Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1725
Research Article(ISSN: 2641-1725) 
Severe Oligohydramnios at Term Pregnancy and Associated Factors Among Pregnant Women Admitted from June 1, 2015 to June 30, 2017 at Gondar University Specialized Hospital, Northwest Ethiopia Volume 3 - Issue 5
Tamiru Minwuye*
- Department of Obstetrics and Gynecology, Gondar University, Ethiopia
Received: October 01, 2019; Published: October 10, 2019
*Corresponding author: Tamiru Minwuye, Department of Obstetrics and Gynecology, School of Medicine, College of Medicine and Health Sciences, Gondar University, Gondar, Ethiopia
DOI: 10.32474/LOJMS.2019.03.000173
Abstract
Background: Oligohydramnios has been correlated with increased risk of fetal stillbirth, meconium aspiration syndrome, severe birth asphyxia, low Apgar score scores and congenital abnormalities. It is also associated with maternal morbidity due to increased rates of induction and instrumental or operative deliveries.
Aims & Objective: To assess maternal and perinatal outcome of sever oligohydramnios at term pregnancy and associated factors among pregnant women admitted from June 1, 2015 to June 30, 2017 at Gondar University Specialized Hospital, Northwest Ethiopia.
Methods and Materials: A descriptive cross-sectional study was conducted in Gonder University Specialized hospital from June 1, 2015 to June 30, 2017. The pregnant mothers admitted in the labor and delivery unit with a diagnosis of oligohydramnios at term singleton pregnancy with known gestation was included in the study. The data were collected using a structured and pretested questionnaire. It was entered in EPI Info7.0 and analyzed using SPSS 20.0. Logistic regression analysis was done to assess any factors associated with severe oligohydramnios.
Results: The calculated sample size was 334 and a total of 295 cases were analysed. Severe oligohydramnios was found in 93 (31.4%) of the cases. Idiopathic (unknown cause) was the most common obstetric complication of oligohydramnios identified in this study 259 (87.8%). Cesarean section was done for 237 (80.2%) of cases, the commonest indication being severe oligohydramnios(C/S can be decided for sole presence of sever oligohydramnios, for NRFHRP while on induction for oligohydramnios or for the presence of previous c/s scar or malpresentation that precludes induction of oligohydramniose cases in our set up). The likelihood of experiencing severe oligohydramnios was nearly three times higher among women with a history of hypertension (AOR= 3.22, 95% CI (1.24-8.36)) and previous history of abortion (AOR=3.42(1.26-9.23)). A unit increase in gestational age the odds of experiencing severe oligohydramnios almost doubled (AOR= 1.58, 95% CI (1.16-2.17)). Women who had ANC follow up at private clinics (AOR= 0.26, 95% CI (0.10-0.68)) were 74% lower odds of experiencing severe oligohydramnios.
Conclusion: There is significantly increased maternal morbidity in the form of a cesarean section (p<0.001) in pregnant women with term oligohydramnios. History of hypertension, previous history of abortion, place of antenatal follows up and increased gestational age were associated factors for the occurrence of severe oligohydramnios.
Keywords: Oligohydramnios; Perinatal Outcome; Maternal Morbidity; Ethiopia
Background
Amniotic Fluid (AF), which is an important part of pregnancy and is found in the gestational sac, has a number of important functions including aiding the development of the lungs, gastrointestinal tract and musculoskeletal system. It also guards against umbilical cord compression, protects the fetus from trauma, regulates body temperature and has bacteriostatic properties. As a result, amniotic fluid volume evaluation is a component of every standard sonogram or obstetric scan and one component of ante partum fetal surveillance [1,2].
Oligohydramnios has been correlated with increased risk of fetal stillbirth, meconium aspiration syndrome, severe birth asphyxia, low Apgar scores and congenital abnormalities. It is also associated with maternal morbidity in the form of increased rates of induction and instrumental or operative deliveries [3]. It also found that women with oligohydramnios had a twofold increased risk of cesarean delivery for fetal distress and a fivefold risk for an Apgar score < 7 at 5 minutes compared with pregnancies with normal AF [4,5].
A Cross sectional study done in India found that the incidence of oligohydramnios was more in primigravida (52%) and the rate of cesarean section was 42%. Whereas, Intra-uterine Growth Restriction (IUGR), low Apgar score and NICU admissions were 18%, 15% and 22% respectively. 50% of cases of oligohydramnios are idiopathic and Pregnancy Induced Hypertension (PIH) was associated with 25% of cases. Induction was performed in 100 % of cases [6].
A similar prospective case control study done on perinatal outcome associated with oligohydramnios in uncomplicated term pregnancies in Monza, Italy shows that the rates of cesarean delivery for non reassuring fetal testing (8.2% vs. 3.9%, p<0.001) and of neonates with birth weight <10th percentile (13.2% vs 5.5%, p<0.001) were significantly higher in the AFI ≤ 5 cm group compared with the AFI >5 cm. No significant differences were identified between the two groups in rates of meconium-stained amniotic fluid, 5- min Apgar score <7, or umbilical artery pH <7 [4].
The most common cause of oligohydramnios at term pregnancy is idiopathic. However, some studies revealed, hypertensive disorders, IUGR, cardiac, renal and diabetic vasculopathy, abruptio placenta, medications and congenital anomalies can contribute to its occurrence [5,7].
Studies show that oligohydramnios is associated with a variety of negative pregnancy outcomes, such as fetal distress, low birth weight, perinatal morbidity and mortality and increased incidence of cesarean section. However, other studies show that oligohydramnios is a poor predictor of adverse perinatal outcome, and even the existence of an entity like isolated term oligohydramnios has been questioned by some authors [8-10].
Previously done studies found that oligohydramnios at term increases the risk of maternal morbidity, due largely to the risks associated with interventions required. However, there was an inconclusive finding in the outcome of perinatal morbidity and mortality. In Ethiopia, specifically in the study area, there were no documented data regarding the effect of oligohydramnios on maternal and perinatal outcomes.
Therefore, this study aimed to assess the maternal and perinatal morbidities and mortality due to management of oligohydramnios at term pregnancy and its associated factors at university of Gondar Hospital.
Methods
This descriptive cross-sectional study was conducted in Gondar University Specialized Hospital, Gondar town; Ethiopia. The study was conducted from June 1, 2015 to June 30, 2017. All pregnant women admitted at Gondar University Specialized Hospital with the diagnosis of term pregnancy with oligohydramnios at 37-42 weeks of gestation period and singleton pregnancy were included in the study.
Operational definitions
Oligohydramnios: is extremes Amniotic Fluid Volume (AFI),
AFI ≤ 5 cm or a single deepest pocket of amniotic fluid ≤ 2 cm (2).
Maternal outcome: Caesarian Section (C/S), Post-Partum
Hemorrhage (PPH), induction
Perinatal outcome: Apgar score, birth weight, NICU admissions
and perinatal death
Increased maternal morbidity- Caesarian Section rate greater
than 15% (24), induction rate greater than 25% (28)
Low Apgar score: Apgar score <7 at the 5th minute.
Data collection procedure
The data were collected using pre-tested and standardized questionnaire which are composed of questions on maternal and perinatal outcomes of women with oligohydramnios at term. The instrument also includes socio-demographic characteristics, medical condition during pregnancy, obstetric risk factors, Oligohydramnios status, and maternal and perinatal outcomes. The instrument was developed in English. The questionnaire was pre-tested before the actual data collection to ensure its clarity and consistency. Two days intensive training was given to data collectors and supervisors on data collection tools and procedures by the principal investigator. Five trained data collectors were involved in the data collection process. The completed questionnaires were checked and corrected on a daily basis among data collectors and supervisors. Questionnaires with missing more than 15% of the data required were discarded.
Data processing and analysis
After the data were cleaned and checked for completeness it was entered into Epi-info version 7 and exported to Statistical Package for Social Science (SPSS) version 20 Windows for analysis. Frequency tables, graphs and cross tabulations were used for data presentation. Chi-square test of association was done to find out the association between perinatal outcome and severity of oligohydramnios as well as induction of labor at term oligohydramnios and perinatal outcome.
Logistic regression analysis was carried out to identify the independent factors associated with severity of oligohydramnios. Model fitness was checked by using the Hosmer Lemshow test at a P value > 0.05. Odds ratios (OR) with 95% confidence intervals was calculated. Statistical significance is accepted at the 5% level (p<0.05).
Results
From a total of 334 sampled women, 39 of cases are excluded as 14 of them have either unknown or unreliable gestational age and in 25 of them the information was not obtained or incomplete). The prevalence of oligohydramnios in the 3rd trimester of pregnancy is 2.36% in this particular study (as the total number of deliveries in the study period were-14,381). Most of the study participants 133 (45.1%) were in the age group 25-29 years old with minimum and maximum age of the study participants being 18 and 40 years. With regard to the residence of the study participants, most 226 (76.6%) were from Gondar town.
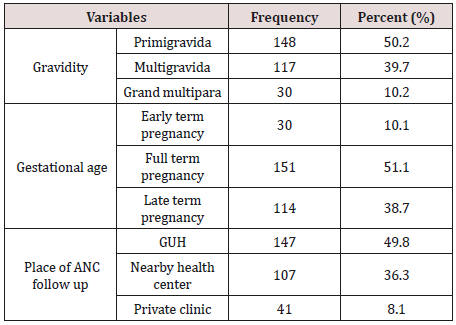
Among pregnant women with oligohydramnios at term pregnancy, the majority 148 (50.2%) were primigravida and 151 (51.1%) of them were full term pregnancy by gestational age. With regard to ANC follow up, 147 (49.8%) of them were seen at Gondar university specialized hospital. Of all the study subjects, only 21 (7.1%) of them had decreased fetal movement as a presenting compliant /symptom of diagnosis of oligohydramnios.
Medical and obstetrical problems
Concerning the presence of medical and obstetrical problems in term oligohydramnios among the study participants, the majority 259 (87.79%) of them had no known cause i.e. idiopathic. Among the known cause’s hypertensive disorders of pregnancy is the most commonly identified cause in 24 (8.14%) of the study participants (66.67% of known cases) followed by IUGR which is found in 10 (3.39%) of study participants (27.78% of known causes) (Table 1).
Table 1: Obstetric history of pregnant women with oligohydramnios at term pregnancy in Gondar University Specialized Hospital, North-West Ethiopia, from June 1, 2015 to June 30, 2017.
Oligohydramnios severity
Among pregnant women with managed oligohydramnios at term pregnancy, 202 (68.5%) of the cases the AFI was between 2 and 5cm. There was no measurable pocket of amniotic fluid, anhydramnios, in 59 (20%) of all cases. There were seven cases for which Doppler ultrasound was done for possible oligohydramnios of which only three of them were abnormal-suggesting IUGR.
Maternal outcome
Of the total study participants, 237 (80.3%) of pregnant women with oligohydramnios at term pregnancy delivered by cesarean section. The majority of cesarean deliveries 153 (64.6%) were done with no labor.ie. C/S done for indication of sever oligohydramnios, oligohydramniose with an X factor like previous C/S scar, malpresentation. That defers/contradicts induction in our set up while 82 (34.6%) of the cesarean deliveries were performed at latent and active phase of labor after induction of labor with balloon catheter and/or oxytocin was started, the indication for induction being just term pregnancy with oligohydramnios. There was no C/S done at the second stage of labor. Induction of labor at term oligohydramnios in this study was done in 143 (48.5%) of the study participants of which 58 (40.6% of induction cases) and 58 (19.7%) of them delivered vaginally. Oligohydramnios is the leading indication accounting in 108 (45.57%) of the cesarean deliveries.
Perinatal outcome
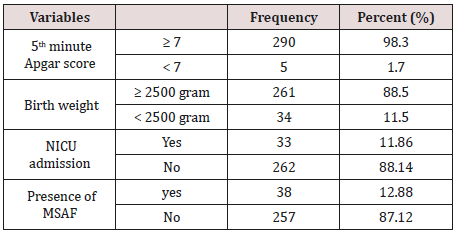
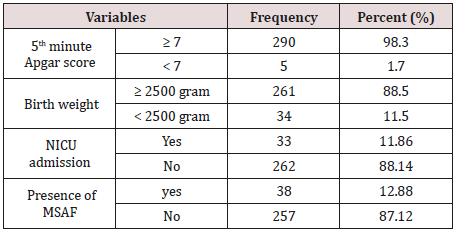
From the study participants only 5 (1.7%) women’s newborns with oligohydramnios at term pregnancy have 5th minute Apgar score < 7 and 261 (88.5%) have a birth weight ≥ 2500gm. Of the total newborns 33 (10.5%) of them were admitted to the NICU and the leading indication was being low birth weight. MSAF was present in 38 (12.9%) of cases (Table 2).
Table 2: Perinatal outcome of pregnant women with oligohydramnios at term who were managed in Gondar University Specialized Hospital, North-West Ethiopia, from June1, 2015 to June 30, 2017.
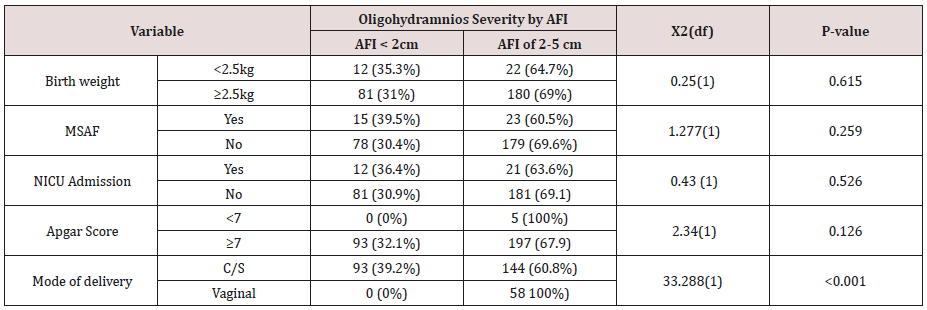
Association between oligohydramnios and perinatal & maternal outcome
Table 3: Association between severity of oligohydramnios and Perinatal & maternal outcome among pregnant women with oligohydramnios at Gondar University Specialized Hospital, North-West Ethiopia, from June 1, 2015 to June 30, 2017.
There was no significant association between severity of oligohydramnios and perinatal outcomes. Whereas, mode of delivery (cesarean C/S versus vaginal delivery) had a statistically significant association with severity of oligohydramnios (X2(df) =33.238(1), P-value<0.001). On the other hand, there was no statically significant association between perinatal outcomes of the Apgar score with induction of labor at term oligohydramnios versus immediate C/S without induction (Table 3).
Independent predictors of severe oligohydramnios
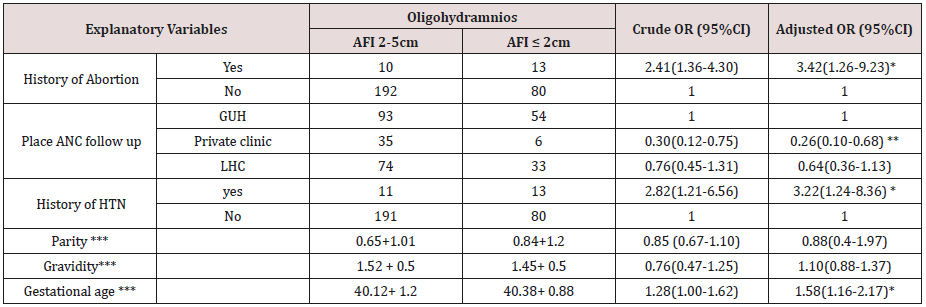
In bi-variate analysis gravidity, parity, previous history of abortion, gestational age, history of hypertension and ANC follow up place have showed significant association with severe oligohydramnios at p <0.25. The overall model to predict probability of severe oligohydramnios was statistically significant (-2Loglikelyhood=264.939, X2= 27.504, DF=6 with a p-value<0.0001).
In multivariable regression analysis gestational age, previous history of abortion, history of hypertension and place of ANC follow up were significant predictors of severe oligohydramnios. Accordingly, the likelihood of experiencing severe oligohydramnios was nearly three times higher among women with a history of hypertension (AOR= 3.22, 95% CI (1.24-8.36)) and previous history of abortion (AOR=3.42(1.26-9.23)) compared to the counterparts. Similarly, for a unit increase in gestational age the odds of experiencing severe oligohydramnios almost doubled (AOR= 1.58, 95% CI (1.16-2.17)). Women who had ANC follow up at private clinics (AOR= 0.26, 95% CI (0.10-0.68)) were 74% lower odds of severe oligohydramnios than those who have follow up at Gondar University Specialized hospital (Table 4 & Table 5).
Table 4: Multivariable analysis of factors associated with severity of oligohydramios among women with term oligohydramnios at Gondar University Specialized Hospital, North-West Ethiopia, June1, 2015 to June 30, 201.
Discussion
Oligohydramnios at term pregnancy in this study is more common in primigravida which comprises 148 (50.2%, 95% CI, (44.7%-56.3%)) of the cases. This result is nearly similar with two studies done in India [4,6]. The possible explanation for these findings is that the incidence of oligohydramnios increases as gestational age increases and in primigravida the gestational age tends to be postdate.
Concerning the possible medical and obstetric problems, among study participants with oligohydramnios at term pregnancy, the majority 259 (87.8%) of the cases had no predisposing factor i.e. idiopathic. This finding is higher than another study done in India in the 3rd trimester pregnancy, which described that 52% of cases of oligohydramnios were idiopathic [11].
Among the predisposing factors of oligohydramnios at term pregnancy, hypertensive disorders of pregnancy, IUGR, placental abruption and drug intake occurred in 24 (8.14%), 10 (3.39%), 1 (0.34%) and 1 (0.34%) of cases respectively. The results of this study are lower than the study in Israel which showed that hypertension (22.1%), premature placental separation (4.2%), IUGR (24.5%) and rate of fetal malformations (11%) are the causes identified [12]. The disparity in the aforementioned results of studies is due to different gestational age limit used in the studies.
Regarding the degree of oligohydramnios by AFI, severe oligohydramnios was found in 31.5% (95% CI 26.1-36.9) of cases of which 10% of them were anhydramnios and non-severe oligohydramnios was found in 68.5% (95% CI 63.1-73.9) of the cases. This result may show that severe oligohydramnios is less common compared a to study done in India that shows severe oligohydramnios (AFI ≤ 2cm) was found in 44% of case of which 10% are anydramnios and non-severe oligohydramnios (AFI between 2cm & 5cm) occurred in 56% of the cases [6].
This study shows that the rate of C/S is 80.3% (95% CI 75.6- 84.7) which is higher than other three studies done in India and in Iran with similar topic of this study showed that the rate of C/S were 64%, 68%, 66% and 20.2% respectively. Among the indications for C/S in this study, severe oligohydramnios is the most common 45.57% of the cases followed by non-reassuring fetal heart rate pattern (NRFHRP) , oligohydramnios with X -factor, failed induction and others occurring in 25.74%, 18.56%, 7.10% and 3.04% of the study participants respectively which is different from study done in India on pregnancy outcomes after diagnosis of oligohydramnios at term revealed that feta distress (50%), IUGR with Doppler changes (26.4%), CPD (8.8%), and failed induction (4.7%) were the indications for the C/S. Induction of labor in this study was done in 48.5% of cases which is lower than studies done in India [6,13]. The possible justification could be due to the different setting and different protocols of the studies in which in our setting more cesarean deliveries were done for severe oligohydramnios. This can be reduced by employing induction and using continuous monitoring in such cases.
According to this study, perinatal morbidities occurred among study participants were 12.88% (95% CI 9.2-16.9) for MSAF, 1.7% (95% CI 0.3-3.4) for 5th minute Apgar score <7, 11.5% (95% CI 8.1- 14.9) for LBW and 10.5% (95% CI 7.5-14.2) for a NICU admission rate. Generally, perinatal morbidities are much lower than studies done in India and Iran. There was also no significant association between severity of oligohydramnios and perinatal outcomes as well as between induction of labor for term oligohydramnios and perinatal outcome. This may be explained by the high prevalence of idiopathic oligohydramnios in this particular study which is consistent with the finding described by other studies on isolated oligohydramnios [4,13].
In this study gestational age, previous history of abortion, history of hypertension and place of ANC follow up significantly associated with severe oligohydramnios. However, due to absence of literature, we could not able to compare this evidence with previous studies.
Conclusion
There is significantly increased maternal morbidity in the form of cesarean section in pregnant women with term oligohydramnios. However, there was no significant association between perinatal outcomes and severity of oligohydramnios at term pregnancy. Induction of labor at term oligohydramnios doesn’t affect the Apgar score rate significantly. Therefore, the decision between vaginal delivery (Induction) and caesarean section should be balanced in the decision-making process. History of hypertension, previous history of abortion, private clinic ANC follows up and increased gestational age are associated factors for the occurrence of severe oligohydramnios.
List of Abbreviations:
AFI: Amniotic Fluid Index; ACEI: Angiotensive Converting Enzyme Inhibitors; ARB: Angiotensive Receptor Blockers; ANC: Antenatal Care; BP: Blood Pressure; C/S: Cesarean Section; CPD: Cephalopelvic Disproportion; EFW: Estimated Fetal Weight; GYN/OBS: Gynecology and Obstetrics; HTN: Hypertension; IUGR: Intrauterine Growth Restriction; LBW: Low Birth Weight; MSAF: Meconium Stained Amniotic Fluid; MAS: Meconium Aspiration Syndrome; NICU: Neonatal Intensive Care Unit; NSAID: Non- Steroidal Anti-Inflammatory Drugs; PIH: Pregnancy Induced Hypertension; PPH: Post-Partum Hemorrhage; RBS: Random Blood Sugar; U/S: Ultrasound
Declarations
Ethics approval and consent to participate.
Ethical clearance was obtained from ethical review committee
of the University of Gondar, collage of medicine and health sciences,
and school of medicine. Permission letter to conduct the study
was obtained from Gondar University Specialized hospital medical
director. The letter was submitted to the head of Gondar University
Specialized hospital documentation and information center for
cooperation to retrieve charts in the data collection process.
Consent for publication
Not applicable.
Availability of Data and Materials
We confirmed that all data underlying the findings would be fully available without restriction if the manuscript is published.
Competing Interests
The authors declare that they have no conflict of interest.
Funding
The authors received no specific funding for this work.
Authors Contribution
Conceived and designed the study: TM ZM SH. Performed the study: TM ZM SH. Analyzed the data: TM SH. Contributed reagents/ materials/analysis tools: TM ZM SH. Wrote the Manuscript: SH TM ZM. All authors read and approved the final manuscript.
Acknowledgements
We would like to thank Gondar University Specialized Hospital documentation and information center staffs their cooperation in the chart retrieval process. Our gratitude also goes to the data collectors and supervisors.
References
- Sultana S, Khan AM, Akhtar KA, Aslam M (2008) Low amniotic fluid index in high-risk pregnancy and poor apgar score at birth. J Coll Physicians Surg Pak 18(10): 630-634.
- Patel PK, Pitre DS, Gupta H (2015) Pregnancy outcome in isolated oligohydramnios at term. Ntl J of Community Med 6(2): 84-88.
- Locatelli A, Vergani P, Toso L, Verderio M, Pezzullo JC, et al. (2004) Perinatal outcome associated with oligohydramnios in uncomplicated term pregnancies. Archives of gynecology and obstetrics 269(2): 130- 133.
- Bangal VB, Giri PA, Sali BM (2011) Incidence of oligohydramnios during pregnancy and its effects on maternal and perinatal outcome. Journal of Pharmaceutical and Biomedical Sciences 12(5): 1-4.
- Gary Cunningham KJ, Leveno SL, Bloom CY, Spong Jodi SD, Barbara LH, et al. (2011) Oligohydramnios and its management. 24: 236-238.
- Jagatia K, Singh N, Patel S (2013) Maternal and fetal outcome in oligohydramnios-Study of 100 cases. International Journal of Medical Science and Public Health 2(3): 724-727.
- Suchithra R, Shreenivas S, Hasini C (2015) To assess the perinatal outcome in isolated oligohydramnios (AFI<5cm) between 37 to 40 weeks of gestation. International Journal of Research in Health Sciences 3(2): 355-360
- Chauhan SP, Sanderson M, Hendrix NW, Magann EF, Devoe LD (1999) Perinatal outcome and amniotic fluid index in the antepartum and intrapartum periods: a meta-analysis. American Journal of Obstetrics & Gynecology 181(6): 1473-1478.
- Sangeetha K, Rao J, Ashwini AP, Kumar A (2015) Pregnancy Outcome in amniotic fluid index less than 5 in term low risk pregnancy. Int J Sci Stud 3(3): 69-73.
- Manzanares S, Carrillo MP, González-Perán E, Puertas A, Montoya F (2007) Isolated oligohydramnios in term pregnancy as an indication for induction of labor. The Journal of Maternal-Fetal & Neonatal Medicine 20(3): 221-224.
- Conway DL, Adkins WB, Schroeder B, Langer O (1998) Isolated oligohydramnios in the term pregnancy: is it a clinical entity? Journal of Maternal-Fetal Medicine 7(4): 197-200.
- Golan A, Lin G, Evron S, Arieli S, Niv D, et al. (1994) Oligohydramnios: maternal complications and fetal outcome in 145 cases. Gynecologic and obstetric investigation 37(2): 91-95.
- Sowmya K, Betty V, Umashankar BY (2014) Effect of isolated oligohydramnios in otherwise normal term pregnancy, International Journal of Biomedical Research 5(2).

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...