Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1725
Research Article(ISSN: 2641-1725) 
Topical Betamethasone Versus Clobetasol in Pediatric Patients with Phimosis: A Prospective Randomized Clinical Trial Volume 6 - Issue 5
Bruno Silva Peixoto de Carvalho1, Rômulo Augusto Lucena de Vasconcelos2* and Adriano Almeida Calado2
- 1Postgraduate Program in Health Sciences, Pernambuco State University, Recife, Pernambuco, Brazil
- 2Medical Sciences College, Pernambuco State University, Recife, Pernambuco, Brazil
Received: April 16, 2024; Published: April 25, 2024
*Corresponding author:Rômulo Augusto Lucena de Vasconcelos, Medical Sciences College, Pernambuco State University, Recife, Pernambuco, Brazil.
DOI: 10.32474/LOJMS.2024.06.000247
Abstract
Introduction: Nowadays the phimosis treatment in boys is still controversial. Recently, topical corticosteroids application has been shown to be an effective alternative to circumcision. Almost all studies used betamethasone or clobetasone condition but there are still doubts about the most effective topical treatment. A prospective study was conducted to evaluate the efficacy (response rate) of the two most utilized topical steroids (betamethasone and clobetasol) for the treatment of tight phimosis.
Methods: A randomized prospective double-blind study was performed at the Pediatric urological section. 154 boys between 3 to 10 years old were treated with bethametasone 0,05% or clobetasol 0,05%, as a cream, with two daily applications for a period of 4 to 8 weeks. After this all the boys were followed up to 12 weeks after the end of the treatment.
Results: 112(72,73%) of the treated boys had success, defined as a Kayaba class 4 or 5 glans exposition. At the 4-week followup, 57 boys (71,3%) in the group A were cured, compared to 45 (60,8%) in the group B. Fifty-two (33,7%) patients needed a second treatment cycle and at the 8-week follow-up the success rate increased to 77,5% in the betamethasone group and 67,6% in the clobetasol group There were no statistical differences between the two compared drugs. There were no side effects noted.\
Conclusion: The betamethasone and the clobetasol creams are equally efficacious and can be offered to parents requesting nonsurgical management of phimosis. Untoward effects are rare with either regimen.
Keywords: Phimosis; Treatment; Corticosteroids; Penis; Urology
Introduction
Phimosis, by far the most common medical indication for circumcision, can be defined as a narrowing of the preputial orifice, leading to an inability to retract the foreskin, or prepuce, over the glans penis [1]. The proportion of boys circumcised during childhood varies markedly by country, by religion and, to some extent, by socioeconomic group. Various Pediatric societies have developed position statements on circumcision. These statements generally conclude that there is insufficient evidence to recommend routine neonatal circumcision [2]. In the last 30 years, due to controversies regarding the medical indications for circumcision, together with the emergence of several entities opposed to circumcision, this surgery started to be questioned. This has led to widespread interest in developing an effective clinical therapy. Initial studies in Europe demonstrated good rates of success using topical steroid [3,4]. Recent reports of medical management of phimosis with topical steroids quote success rates of 67%-95% and resulting in a 75% savings compared with surgery [5-7]. This pharmacological approach is now commonly considered as an effective treatment for this condition but there are still doubts about the most effective medication. Almost all studies used betamethasone or clobetasone independently [4,5,8,9]. The aim of this study is to evaluate the efficacy (response rate) of the two most utilized topical steroids (betamethasone and clobetasol) for the treatment of tight phimosis and determine if comparable results could be achieved.
Material and Methods
154 boys (3 to 11 years, mean 6,74) were included, after parental consent, in this consecutive and prospective double-blind study. The study protocol was approved by the ethical committee of the university. All children were referred for consideration of circumcision due to of a history of phimosis and all referrals were generated from paediatricians. Study inclusion criteria, for each group were, tight phimosis never treated with topical steroids, absence of previous urinary tract infections or balanoposthitis, age >3 years and no hormone therapy administered before or during the study. Patients were randomized into the treatment groups at our outpatient’s department. The degree of preputial retractability was assessed at presentation using the classification suggested by Kayaba et al. [10]. Patients received tubes of cream (betamethasone cream 0.05% or clobetasol cream 0.05%.) at random, which were not identifiable (the tags were provided later by a member of the study who was unaware of the results); the data were kept in a sealed envelope until data collection was complete. Thus, neither the researchers nor the parents knew who were using the betamethasone or clobetasol. Topical application on the prepuce was performed twice a day for four weeks. The dose of each application was very small, just enough to make a thin film around the preputial margin. They were specifically instructed to gently retract as much as possible — not to retract forcibly, causing pain. Those cases where topical treatment failed were invited to start a new treatment cycle (more 4 weeks), carried out with the same procedure. After the end of topical treatment, stretching methods had to be carried out daily together with good personal hygiene using neutral soap. Clinical response to the treatment was defined as success if glans exposure to above corona at site of preputial adhesion (Kayaba type IV) or if easy and complete exposure of the whole glans (Kayaba type V). Failure of therapy was defined when less than half of the glans was exposed (Kayaba I, II or III). Where there had been no improvement or only minimal improvement (as assessed by both parents and clinician), patients were offered surgical intervention. Treatment outcomes (degree of preputial retractability) was evaluated at 4, 8, 12, 16 and 20 weeks of followup at the outpatient’s department. The Mann-Whitney and chisquare tests were used to compare data on the 2 groups. A p-value of <0.05 was considered statistically significant.
Results
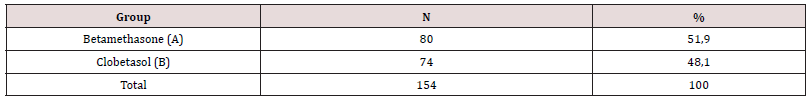
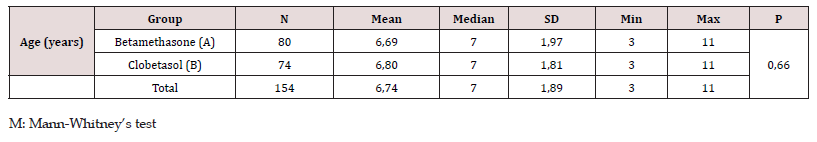
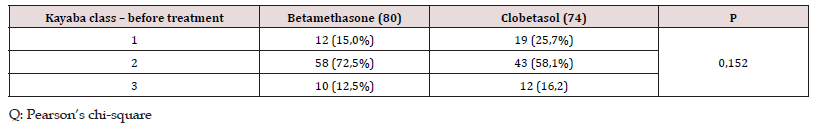
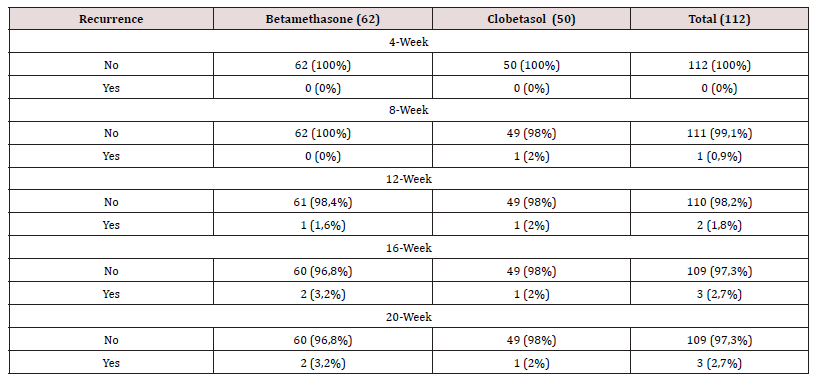
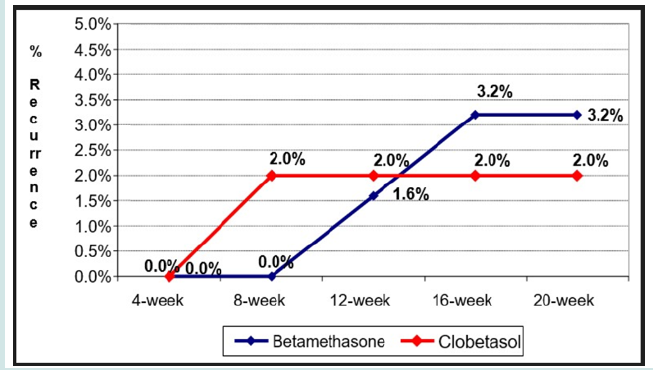
After decoding the tubes, the two groups were identified (Table 1); group A comprised 80 patients who used betamethasone cream; and group B, 74 patients who used clobetasol cream. The mean age of each study group was not significantly different between the two groups (betamethasone group 6,69 years, range 3 to 11 years, control group 6,80 years, range 3 to 11 years) (Table 2). Table 3 shows the distribution per group of degree of preputial retractability (Kayaba classification). As it is shown the two groups were homogeneous. All patients followed the treatment with a compliance of 100%. No patient from group A and B reported any side effect caused by the treatment. At the 4-week follow-up, 57 boys (71,3%) in the group A were cured, compared to 45 (60,8%) in the group B. Fifty-two (33,7%) patients needed a second treatment cycle and at the 8-week follow-up the success rate increased to 77,5% in the betamethasone group and 67,6% in the clobetasol group (Table 4, Figure 1). At the end of 20-weeks of follow up, 96,8% of the patients treated in the group A maintained total success, as compared to 98% of the group B (Table 5 – Figure 2).
Discussion
A significant number of patients seen in a typical day at a Pediatric clinic are uncircumcised boys with a nonretracting foreskin. Surgical intervention is not warranted in a large number of these patients. Many simple have adherence of the foreskin to the glans or they are infants who are best treated expectantly. Boys with persistent phimosis have the options of circumcision and now topical steroids. Circumcision, like any surgical procedure, carries a risk of complications; the reported rate varies greatly from as low as 0.06 per cent to as high as 55 per cent. This variation is largely the result of the many different criteria used to define complications [11]. On the other hand, In the mid-1990s to late 1990s, various groups began publicizing data looking at the adverse effects of genital mutilation on adult men who had undergone circumcision in childhood to stem the practice of unnecessary circumcisions. Emphasis was placed on the function and importance of the prepuce. Since then, efforts have been made to introduce conservative methods of treating phimosis. Topical application of moderate or highly potent steroids for 4-8 weeks was found to yield high success rates (67% to 95%) for prepubertal phimosis and has been advocated as a simple, safe, economical and effective primary measure in young and old boys who were referred for circumcision to the surgical departments [4-9,12]. Why topical steroids are effective for phimosis is not clear. Corticosteroids are proven to decrease arachidonic acid and hydroxy eicosatetraenoic acid in inflammatory skin diseases, to inhibit prostaglandin release and to increase the activity of superoxide dismutase, an antioxidant. Monsour et al. [5] and Orsola et al. [4] proposed that both the antiinflammatory activity and the moisturizing effect of the steroid improved the elasticity of the prepuce and allowed the prepuce to be retracted. Although steroids have many well-known side effects, including hypothalamic–pituitary–adrenal axis suppression, even highly potent steroids applied only to the foreskin (less than 0.1% of the total body surface area) are very unlikely to induce systemic side effects, even in young boys less than three years of age. Probably the efficacy of a treatment with topical steroids may depend on the efficacy of the medication on a specific patient. This would explain why some patients respond better than others to a treatment with specific topical steroids, as many surveys have shown. After treating 138 patients with betamethasone. Ku et al. [13] reported an 81,5% success rate. Lindhagen [14] and Jorgensen & Svensson [15] described success rates of 67 and 70%, respectively, using clobetasol propionate. Other studies using betamethasone or clobetasol have all been suggested that these steroids are an effective and safe treatment for phimosis with variable success rates. To avoid the expense and time required to treat phimosis with steroidal creams it would be advantageous to predict a successful outcome and if one specific topical steroid is superior to the others. Only one study compares betamethasone and clobetasol in the treatment of phimosis. In this Study the authors compared the effect of applying steroids of moderate potency with those from applying highly potent steroids, proved that their effects were similar (81.3% vs 77.4%), but contain patients under 3 years of age and may have increased possibility of physiologic phimosis which could influence the success rate [16]. For this reason, in our study we included only patients > 3 years old and exclude boys with Kayaba grade 4 and 5 (which never requires surgery as it may disappear spontaneously); second, the main aspect of our study is that we have comparatively studied two homogeneous groups of patients the first treated with betamethasone and the second with clobetasol cream. Our overall success rate seems to be lower from those in these previous reports. The reason for this low success rate may be related to the fact that our study included only boys > 3 years of age and who were referred for circumcision to surgical departments. No statistical differences were observed between the different topical steroids. In our study we proved that the duration of treatment may also influence the success rate. Moreover, none of our patients reported adverse effects related to the two medications and our results proved stable over time at a median follow-up of 20 weeks. However, in order to maintain the good results achieved, it is extremely important to stress to the parents the daily practice of genital hygiene, consisting in adequate care and cleansing of the foreskin and glans, even after withdrawal of the medication.
Conclusion
Our data are consistent with the theory that topical steroid administration is effective treatment for phimosis and before deciding to perform circumcision, topical steroid therapy should be considered, which is less invasive and more cost-effective. Betamethasone cream and clobetasol cream are effective and of comparable therapeutic efficacy in treating phimosis.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Urologia SB de [Internet]. [cited 2008 May 10].
- (1999) AA of Pediatrics Circumcision policy statement. Pediatrics.103(3): 686–693.
- ter Meulen PhH, Delaere KPJ (2001) A conservative treatment of phimosis in boys. European Urology 40(2): 196–200.
- Orsola A, Caffaratti J, Garat JM (2000) Conservative treatment of phimosis in children using a topical steroid. Urology. 56(2): 307–310.
- Monsour MA, Rabinovitch HH, Dean GE (1999) Medical Management of Phimosis in children: Our experience with topical steroids. Journal of Urology. 162(3 Part 2): 1162–1164.
- Elmore JM, Baker LA, Snodgrass WT (2002) Topical steroid therapy as an alternative to circumcision for phimosis in boys younger than 3 years. Journal of Urology. 168(4 Part 2):1746–1747.
- Berdeu D, Sauze L, Ha‐Vinh P, Blum‐Boisgard C (2001) Cost‐effectiveness analysis of treatments for phimosis: A comparison of surgical and medicinal approaches and their economic effect. BJU International. 87(3): 239–244.
- Ng W, Fan N, Wong CK, Leung SL, Yuen KS, et al. (2001) Treatment of childhood phimosis with a moderately potent topical steroid. ANZ Journal of Surgery. 71(9): 541–543.
- Klyver H, Montersen SO, Klarskov OP, Christiansen P (2001) Ugeskr Laeger 12(163): 922–924.
- Kayaba H, Tamura H, Kitajima S, Fujiwara Y, Kato T (1996) Analysis of shape and retractability of the prepuce in 603 Japanese boys. Journal of Urology. 156(5): 1813–1815.
- Niku SD, Stock JA, Kaplan GW (1995) Neonatal circumcision. Urologic Clinics of North America. 22(1): 57–65.
- Webster TM, Leonard MP (2002) Topical steroid therapy for phimosis. The Canadian Journal of Urology 1(9): 1492–1495.
- Ku W, Chiu BS, Huen K (2007) Outcome and recurrence in treatment of phimosis using topical betamethasone in children in Hong Kong. Journal of Paediatrics and Child Health. 43(1–2): 74–79.
- Lindhagen T (1996) Topical clobetasol propionate compared with placebo in the treatment of unretractable foreskin. Acta Chirurgica.;1(162):969–72.
- Jørgensen ET, Svensson A (1993) The treatment of phimosis in boys, with a potent topical steroid (clobetasol propionate 0.05%) cream. Acta Dermato-Venereologica. 73(1): 55–56.
- Yang SS, Tsai YC, Wu CC, Liu SP, Wang CC (2005) Highly potent and moderately potent topical steroids are effective in treating phimosis: A prospective randomized study. Journal of Urology. 173(4):1361-1363.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...