson-Humbles DN, Li N, Van Dyken SJ, et al. (2016) Ozone induced nasal type 2 immunity in mice is dependent on innate lymphoid cells. Am J Respir Cell Mol Biol 54(6): 782-791.
- Yang Q, Ge MQ, Kokalari B, Redai IG, Wang X, et al. (2016) Group 2 innate lymphoid cells mediate ozone-induced airway inflammation and hyperresponsiveness in mice. J Allergy Clin Immunol 137(2): 571-8.
- Bromberg PA (2019) Mechanisms of the acute effects of inhaled ozone in humans. Biochim Biophys Acta 1860: 2771-2781.
- Mumby S, Chung KF, Adcock IMTranscriptional effects of ozone and impact on airway inflammation. Front Immunol 10: 1610.
- Chen TM, Gokhale J, Shofer S, Kuschner WG (2007) Outdoor air pollution: nitrogen dioxide, sulfur dioxide, and carbon monoxide health effects 333(4): 249-256
- Orellano P, Reynoso J, Quaranta N, Bardach A, Ciapponi A, et al. (2020) Short-term exposure to particulate matter (PM10 and PM2. 5), nitrogen dioxide (NO2), and ozone (O3) and all-cause and cause-specific mortality: Systematic review and meta-analysis. Environment International 142: 105876.
- Manucci PM, Franchini M (2017) Health effects of ambient air pollution in developing countries. Int J Environ Res Public Health 14(9): e 1048
- Manisalidis I, Stavropoulou E, Stavropoulos A, BezirtzoglouE (2020) Frontiers in public health 8: 14.
- AlRyalat SAS, Malkawi LW, Momani SM (2019)Comparing bibliometric analysis using PubMed, Scopus, and Web of Science databases. JoVE (Journal of Visualized Experiments) 24: 152.
- Zhang Y, Peng M, Yu C, Zhang L (2017) The burden of mortality and years of life lost due to ambient PM10 pollution in Wuhan, China. Environmental Pollution 230: 1073-1080.
- Zhang Z, Wang J, Lu W (2018) Exposure to nitrogen dioxide and chronic obstructive pulmonary disease (COPD) in adults: a systematic review and meta-analysis. Environmental Science and Pollution Research 25(15): 15133-15145.
- Ana G, ShendellD, Odeshi T ,Sridhar M (2009) Identification and Initial Characterization of Prominent Air Pollution Sources and Respiratory Health at Secondary Schools in Ibadan, Nigeria 46(7): 670-676
- Schreiber M (2018) A skeptical view on the Hirsch index and its predictive power. Physica Scripta 93(10): 102-501.
- Tiotiu AI, Novakova P, Nedeva D, Chong-Neto HJ, Novakova S, et al. (2020) Impact of Air Pollution on Asthma Outcomes. International journal of environmental research and public health 17(17): 6212.
- Santos UP, Arbex MA, Braga A, Mizutani RF, Cançado J, et al. (2021) Environmental air pollution: respiratory effects. Jornalbrasileiro de pneumologia :publicacaooficial da SociedadeBrasileira de Pneumologia e Tisilogia 47(1): e20200267.
- WHO (2015) Le a d Po is o n i n g in Nigeria fweb.int/report/Nigeria/lead-poisoning Nigeria - 15- May - 2015
- WHO (2014) 7 Million premature deaths linked to air pollution, WHO March 2014.
- Urhie E, Afolabi A, Matthew O, Osabohien R, Ewetan O, et al. (2020) Economic growth, air pollution and health outcomes in Nigeria: A moderated mediation model. Cogent Social Sciences 6(1): 1719570.
- Pona HT, Xiaoli D, Ayantobo OO, Tetteh ND (2021) Environmental health situation in Nigeria: current statusand future needs. Heliyon 7(3): e06330.
- Ekpenyong CE, Ettebong EO, Akpan EE, Samson TK, Daniel NE, et al. (2012) Urban city transportation mode and respiratory health effect of air pollution: a cross-sectional study among transit and non-transit workers in Nigeria. BMJ Open 2(5): e001253.
- Lelieveld J, Klingmüller K, Pozzer A, Pöschl U, Fnais M, et al. (2019) Cardiovascular disease burden from ambient air pollution in Europe reassessed using novel hazard ratio functions. European heart journal 40(20): 1590-1596.
- Mohajan HK (2017) Two criteria for good measurements in research: Validity and reliability. Annals of Spiru Haret University. Economic Series 17(4): 59-82.
- Fagbeja M, Chatterton T, Longhurst J, Akinyede J, Adegoke J, et al. (2008) Air pollution and management in the Niger Delta - Emerging issues. WIT Transactions on Ecology and the Environment p. 116.
- Ana G (2011) Air pollution in the Niger Delta area: Scope, challenges and remedies. Intech open p. 182-200
- Yakubu O (2018) Particle (Soot) Pollution in Port Harcourt Rivers State, Nigeria—Double Air Pollution Burden? Understanding and Tackling Potential Environmental Public Health Impacts.
- Whyte M, Numbere T, Sam K (2020) Residents’ perception of the effects of soot pollution in Rivers State, Nigeria. African Journal of Environmental Science and Technology.
- Qasim H, Alarabi AB, Alzoubi KH, Karim ZA, Alshbool FZ et al. (2019) The effects of hookah/waterpipe smoking on general health and the cardiovascular system. Environmental Health and Preventive Medicine 24(1): 1-17.
- Abubakar IR, Dano UL (2018) Socio-economic challenges and opportunities of urbanization in Nigeria. In urbanization and its impact on socio-economic growth in developing regionp pp. 219-240.
- Bauer SE, Im U, Mezuman K, Gao CY (2019) Desert dust, industrialization, and agricultural fires: Health impacts of outdoor air pollution in Africa. Journal of Geophysical Research: Atmospheres 124(7): 4104-4120.
- Bell M L, Zanobetti A, Dominici F (2014) Who is more affected by ozone pollution? A systematic review and meta-analysis. American Journal of Epidemiology 180(1): 15-28.
- Byrne A (2017) Trouble in the Air: Recent Developments under the 1979 Convention on Long‐Range Transboundary Air Pollution. Review of European, Comparative & International Environmental Law 26(3): 210-219.
- EmbersonL (2020) Effects of ozone on agriculture, forests, and grasslands. Philosophical Transactions of the Royal Society.
- Health Effects Institute (2020) State of Global Air 2020. Special Report. Boston, MA: Health Effects Institute.
- Lekwot V, Dayaji L, NwokediriohaO (2013) Public Health Effects from Vehicular Emissions In Kaduna Metropolis, Kaduna State, Nigeria.
- McCullough SD, Dhingra R, Fortin MC, Diaz-Sanchez D (2017) Air pollution and the epigenome: a model relationship for the exploration of toxicoepigenetics. Current Opinion in Toxicology 6: 18-25.
- Newell K, Kartsonak C, Lam KBH, Kurmi OP (2017) Cardiorespiratory health effects of particulate ambient air pollution exposure in low-income and middle-income countries: a systematic review and meta-analysis. The Lancet Planetary Health 1(9): 368-380.
- Nwachukwu A, ChukwuochaE, Igbudu O(2012) A survey on the effects of air pollution on diseases of the people of Rivers State, Nigeria.
- Nwachukwu AN, Ugwuanyi JU (2010) Air pollution and its possible health effects on rural dwellers in Rivers State, Nigeria. Afr J Phys 3: 217-240.
- Oguntoke O, Adeyemi A (2017)Degradation of urban environment and human health by emissions from fossil-fuel combusting electricity generators in Abeokuta metropolis, Nigeria.
- Oguntoke O, Yussuf A (2008) Air Pollution Arising from Vehicular Emissions and The Associated Human Health Problems in Abeokuta Metropolis, Nigeria.
- Pinichka C, Makka N, Sukkumnoed D, Chariyalertsak S, Inchai P, et al. (2017) The burden of disease attributed to ambient air pollution in Thailand: A GIS-based approach. PloS One 12(12): 189- 909.
- Rybarczyk Y, Zalakeviciute R (2018) Machine learning approaches for outdoor air quality modeling: A systematic review. Applied Sciences 8(12): 2570.
- SweilehWM (2020) Bibliometric analysis of global scientific literature on vaccine hesitancy in peer-reviewed journals. BMC Public Health 20(1): 1-15.
Editorial Manager:
Email:

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...