Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6695
Research Article(ISSN: 2637-6695) 
Aspects Of Sexual Consequences in Women Undergoing Anti-Hormonal Breast Cancer Therapy Volume 3 - Issue 1
Mary Zapczynski*, Cheryl Adair
- Assistant Professor Northwestern State University of Louisiana, College of Nursing and School of Allied Health, USA
Received: April 22, 2021; Published: April 29, 2021
Corresponding author: Mary Zapczynski, DNP, APRN, FNP-BC Assistant Professor Northwestern State University of Louisiana, College of Nursing and School of Allied Health, 1800 Line Avenue, Shreveport, Louisiana 71101
DOI: 10.32474/LOJNHC.2021.03.000155
Abstract
Breast cancer (BC) is the most frequent form of female cancer with a global annual incidence of 2.4 million. Sexuality and sexual distress after breast cancer are a common and complex phenomenon not yet fully understood. The aim of the present study was to explore long-term sexual consequences after adjuvant endocrine breast cancer therapy and the strategies used to manage these consequences. This qualitative and descriptive focus group study included 45 women mean age 57.7 (36 - 77) from Region Stockholm, Sweden. Inclusion criteria were ongoing adjuvant endocrine BC therapy started within the past seven years and the ability to speak and understand Swedish. After eight focus group interviews were conducted saturation was reached. Qualitative content analysis with an inductive approach revealed five themes:
a) Decreased or absent sexual desire
b) Reasons for changed sexual desire.
c) Reactions to changes in sexual desire.
d) Relations to a partner.
e) Strategies to manage sexual dysfunctions.
The results deepen the understanding of sexuality after BC. We conclude there is a real need for compulsory education in sexology/sexual medicine for healthcare professionals meeting women with BC and moreover, sex therapists need to be trained to meet women with BC.
Keywords: Breast Cancer, Adjuvant Endocrine Therapy, Sexual Dysfunction, Sexual Desire, Genital Sexual Pain, Healthcare Professionals
Introduction
Worldwide, breast cancer (BC) is the most frequent form of cancer among women. The present global annual incidence is 2.4 million [1]. In Sweden breast cancer is responsible for one-third of all cancer cases in women; in 2018 more than 7,800 women were diagnosed with BC and about a third of them were aged 59 years or younger (The National Board of Health and Welfare, 2019). Survival has substantially increased over the last decades, with over 70% surviving at least ten years following diagnosis in countries with advanced medical care as in Sweden [1]. The improved prognosis is mainly due to screening strategies that detect breast cancer at an earlier stage and more effective multimodal treatment regimens including surgery, radio- and systemic therapies that substantially reduce the risk of dying [2]. Women who have undergone breast cancer surgery and have a hormone receptor-positive tumour are offered adjuvant endocrine breast cancer therapy (AET) for five to ten years to reduce the risk of recurrence. Menopausal side-effects caused by AET are common and often result in distress with a negative impact on satisfaction with life [3,6]. Sexuality and sex- ual distress are complex phenomena. It is not just AET that affects sexuality after BC. In studies where sexually related problems were investigated, irrespective of treatment modalities, several of them found sexual dysfunctions to be common after breast cancer. There are, however, quite large differences regarding the prevalence; for example decrease in sexual interest/desire varied between 24% - 71% [7,11] arousal and lubrication dysfunctions 51% - 74% [7,10- 11], genital sexual pain 39% - 51% [7,9,11]. Moreover, a decrease in sexual satisfaction/low sexual satisfaction has been reported to exist in 54% - 71% [10-12].
Other areas of sexually related concerns among women with BC have been reported regarding poor body image and feelings of being less feminine [13-15]. Furthermore, aspects of being partnered or single affect sexuality for these women. In follow-up studies partnered women have been found to be more sexually active than single women who, on the other hand, showed fewer sexual dysfunctions [8,16] and were less distressed about their sexuality [8]. However, in an Australian study as many as 57% of single women felt that BC had a negative impact on sexuality with worries of being less attractive, rejected, and undesirable [10]. In spite of the high numbers of sexual dysfunctions “only” 33% of partnered women with BC have been found to be unsatisfied with their sexual relationship [7]. The aim of the present study was to explore women´s perceived long-term sexual consequences after adjuvant endocrine breast cancer therapy and the strategies they use to manage these consequences.
Subjects and Methods
The present qualitative and descriptive study is one part of a project regarding the experience of menopausal side-effects during AET and strategies to deal with them. The project involved four hospitals in Region Stockholm, which is the most densely populated area in Sweden. The research team consisted of representatives from several professions: oncologists, nurses, a sexologist, and a medical social worker. The team created an interview guide aimed at achieving the goal of the study. The guide was based on results from a study of medical records [17], literature findings, clinical experiences, and discussions in the research group.
Participants
Participants were recruited via flyers placed in the waiting areas of the oncology clinics at the hospitals and with help from the Breast Cancer Association which informed its members about the study by email. Those who were interested contacted the first author for further verbal information and informed consent. To be considered for inclusion, women needed to be undergoing current adjuvant endocrine BC therapy started within the past seven years. Furthermore, they needed to be able to speak and understand Swedish. Exclusion criteria were prior breast cancer treatment. A total of 68 women from Region Stockholm, Sweden showed interest in participating in the study. Three women did not meet the inclusion criteria due to prior breast cancer treatment. At the time of the interviews, four were no longer interested, and 16 were unable to attend the specific focus group they were invited to. Thus, a total of 45 women were included. In the verbatim quotations below, each woman is given a group and an individual number; age is noted as either under 50 years (50-) or 50 years or more (50+).
Interview procedure
Eight focus groups were organised with four to nine women (median: five women) in each group. By selecting participants with different experiences, the opportunity to elucidate the research question from different aspects increases [18]. In five of the groups, the women were invited to specific meetings based on their age and whether they had received chemotherapy. The matching was done to increase homogeneity and to facilitate discussion [19]. The interviews were conducted from October 2013 to January 2014. The interviews were completed as described by Krueger [19] who suggested the inclusion of a moderator and an assistant moderator. The task of the moderator is to facilitate the discussions, invite the participants to speak, and encourage the members to participate in the discussions. The interviews were moderated by the first author and the second author was the assessor during four of the interviews. The interviews lasted 90 minutes, which included a 15-minute break. All interviews were conducted in Swedish.
Data analysis
After eight conducted focus group interviews the research group found that saturation was reached and therefore no new group interviews were initiated. All interviews were tape-recorded and transcribed verbatim. After achieved saturation a qualitative content analysis with an inductive approach was used; described by Patton [18] and Graneheim and Lundman [20]. The qualitative content analysis focuses on the interpretation of texts and the inductive approach involves an unconditional analysis of texts, for example, people’s narratives about their experiences [20] (Graneheim and Lundman, 2004). In order to identify differences and similarities in the interviews, the transcript was analysed Lundman’s and Hällgren Graneheim’s recommendations [21]. Thus, the transcribed text was divided into meaning units. These meaning units were condensed and then abstracted into a code describing the contents of the meaning unit. Codes with similar content are merged into themes and sub-themes.
Ethics
The ethical procedures followed in the study are in accordance with the Helsinki Declaration. The study was approved by the Regional Ethical Review Board in Stockholm County in 2013. Before the interviews, all participants signed informed consent.
Results
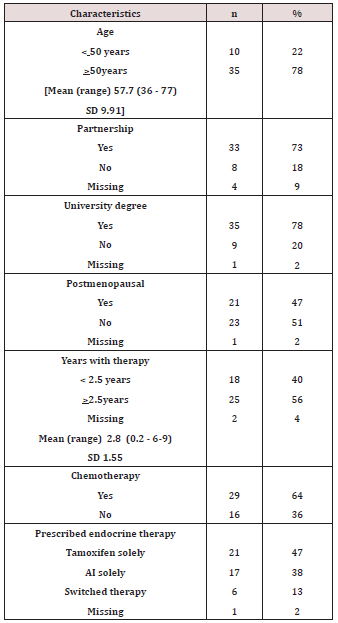
Sociodemographic and clinical characteristics are presented in Table 1. The women’s ages ranged between 36 and 77 years (mean age 57.7 years). A majority of them were living with a partner. Most of them had a university degree. Nearly half of the women (48%) were post-menopausal. The mean time for AET was 2.8 years (range 0.2 - 6.9 years), 64% had had chemotherapy and all endocrine therapy.Data from the focus groups revealed five themes: 1) Decreased or absent sexual desire; 2) Reasons for changed sexual desire; 3) Reactions to changes in sexual desire; 4) Relations to a partner; 5) Strategies to manage sexual dysfunctions.
Table 1: Sociodemographic and clinical characteristics among 45 women treated with endocrine breast cancer therapy.
Decreased or Absent Sexual Desire
The theme ‘Decreased or Absent Sexual Desire’ was frequently discussed in the focus groups as many of the women experienced a decreased or absent sexual desire due not only to endocrine therapy but also to surgery and/or chemotherapy. Both the younger and the older women described absent sexual desire, but these descriptions were more frequent in focus groups with participants younger than 50 years. Moreover, some women said that their sexual desire had already ceased upon receiving their cancer diagnosis. The women used words like ‘finished’, ‘nothing’, and ‘gone’ when they discussed their present desire. One woman described the loss in the following way `Yes, I was not prepared for it [absence of sexual desire], being like this I can tell you, and I am married and have had a healthy sex life. I have absolutely no desire for sex anymore[. . .] But I think about it like this, it’s a bit like you see “honey dishes”, favourite dishes, all laid on a table. What, fun! It looks great, but while, everybody else can eat, you only want a glass of water. It’s just gone! ’(S8:1, 50+).
Reasons for Changed Sexual Desire
The reasons the participants gave for the absent or decreased sexual desire can be summarised as genital sexual pain and/or changed feelings about their femininity.
Genital Sexual Pain
Several women reported that vaginal dryness had led to decreased sexual activity due to painful intercourse. Two women stated frankly that if it hurts when you are trying to have sex, the desire will disappear and sexual activities will be dissatisfying: ’Yes, I think this is really hard. It´s been so dry that if you want to have sex, or you have sex, it just ends up being painful[. . .] It is no fun!’ (S8:2, 50+)
Changed Feelings about Femininity
Many women described their femininity to be negatively altered or even lost due to completed and ongoing BC treatments. This change led to an experience of disrupted life, and many women no longer recognised themselves as a ‘woman’. Some women reported that the injuries from breast surgery, especially a lost or deformed breast, affected their sexuality. The loss of a breast made the women feel less attractive and less comfortable with their bodies. One woman who had undergone a mastectomy and was now on endocrine therapy summed up her feelings about her femininity as follows:‘I have become so ugly. I have so much fluid in the body overall and everywhere; yes, I do not want to show myself’ (S1:3, 50-). Several women described how not feeling attractive affected their sexual desire: ‘I am also totally uninterested in any kind of sex life and then I think it is related to me feeling not attractive anymore’ (S8:4, 50+).
Reactions to Changes in Sexual Desire
Several of the women said they missed their sexual desire and that the loss or decrease also negatively affected their overall life satisfaction. The absence of sexual desire was something that the women felt they had to address: `Since I started with chemotherapy in January 2012, I have had no sex life at all because I have no sexual desire. And that’s very boring. Of course, it’s a disappointment that you must deal with it in some way. And it’s not so funny when you’re married ’(S2: 4, 50-)’ Many were disappointed that there was so little help available: `It’s so hard that it has become like this and that there is no help. I have gone to both gynaecologists and doctors and then they say I can use oil or something. But that’s not good! It will not be good! So it is – you are a little mutilated’ (S4:5 50-). However, many women stated that, taken into account that cancer is a deadly/a life-threatening disease, they accepted the side-effects of menopause problems and sexual dysfunctions as a worthwhile price to be paid during the treatment period. Several women expressed the hope that their sexual desire would return when the endocrine therapy was completed. Two of these women had heard from others that this usually happens.
Relations to a Partner
Being in a Partner Relationship
Several women reported that they had a caring partner, and this caring was especially evident after the diagnosis and during chemotherapy: ‘I discovered a new side of my husband, actually, the caring side[. . .] It´s almost like a parent to child role’ (S1:3, 50+). Most of these partners understood the woman’s lack of sexual feelings although some of them had expressed that they missed woman’s sexual desire. Only one woman talked about her partner as being irritated by the changes in their sexual life. Many women in the focus groups emphasised the importance of talking to their partner about their sexual discomfort and the sexual problems following the cancer treatment. Furthermore, two women pointed out that they felt guilty about their lack of sexual desire resulting in absence of intercourse: `Yes, I can say [. . .] I am married and have had a healthy sex life [before], you could say. Now, I have absolutely no desire for sex. I have tried to explain this to my husband. He is great and understanding, and it’s just a bitter pill to swallow realising it is so’ (S8: 2, 50-).The importance of an understanding partner was also noted: `It is fortunate to have a relationship [partner] who accepts you as you are; otherwise, it would never work. There would have been a divorce because it [sex] is not on the map. It’s really hard that you cannot [have sex]. And it’s no use pretending because it’s not’ (S8:2, 50+)
One woman stressed that it was problematic that her husband reacted negatively to her bodily changes and especially the fear he felt when confronted by her operated breasts: `I want to have support from my husband [. . .] I want to feel like a woman too. Oh, they are the way they [the breasts] look (S1:2, 50-) Some of the elderly women reported that factors related to their partner’s health also affected their own sexual desire and sexual life. Two of these women had partners who had been diagnosed with severe diseases (e.g., diabetes) shortly before the women’s BC diagnoses; this was experienced as a further obstacle to sexual desire and sexual activities: `The old guys are not so alert either’ (S7:1, 50+)
Being Single
Some of the women were not in a relationship with a partner. Two single women stated that they had sex after the BC treatment. One described her sexual function to be unaffected (i.e., her sexual activity was as before being diagnosed with BC). The other thought she had no desire left but when having intercourse with a man she trusted, it helped her to find her way back to her sexuality: `When I was completely knocked down, there was now nothing left, but then I got very, very lucky [. . .] one of my old partners re-appeared [. . .] it was absolutely amazing [. . .] the lust was there [. . .] Now I’ve come back. It was enough because there was such confidence between us; he could help me because we had such a long relationship before’ (S2:1, 50-). Other women felt that the altered body and the changing experience of their sexuality made it impossible to start a new relationship. One woman expressed hope that if she met a partner, and there was a mutual attraction, then a solution to any sexual complications would arise. Two single women reported that before being diagnosed with BC they were not sexually active. Both of them stated that AET did not mean any changes in their experiences of sexuality.
Strategies to Manage Sexual Dysfunctions
Strategies to Manage the Changed Sexual Desire
The women experienced healthcare providers as non-supportive with respect to the aspect of decreased sexual desire. They found that they were largely left to themselves to find solutions. These women had different strategies for managing their decreased or absent sexual desire such as using lubricants, carefully examining what helps, and having sex without penetration. Two women in one of the focus groups described low sexual desire as a barrier they must overcome to make sexual life possible: `It’s probably a threshold that you have to overcome. Oh, once you’ve got over it [. . .] I have done it myself. It’s probably more psychological for me ’(S2:3, 50). For these women, it was important to be confirmed that they still functioned physically, and both claimed that they needed more time to recover psychologically.
Strategies to Manage Genital Sexual Pain
Vaginal dryness was described as an obstacle leading to genital sexual pain (GSP) and no sexual satisfaction. Different strategies to manage this problem existed and many of the women contacted healthcare providers for help. Some turned to a gynaecologist for assistance with their vaginal dryness issues. Sometimes they sought this help after recommendations from their oncologists and others took their own initiative to meet with a gynaecologist they already had a patient/physician relationship with. Many women perceived that the assistance from the healthcare providers was insufficient and contradictory and therefore they tried to find their own solutions to the problems. On their own initiative, some women took medication not containing oestrogen such as herbal medicines containing phytoestrogens and some women used different overthe- counter oils or creams or changed the endocrine drugs after consultation with an oncologist. During the interviews, the women both listened very actively to each other, and spontaneously gave each other advice.
Overall Statement
Some women stated that they were convinced that a cancer diagnosis, its treatment, as well as the physical and psychological side-effects, including feelings of being unattractive, losing one’s femininity, and experiencing decreased or absent sexual desire, are interrelated. Moreover, they expressed that the BC surgery and the treatment that followed resulted in losing their identity as sexual beings.
Discussion
The principal finding of this investigation is that sexuality has to be acknowledged as an area of importance for women with a breast cancer diagnosis. In consensus with others (for a review see (Male et al., 2016) [14] we found sexuality to be negatively affected not only in terms of sexual dysfunctions but also regarding aspects of decreased experiences of femininity, attractiveness and being in a relationship or not. It wasn’t only adjuvant endocrine therapy that had a negative effect on women´s sexuality, breast surgery and chemotherapy did so too. Women rarely found that the healthcare system provided information about sexual consequences and, furthermore, they felt the healthcare system was not supportive as there was a lack of consensus and knowledge on issues regarding therapy for sexually-related problems after breast cancer treatment [22,23]. The partner is, in one way or another, affected by the woman’s disease and sexual experiences. There are, however, some contradictory findings when it comes to the impact of being in a relationship - or not - and sexual consequences after BC. Unchanged partner relationship has been reported to occur in 67% [12] and Ussher et al. [10] found half of their investigated women communicated with the partner about sexuality but only seven percent stated an increased communication within the partnership after BC. In the present study, a partner’s own serious diseases and old age also negatively affected women´s sexual life. In these couples, it is likely that women and men´s sexual dysfunctions occur simultaneously [24]. Partners could also experience fear in relation to the woman’s changed body. The relationship dynamics can be of decisive importance for the success of treatment. Fear of pain, partner avoidance, and distracting factors are some aspects that may be areas to acknowledge in the case history and in treatment [25]. Furthermore, in the present study, some women expressed feelings of guilt due to lack of sexual interest, thereby excluding their partner from intercourse. Having a partner, his/her reaction to cancerrelated emotional distress is essential for perceived satisfaction within the relationship. If a partner uses approach-oriented coping strategies, the woman’s partnership satisfaction increases but when a partner uses avoidance strategies satisfaction decreases [26-27]. Single women with BC need attention concerning sexual issues as well. In agreement with others [8,16] we found that these women were less sexually active and had fewer sexual dysfunctions and problems than those in a relationship. One can speculate as to whether the occurrence of fewer dysfunctions might be a result of less sexual activities [10]. Ussher et al. [10] found 57% of single women with BC expressing that the cancer had a negative impact on their sexuality; feeling unattractive and undesirable, and fearing rejection. A few women in the present study had experiences like that but there were also some expressions of hope for a satisfying relationship and sexual life in the future.
Regarding clinical aspects of sexual issues in women with BC, we suggest attention directed towards treatment strategies equivalent to sexual complaints among women without BC. That is, starting with medical evaluation and sexological case-history, leading to a sexological diagnosis and thus, possibilities for adequate treatment strategies[10,25,28] According to the International Classification of Diseases ICD 11 (WHO, 2018), the following diagnoses are associated with BC treatment: hypoactive sexual desire dysfunction, sexual arousal dysfunction, and genital sexual pain/dyspareunia. Interestingly, the number of and the order of the dysfunctions were found in different combinations among the women with BC. That is, some women started with decreased or absent sexual desire that resulted in arousal disorder with genital sexual pain, and some women started with genital sexual pain as the primary (i.e., first) dysfunction that resulted in decreased/ absent sexual desire. For the majority, however, genital sexual pain and sexual arousal disorder seemed to be the first dysfunctions to occur during the endocrine treatment and were difficult to tell apart. In agreement with others, this leads us to the conclusion that individual aspects with a multi-professional approach have to be considered in the meeting with women with BC [15,22,30]. It can be noted that none of the participating women mentioned orgasmic function/dysfunction, either before or after BC. As we have been able to locate only one study [11] regarding orgasmic function in women with BC the present finding may not be surprising.
On the other hand, these authors [11] found as many as 42% reporting orgasmic dysfunction. As the aetiology of sexual desire dysfunction, as well as GSP, are complex, a comprehensive multidisciplinary approach is necessary both for evaluation and treatment [25,31]. This recommendation is supported by the present study and seems, not least, important when it comes to women who have and have had breast cancer. Physical conditions that could cause genital sexual pain for women who have had breast cancer can be related to chemotherapy and endocrine therapy [7,11]. Therefore, we conclude that mucosal disorders cause genital pain due to oestrogen deficiency. A finding that further emphasises the importance of including sexual issues in the care of women with breast cancer.
Sexual desire and genital function can be regarded as necessary parts of sexual satisfaction, but this is an incomplete picture. Basson’s model for female sexual response [32] is used here to understand women’s expressed sexuality after breast cancer, particularly as we prefer to view sexuality from a holistic perspective. Thus, there are intimacy needs that have to be fulfilled for acceptable sexual satisfaction to be achieved. For example, Muise et al. [33] found that being sexual/reaching out for sexual activities due to the wish to feel close and bond to a partner increases satisfaction with a partner relationship and with sexual life. Basson’s model [32,34] shows that women need to make conscious and motivational choices to be receptive to different kinds of sexual stimuli that can lead to sexual desire and sexual arousal. For example, two women in the present study viewed their decreased sexual desire as a barrier they had to overcome to find their sexuality again. However, the present study confirms earlier investigations showing the complex interaction between not only different sexual dysfunctions but also other areas such as partner aspects, decreased femininity, and body changes leading to feelings of unattractiveness [9,13-15] The women used different strategies to recover a satisfying sexual life. The use of lubricants seems to be the most common but, unfortunately, advice and counselling from healthcare providers was often poor and contradictory, leaving the women confused and with little trust in the healthcare system. As sexual life can be complex a lubricant prescription is not always enough as this condition often requires sexual counselling and sometimes psychotherapy, including couples counselling. Halley et al. [22] also pointed out that healthcare providers primarily allow for physical advice but women (with BC) desired a multidimensional approach. Moreover, this study showed that the information from healthcare providers regarding pharmacological treatment for arousal dysfunction differed. To avoid misunderstandings, it is important that the professionals provide women who undergo adjuvant endocrine therapy the same and pertinent up-to-date information about pharmacological therapies and over-the-counter herbal remedies. Other strategies women use to overcome a dissatisfying sexual life were attempting to rediscover intimacy and being sexually active without penetration. However, most women noted that it was more difficult to recover psychologically than physically.
Strengths and limitations
A strength of the study is the multidisciplinary composition of the research team; which enhances the credibility of the method and analysis and created an opportunity to shed light on the research issues from a variety of perspectives. As many women were interested in participating in the study it became possible to divide the women into groups by age and whether they were offered cytostatic or not, enabling us to highlight sexual consequences and strategies from a different perspective which increases credibility.
When, as in this study, there are extensive data and data collection extends over time, there is a risk of inconsistency. New insights given from the focus groups may cause a risk that follow-up questions posed by the moderator change over time. Importance was placed on being aware of this and carefully following the interview guide. One may argue that the data are somewhat old but to our knowledge, the care of women with breast cancer therapy has not been changed. Another limitation might be the lack of partner interviews.
Conclusion
Women’s sexuality is highly affected by breast cancer and its treatment. Several symptoms and signs, in a broad sense, create problems which were experienced as being met by “silence” by the healthcare system and even lack of consensus regarding the advice given. To overcome these barriers for a sexual life without major problems they used a variety of strategies; from trying different kinds of lubricants, turning to gynaecologists, changing sexual behaviour into no- penetration sex and facing the problems as a “threshold” they have to overcome.In the future, the need for compulsory education in sexology/sexual medicine for healthcare professionals meeting women with BC seems highly significant and moreover, sex therapists need to be trained to meet women with BC.
References
- Global Burden of Disease Cancer C, Fitzmaurice C, Abate D, et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-Years for 29 Cancer Groups, 1990 to 2017: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol 2019.
- Early Breast Cancer Trialists' Collaborative G, Peto R, Davies C, et al. Comparisons between different polychemotherapy regimens for early breast cancer: meta-analyses of long-term outcome among 100,000 women in 123 randomised trials. Lancet 2012; 379: 432-444.
- Kallak TK, Baumgart J, Goransson E, Kerstin Nilsson, Inger SP, et al. Aromatase inhibitors affect vaginal proliferation and steroid hormone receptors. Menopause 2014; 21: 383-390.
- Baumgart J, Nilsson K, Evers AS, et al. Sexual dysfunction in women on adjuvant endocrine therapy after breast cancer. Menopause 2013; 20: 162-168.
- Frechette D, Paquet L, Verma S et al. The impact of endocrine therapy on sexual dysfunction in postmenopausal women with early stage breast cancer: encouraging results from a prospective study. Breast Cancer Res Treat 2013; 141: 111-117.
- Panjari M, Bell RJ, Davis SR. Sexual function after breast cancer. J Sex Med 2011; 8: 294-302.
- Cobo-Cuenca AI, Martin-Espinosa NM, Sampietro-Crespo A, et al. Sexual dysfunction in Spanish women with breast cancer. PLoS One 2018; 13: e0203151.
- Raggio GA, Butryn ML, Arigo D et al. Prevalence and correlates of sexual morbidity in long-term breast cancer survivors. Psychol Health 2014; 29: 632-650.
- Wang F, Chen F, Huo X et al. A neglected issue on sexual well-being following breast cancer diagnosis and treatment among Chinese women. PLoS One 2013; 8: e74473.
- Ussher JM, Perz J, Gilbert E. Changes to sexual well-being and intimacy after breast cancer. Cancer Nurs 2012; 35: 456-465.
- Safarinejad MR, Shafiei N, Safarinejad S. Quality of life and sexual functioning in young women with early-stage breast cancer 1 year after lumpectomy. Psychooncology 2013; 22: 1242-1248.
- Andrzejczak E, Markocka-Maczka K, Lewandowski A. Partner relationships after mastectomy in women not offered breast reconstruction. Psychooncology 2013; 22: 1653-1657.
- Barsotti Santos D, Ford NJ, Dos Santos MA, Vieira EM. Breast cancer and sexuality: the impacts of breast cancer treatment on the sex lives of women in Brazil. Cult Health Sex 2014.
- Male DA, Fergus KD, Cullen K. Sexual identity after breast cancer: sexuality, body image, and relationship repercussions. Curr Opin Support Palliat Care 2016; 10: 66-74.
- Taylor S, Harley C, Absolom K et al. Breast Cancer, Sexuality, and Intimacy: Addressing the Unmet Need. Breast J 2016; 22: 478-479.
- Bloom JR, Stewart SL, Oakley-Girvan I et al. Quality of life of younger breast cancer survivors: persistence of problems and sense of well-being. Psychooncology 2012; 21: 655-665.
- Johnsson A, von Wachenfeldt A, Fugl-Meyer K. Which Menopausal Symptoms after Adjuvant Endocrine Breast Cancer Therapy are Addressed by Health Care Providers? Medical Records Notes Versus Self-Reported Side-Effects”. EC Nursing and Healthcare 2021; 3.1: 5-1.
- Patton MQ. Qualitative research and evaluation methods. Thousand Oaks: Sage,2002.
- Krueger RA. Focus group interveiws: A practical guide for applied research. Thousand Oaks: Sage,1994.
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today 2004; 24: 105-112.
- Lundman B, Hällgren Graneheim U. Kvalitativ innehållsanalys (Qualitative Content Analysis). Lund: Studentlitteratur, 2008.
- Halley MC, May SG, Rendle KA et al. Beyond barriers: fundamental 'disconnects' underlying the treatment of breast cancer patients' sexual health. Cult Health Sex 2014; 16: 1169-1180.
- Albers LF, Van Ek GF, Krouwel EM et al. Sexual Health Needs: How Do Breast Cancer Patients and Their Partners Want Information? J Sex Marital Ther 2020; 46: 205-226.
- Fugl-Meyer K, Fugl-Meyer AR. Sexual disabilities are not singularities. Int J Impot Res 2002; 14: 487-493.
- Fugl-Meyer KS, Bohm-Starke N, Damsted Petersen C et al. Standard operating procedures for female genital sexual pain. J Sex Med 2013; 10: 83-93.
- Kraemer LM, Stanton AL, Meyerowitz BE et al. A longitudinal examination of couples' coping strategies as predictors of adjustment to breast cancer. J Fam Psychol 2011; 25: 963-972.
- Manne SL, Ostroff J, Winkel G et al. Partner unsupportive responses, avoidant coping, and distress among women with early stage breast cancer: patient and partner perspectives. Health Psychol 2005; 24: 635-641.
- Gianotten WL. Cancer and sexuality. In Kirana PS, Tripodi F, Reisman Y, Porst H (eds): The EFS and ESSM Syllabus of Clinical Sexology. Amsterdam: Medix Publ 2013; 928-947.
- ICD 11. In. 2018.
- Masjoudi M, Keshavarz Z, Akbari M et al. Barriers to Sexual Health Communication in Breast Cancer Survivors: A Qualitative Study. Journal of Clinical and Diagnostic Research 2019; 13(5): 1-4.
- Carter J, Goldfrank D, Schover LR. Simple strategies for vaginal health promotion in cancer survivors. J Sex Med 2011; 8: 549-559.
- Basson R. The female sexual response: a different model. J Sex Marital Ther 2000; 26: 51-65.
- Muise A, Impett EA, Desmarais S. Getting it on versus getting it over with: sexual motivation, desire, and satisfaction in intimate bonds. Pers Soc Psychol Bull 2013; 39: 1320-1332.
- Basson R. Using a different model for female sexual response to address women's problematic low sexual desire. J Sex Marital Ther 2001; 27: 395-403.
- Eleuteri S. Sexuality in the couple coping with breast cancer (Abstract). JSM 2019; 16, suppl 2: S78.
Editorial Manager:
Email:

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...