Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1725
Research Article(ISSN: 2641-1725) 
“Lean Management” a Method of Improving Change Management in Healthcare Organizations Volume 4 - Issue 3
Joanna Jasińska1* and Hab2
- 1University of Social, Computer & Medicine Science, Poland
- 2University of Social Sciences Computer Science and Medicine, Vice-Rector for Education and Development, Poland
Received: January 06, 2020; Published: January 13, 2020
*Corresponding author: Joanna Jasińska, University of Social, Computer & Medicine Science, Poland
DOI: 10.32474/LOJMS.2020.04.000186
Abstract
The aim of this article is to present selected ways of developing the management in medical institutions in Poland with the help of Lean Management. The author concentrates on processes of changes in clinical hospitals which include dealing with special tasks in healthcare system, diversity of tasks, medical technology, diversity of relationships with the surrounding, financing from few different sources, limits of resources (especially public ones). The article leads to a conclusion that Lean Management should be a way of thinking.
Keywords: Lean; Management; Health services; Health care units restructuring
Admission
The production management system developed and
implemented at the Toyota concern in the period after World War
II was recognized as a kind of miracle in the area of management
systems, enabling the improvement of productivity, quality and
efficiency of enterprises. For years, it was introduced to production
systems, as well as in health care and many entities operating in
various sectors of the economy under the name Lean Management,
Lean Production or simply Lean. Lean in management means
eliminating losses and any factors not adding value to a product
or service. The key ingredient of Lean is continuous improvement
[1]. According to Graban, Lean is a set of tools, management
system and philosophy, whose introduction can change the way
of organization and management of medicinal entities. “A lean
system is a method that allows hospitals to improve the quality of
patient care by reducing the number of errors and reducing waiting
times” [2]. Permanent pursuit of perfection in the management
of manufacturing processes is not without a negative impact
on the satisfaction of healthcare system employees. It is often
not connected with raising salaries, improving work safety or
improving working conditions.
The purpose of this article is to indicate selected directions for
improving change management in healthcare entities in Poland
using the Lean Management concept. Changes in management were
presented in the aspect of restructuring activities undertaken in
healthcare entities. Particular attention will be focused on change
processes in multi-specialized hospitals, which have the following
features:
a) Performing specialized tasks in the field of health protection,
b) Multi-tasking,
c) Using highly advanced medical technologies,
d) The multiplicity and diversity of relationships with the
environment,
e) Financing from several sources.
Specialist hospitals, due to their organizational complexity, are
subject to change processes, which results not only from legally
imposed obligations [Act of 15 April 2011 on medical activities: Dz. Of Laws 2011 No. 112, item 654], but also from the decisions of
managers managing entities. These institutions are implementing
changes in the financial and organizational area. The effectiveness
of actions resulting from centrally made systemic decisions aimed
at restoring the financial balance of public health care facilities
in Poland has been undertaken since the 1990s and is now being
continued. As part of the so-called Plan B in the years 2009–2016
[Resolution No. 58/2009 of the Council of Ministers of 27 April
2009 on establishing a multiannual program called ‘Support
for local government units in actions stabilizing the health care
system’]. The restructuring changes program at that time covered
80 independent public health care facilities [Rydzewska 2017, p.
179-187].
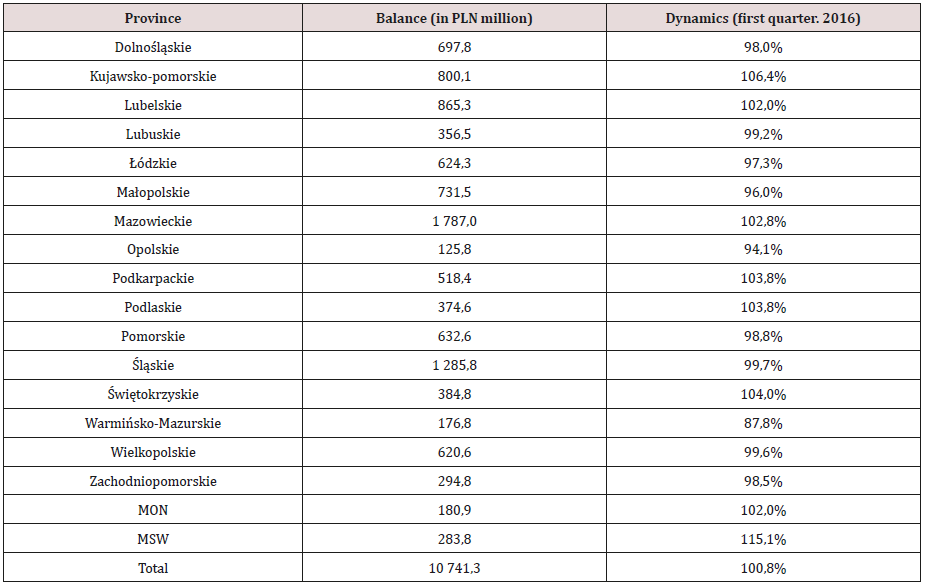
Source: Dynamics of total SPZOZ liabilities, broken down by
voivodships. MZ information based on survey data obtained from
voivodship offices, the Ministry of the Interior, the Ministry of
National Defense, medical universities and SPZOZ supervised by
the Ministry of Health, http://www.mz.gov.pl/
Despite a number of initiatives at the level of the Ministry of
Health and at the level of management by public local governments
of public health care facilities, their debt not only has not stabilized,
but - as the latest data shows - it increases in the scale of the health
system Table 1. In view of such facts, it is justified to seek and
implement solutions that are good practices enabling rational and
effective / lean resources of medical organizations while reconciling
the interests of recipients of medical services.
Lean Management Concept Main Assumptions
A number of Lean Management terms have been presented in
the literature. This concept is presented as business management,
which assumes adapting it to market management conditions
based on continuous organization rationalization processes
and its relations with the environment. These processes should
concern the introduction of changes in the organization in terms of
operations, property structure, management, shaping the attitudes
of employees focused on “slimming” the organization [3]. In another
term, the emphasis is on ways of reducing the cost of generating
added value for the customer by rationalizing employment,
infrastructure, expenditure on current and investment activities,
and working time [4]. The main principle of Lean Management
is primarily the elimination of waste to reduce the costs of the
entity’s operations while ensuring adequate added value for the
client [5]. In a different approach, Lean Management is combined
with the organization management method, especially in the
process of implemented changes [6]. It emphasizes rationalization
by restructuring the organization’s resources and the way they
are used, taking into account the conditions arising from its
environment. In the term Lean Management, the role of “slimming” the organization in order to improve the productivity and quality
of products is emphasized [6]. As it results from the quoted terms,
the Lean concept refers to both the internal elements of the subject
and his relationship with the environment in which he operates.
It covers activities improving the quality of products, restructuring
the scope of manufactured products, related to the flattening
of organizational structures, with changes in human resource
management and ensuring the competitiveness of manufactured
products. The key concept of Lean Management is the added
value of the product or service for the recipient, while generating
profit for their producer. Obtaining it requires meeting at least the
following conditions:
a) The customer (in the case of health protection, individual
patient or institutional payer - public or private) is willing to
pay for the product,
b) The product (health service) has the value desired by the
customer (it is not defective, has utility value, corresponds to
the health need),
c) The manufacturer (medical entity) rationalizes the use of
production factors (labor input, expenditure on manufacturing
instrumentation, expenditure on infrastructure, proper
inventory rotation).
Understanding the Lean Management principle is a condition
to avoid misunderstanding its essence. Correct interpretation is
associated with its identification with activities aimed at eliminating
waste (from Japanese Muda), and not with austerity measures
consisting in limiting expenditures while providing value not fully
desired for the patient (e.g. limiting the employment of persons in
the positions of medical secretaries assisting the work of doctors
or people working in the registration of medical entities, resulting
in longer queues and patient waiting times, as well as employee
dissatisfaction due to excessive workload). [7]. The term Muda is
combined, among others with: production of defective products,
production of products with low utility and low efficiency for the
recipient, production of often unnecessary products, inefficient
organization of employees’ work resulting in so-called apparent
actions (not having a real purpose), lack of synchronization in
time and space of activities of individual employees or groups
of employees (downtime related to time not worked effectively,
resulting from non-delivery of products by the previous product
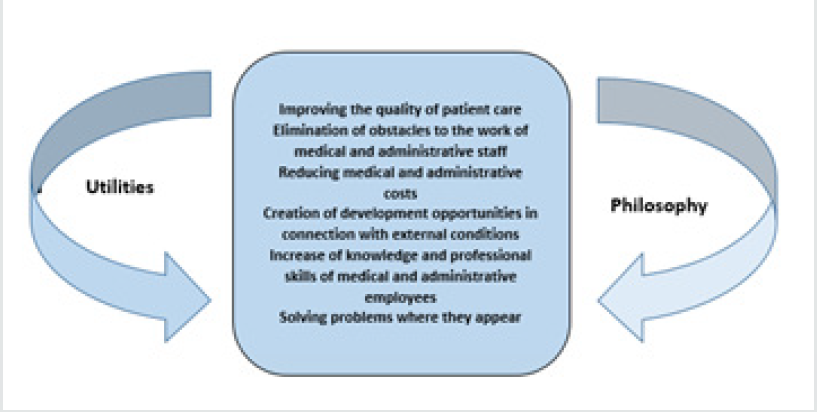
manufacturing links) Figure-1.
Source: Own study based on [2].
To sum up, it should be emphasized that the concept of
lean management, especially in the management of healthcare
organizations, should be clearly understood. Elimination of waste
(time, equipment and apparatus, money) should be distinguished
from economical and limiting resources of medical organizations
that cause disruptions in the course of medical processes, extending
patient waiting time, offering defective health services and
dissatisfaction of employees with work overload. Lean Management
as a concept supporting the implementation of changes is not a way
to generate profit at all costs, but is a way to reconcile the demand
side with the supply side through the transformation of assets, the
way of management, organization, relations with the environment
understood not only as a market of health services, but much more
widely (legislation, competition, outsourcing, general economic
factors).
Principles and Tools of Lean Management in the Aspect of Application in Healthcare Organizations
Creating patient value should be based on several principles of
Lean Management. The rules are as follows:
a) The products are free of defects (benefits having value
for the recipient; benefits not disputed by payers - in accordance
with technological standards, requirements set by payers as to the qualifications of personnel, medical equipment and apparatus,
infrastructure conditions; benefits corresponding to satisfying a
given health need; no loss of time and material; safe in terms of
health, technology and hygiene for all stakeholders),
b) Solving problems at the place of origin (employees’
readiness to redefine activities and redesign work),
c) Compliance of the performed health service with the
standard way of its performance (if it was developed), objectives,
conditions of implementation,
d) Transparency of relations between producers and
recipients of health services thanks to a properly designed and
constantly improved process of manufacturing and supplying
products; designing roles enabling the production of services
without defects [8].
e) Techniques leading to the elimination of losses and
adapting business results to external expectations should also
be adapted to the specifics of healthcare organization entities.
Selected techniques include, but are not limited to, techniques
that may prove particularly valuable from the perspective of the
effectiveness of implementing changes in healthcare organizations.
These are among others:
f) Just in Time or production on time - the use of this tool
allows you to eliminate the unjustified expectations of patients,
employees from the same or another organizational unit, recipients,
suppliers, and as a consequence prevents the loss of contracts and
income.
g) Kanban - is a system of signals used in undertaking
individual actions at various stages of product creation (at what
point in time the next health service for the patient is needed,
in which organizational part of the entity, which personal and
material resources are to be used). The condition of introducing
the signal system is to create an undisturbed system of relations
between individual groups of employees or organizational units
of the therapeutic entity leading to the development of principles
of close cooperation and a system of communication between
them. A particularly desirable approach to patient management is
treating the patient care path as an inseparable whole (successive
phases of value creation), which is a condition for determining
the cumulative value (final health effect) of individual services
(medical procedures) performed for the patient. The condition is
cooperation between individual organizational parts of the entity
and a departure from treating services performed by individual
organizational units as final or detached from the final effect for
the patient.
h) Elimination of waste - areas of waste can be: production
of health services that do not correspond to the reported demand,
breaks / downtime between the individual stages of the process of
creating value (the final health effect) for the recipient, unjustified
movement between the stages of creating value (transport of the
patient between parts of the hospital or between hospitals), the
appearance of defects in the manufacturing process or product
(making an incorrect diagnosis based on a faulty performance of
a diagnostic test), unjustified generation of inventory, unnecessary
movement of employees, equipment and apparatus, documentation
and an unfriendly way of delivering products to recipients (failure
to comply with the dates and hours of health service). For example
- obtaining incorrect results of a patient’s diagnostic examination
requires correction or repetition, i.e. the consumption of additional
material resources and workload, as well as additional control.
This, in turn, can cause “downtime” in other parts of the medical
organization.
i) 5 S (selection, systematics, cleaning, standardization,
self-discipline) - the use of this tool becomes possible to reduce
in-hospital infections, which may also result from irregularities
in waste storage, non-compliance with occupational hygiene,
movement between hospital departments without adequate
protection against exposure to infection biological agents.
j) Creating a value stream map (VSM) - the essence of VSM is
to analyze how to produce and deliver the product to the customer
and identify those activities that add value. The activity that creates
the value of a patient’s medical service is to conduct an interview
with the patient by a nurse, as opposed to providing no interview
with a patient waiting for direct contact with a doctor who only
after entering the office orders or conducts the interview himself.
k) Jidoka - is a way for employees to respond in the event
of problems during the product manufacturing process. Prevents
the penetration of the defective product or its parts into the
next stages of manufacture and subsequent positions, e.g. in the
event of incorrect preparation of the patient for a diagnostic test
or surgery, the employee should break the chain of subsequent
medical activities that may have a defective “effect” of the medical
procedure.
l) To sum up, it should be emphasized that the selection of
tools under the Lean Management concept and the way they are
used must take into account the specifics of a given activity, as well
as adapting them to a given type of therapeutic entity [9].
Using the principles of “lean” management in restructured healthcare organizations - Lean Healthcare
The principles of Lean management in health care were adopted
to be called Lean Healthcare. They have been introduced in many
healthcare organizations in numerous countries [10]. However,
experience shows that only part of the Lean Management tools
and methods have been used to improve selected areas of activity
of health care entities, especially hospitals. Given the specifics of
the healthcare sector and operations, Lean Healthcare has a specific
interpretation: a medical entity is an entity that produces specific
products - most often they are health services; health service is a
manufacturing process; the patient, together with the services
provided to him which bring specific health effects, is a product. The applications of Lean Healthcare in healthcare organizations
presented in the literature show that it is most often focused on
improving the quality of health care (increasing the value of the
product for the patient), improving access to health services,
improving organizational processes and rationalizing costs.
Improving access to healthcare understood as shortening the
waiting time for health services, streamlining internal processes
related to providing patients with services are the factors that allow
rationalization of the costs of medical procedures. By increasing
work efficiency, both in terms of health services and support
activities (patient registration, referring patients to appropriate
organizational units in the hospital) - there is the possibility of
shortening expectations for services and improving the economic
efficiency of entities. With the high effectiveness of implementing
changes, patient waiting times can be reduced by up to 42% [11].
Reducing patients’ waiting time for medical procedures is not the
only attribute of high-quality healthcare. It also depends on the
method of providing health services, especially in those entities
(mainly hospitals) that provide comprehensive care for a package
of medical services. Often, due to the nature of the disease, the
group of patients requires various activities not only within one
ward / hospital department. An example would be elderly patients
with chronic diseases. The experience of hospitals indicates that
ensuring higher quality of care may depend on the implementation
of so-called complex co-managed care depending on the patient’s
condition and medical procedures that he needs. This creates a
situation in which patients are not exposed to frequent movement
between different parts of the hospital (avoiding unnecessary
transport) and frequent changes of the staff who care for them. This
undoubtedly increases the sense of patient safety [12]. The problem
of many healthcare organizations in most health systems is the
strong bureaucracy of organizational structures. This is associated
with the loss of working time of medical workers, and from the point
of view of patients with prolonged paths and time from the moment
of issuing the diagnostic test order to its execution and obtaining
the test result. Often, the extension of the “path” is associated
either with errors in completing order cards or with errors in the
performance of the study itself. According to Canadian experience,
by optimizing the time spent on organizational processes or
activities related to medical diagnostics, hospitals can intensify
both human and apparatus work, and thus at the same time
provide more health services, which can translate into increased
accessibility them. An additional advantage is the implementation
of the same activity with the same measures [13]. The changes
inspired by the Lean Healthcare concept, which resulted in a
reduction of patients’ waiting time by 19-24%, were associated with
the creation of clear, understandable mechanisms of cooperation
between individual employees by defining their roles in the chain of
creating value for the patient, creating new principles of employee
communication, defining patterns procedures and work schedules,
scope of duties and ways of solving current problems. Adaptation
of Lean Healthcare in Swedish hospitals has resulted in improved
management due to the introduction of work standardization,
organizational connections of positions / people working in mutual
logical relationships, elimination of unnecessary and disruptive
medical procedures, introduction of employee motivation to
independently identify problems and overcome them [14].
The effectiveness of Lean Healthcare adaptation in strengthening
employee roles in the value creation chain may be conditioned
by transferring greater responsibility for the way the work is
performed and its effects to individual employees who perceive
it as an increased motivation to work [15]. Given the specifics of
the tasks performed, the manner of management in healthcare
organizations, and strong restrictions on their functioning, caused
by limited access to public funds, an approach that can bring
good results from the implementation of Lean principles is the
evolutionary approach [Nielsen, Improving Healthcare through
Lean Management: Experiences from the Danish healthcare
system].
In view of the international experience and conclusions
resulting from the implementation of Lean Healthcare in healthcare
entities and the conditions for the functioning of healthcare
organizations in Poland, an attempt can be made to indicate
directions for improving management in healthcare entities.
Particular attention will be focused on specialist hospitals. The
starting point for determining the areas of the entity’s operations
that should become subject to improvement / restructuring is the
diagnosis of the entity’s activities, including:
a) Analysis of the economic situation (basic economic values and
indicators as well as financial statements); in the conditions
of growing financial debt of hospitals in Poland, the scope of
analysis should include: financial efficiency ratios - receivables
turnover, liabilities turnover, inventory turnover; debt ratios
- total debt ratio, equity to liabilities ratio; productivity
indicators),
b) Analysis of the causes of the entity’s existing financial situation
(impact of system changes on the entity’s position),
c) Analysis of internal causes of organization and management
irregularities (scope and structure of resources, degree of
their adaptation to conducted activity, allocation of resources
in the entity, organization of work processes, mutual relations
between medical activities).
The conclusions made as a result of the diagnosis should
become the starting point for indicating the directions of improving
the management of the entity. However, creating a uniform list
of directions, or “path of change” for all hospitals is not justified
because existing profile, technological, organizational and financial
differences that generate other problems. Potentially they may
include:
a) Setting priority and other tasks in individual areas of
conducted activity (medical, scientific, didactic) and medical
specialties as well as individual activities constituting their
implementation;
b) Organizational changes, e.g. laboratory diagnostics
combined with a change in the location of diagnostic cells to
reduce costs; allocation of archived documents in one “place” in the
hospital building, which will allow faster access to information and
adaptation of vacant rooms for other purposes;
c) Functional changes - restructuring of hospital beds in
order to adjust the financing bed base (monitoring indicators of
average period of stay of patients, waiting time for admission to a
ward or clinic, the degree of bed use);
d) Resource changes: a combination of clinical units enabling
consistent policy to intensify the use of medical equipment and
apparatus; providing access to the departments’ facilities providing
health services as part of caring for the local population (eliminating
duplication of purchases of the same equipment and apparatus
as well as dispersion of equipment increasing operating costs);
centralization of the distribution of diagnostic base elements;
e) Changes in personal resources in the aspect of assigning
employees to diagnostic, hospitalization and outpatient tasks;
formal assignment of employees to consulting tasks not only within
one branch, but also for other organizational units;
f) Eliminating (by pooling) duplication of the same medical
procedures by several hospital organizational units to improve
resource management and eliminate unnecessary manufacturing
factors;
g) Determining the centers of responsibility for the
management of medical equipment and apparatus (taking over
supervision over the management of diagnostic equipment by a
separate department, plant, clinic or clinic);
h) Implementation of new medical technologies enabling
more efficient diagnosis of disease entities, which is associated with
shortening the waiting time for results and the time from diagnosis
to intervention;
i) Implementation of an integrated IT system facilitating
and accelerating the flow of information in the hospital (integrated
management of drugs, medical equipment, centralization of
material management),
j) Implementation of integrated management of medical
materials, medical consumables and medicines;
k) Establishment of cost responsibility centers to strengthen
supervision and eliminate waste;
l) Developing the principles of communication between
the management and employees in order to explain and motivate,
which allows reducing stress and social unrest associated with the
economic uncertainty of the entity;
m) Compliance with the precise implementation of contracts
with payers in order to eliminate any financial sanctions, including
the termination of contracts; particular attention should be focused
on the so-called over-limit benefits;
n) Property restructuring (e.g. when the hospital operates
in several different buildings / rooms distant from each other or
the infrastructure is not used due to poor technical condition) to
eliminate unnecessary usable space and unnecessary transport, to
rationalize maintenance costs and depreciation costs;
o) Outsourcing of non-medical services.
Summary
The effective functioning of medical entities depends not only
on the course of internal management processes, but also on the
flexible adjustment of their activities to the changing environment.
The emergence of new health technologies, changing health
exposures not yet occurring or occurring to a limited extent,
demographic and epidemiological changes in combination with
systemic factors force changes in which the use of “lean management”
may be particularly useful. The main directions of improving the
functioning of healthcare organizations should be: reducing the
time of access to health services by designing an efficient from the
point of view of direct recipients of the implementation of activities
preceding the performance of health services; this is associated
with a smooth transfer of information, e.g. about available places
in hospital wards; maximum focus on patients’ expectations,
while in the case of financing services from public funds - focus
on the implementation of obligations towards public payers
(National Health Fund, ministries, local governments), which
are related to the implementation of the principles of contracts
concluded (comprehensiveness and continuity of care, accuracy
of diagnoses , reliability of the use of diagnostic, therapeutic and
prophylactic methods, ensuring declared personnel, equipment
and infrastructure conditions, maintaining the assumed level
of costs and financial result). Ensuring good communication
between patients and the medical entity in the scope of providing
information at every stage of medical treatment with the patient.
Conducting constant analysis of work positions, activities of
individual organizational parts of the medical entity in order to
formulate current recommendations for employees assuming equal
treatment of medical employees and those indirectly involved in
the provision of medical services.
In addition, care for proper technological preparation, which
allows to avoid discouragement of employees and patients
as well as the increase of costs and losses, which result, e.g.
from poor-quality diagnostic tests results requiring repetition,
downtime, cancellations of medical services. It is also important
to increase the quality of tasks implemented, which contributes to
strengthening the relationship between hospitals and recipients
of their products (patients, payers, other medical entities) [16].
Even precise determination of directions of changes in health
care organizations may not prevent management staff from
implementing them incorrectly. The main risks associated with
the distortion of the Lean being are most often: identifying the
Lean concept with the economic or financial rationalization of the
medical entity’s economy, reducing financial liquidity, reducing the quality of services and bypassing legal provisions imposing specific
obligations on entities contracting benefits with payers, increasing
the level of employee stress and decrease in motivation to work,
rationalizing employment by simply limiting it, neglecting the
problems of employees with lower qualifications [17]. According
to prof. Zimniewicza [18], the need arises to consolidate the Lean
concept as a way of thinking.
References
- Niedziółka M, Piasek A (2014) Kaizen Costing by a modern method of cost management, Scientific Notebooks of the Podlasie University in Siedlce, Series: Administration and Management 81: 79-87.
- Graban M (2014) Lean hospitals - improving hospitals. Quality improvement, patient safety and staff satisfaction, ProdPublishing, Wrocław, Poland, p. 2.
- Lichtarski J (1997) Fundamentals of enterprise science, WAE, Wrocław, Poland, pp 224.
- Jones DT, Womack JP (2014) Slimming companies, CIM, Warsaw, Poland.
- Czerska J (2016) More than slimming, i.e. the essence of the concept of Lean management, Staff.
- Pedro José Martínez-Jurado, JoséMoyano-Fuentes (2014) Lean Management, Supply Chain Management and Sustainability 85 (15): 134-150.
- Cholewicka Goździk K (2014) LEAN method - process and product improvement, Quality Problems p. 21.
- Jimmerson C Weber D Sobek DK (2014) Reducing Waste and Errors: Piloting Lean Principles at IHC, Joint Commission Journal on Quality and Safety 1-22.
- Kubis N (2015) Lean management tools, Technical and Economic issues 50(2-3): 291-303.
- De Souza LB (2015) Trends and Approaches in Lean Healthcare, Leadership in Health Services 22 (2): 121-139.
- Bernatek A (2019) A profitable investment in Lean Healthcare.
- Greco A, Cascavilla L, Paris F, Addante F, Miscio L, et al. (2015) The nephro-geriatric unit in a lean-oriented in hospital model of care. J Nephrol 25(19): 16-19.
- Villeneuve C (2014) Fujitsu’s Lean Soution Group. Lean Healthcare in Canada. Fujitsu Sci Tech 47(1): 41-48.
- Mazzocato P, Holden RJ, Brommels M, Aronsson H, Bäckman U, et al. (2016) How does lean work in emergency care? A case study of a lean-inspired intervention at the Astrid Lindgren Children’s hospital, Stockholm. Sweden BMC Health Services Research 12: 28.
- Glossmann JP, Schliebusch O, Diehl V, Walshe R (2016) Lean management in hospitals: Potentials and limitations. Med Klin Munich 95(8): 470-473.
- Sobczak A, Rydlewska Liszkowska I (2016) Management of occupational medicine entities. The concept and application of lean management, Occupational Medicine 63(5): 599-606.
- Robbins A (2016) Lean Management I outsourcing. The road to success is to take massive, determined actions, Change management. POU Newsletter.
- Zimniewicz K (1999) Contemporary management concepts and methods, Polish Economic Publishing House, Warsaw, Poland, p. 63.
- Brännmark M, Halvarsson A, Lindskog P (2019) Implementing Lean in Swedish Municipalities and Hospitals.
- Der Shin Ke Overwork (2012) Stroke and Karoshi-death from Overwork. Acta Neurol Taiwan 21(2): 54-59.
- Encyklopedia Zarządzania (2019).
- Fijałkowska B (2019)
- Efficiency and restructuring of SPZOZ (2019).
- Izabela Rydlewska-Liszkowska, Lean Management-doskonalenie zarządzania pp. 289.
- Inoue K, Matsumoto M (2014) Suicide from overwork: A spreading occupational threat. Occup Environ Med 57(4): 284-285.
- Iwasaki K, Takahashi M, Nakata A (2016) Health problems due to long working hours in Japan: Working hours, workers compensation (Karoshi) and preventive measures. Ind Health 44(4): 537-540.
- Kawanishi Y (2016) Suicide by Overwork: Why Do Japanese Workers Work Themselves to Death?. Follow International Journal of Mental Health 37(1): 61-74.
- Nogalski B, Walentynowicz P (2016) Modern management concepts in production enterprises of the Pomeranian region - an attempt to evaluate, Scientific Papers of E. Kwiatkowski University of Administration and Business in Gdynia 7: 14-32.
- Nielsen AP (2019) Improving Healthcare through Lean Management: Experiences from the Danish healthcare system.
- Uchiyama S, Kurasawa T, Sekizawa T, Nakatsuka HJ (2015) Job strain and risk of cardiovascular events in treated hypertensive Japanese workers: hypertension follow-up group study. Occup Health 47(2): 102-111.
- Act of 15 April 2011 on medical activity, Journal of Laws 2011 No. 112: 654.
- Weathers C, North S (2015) Overtime Activists Take on Corporate Titans: Toyota, McDonald’s and Japan’s Work Hour Controversy. Pacific Affairs 82(4): 615-636.
- Zimniewicz K (1999) Contemporary management concepts and methods, Polish Economic Publishing House, Warsaw, Poland, p. 63.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...