Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1725
Case Report(ISSN: 2641-1725) 
Fatal Intoxication with Metformin and Gliclazide- Case Report Volume 6 - Issue 1
Peter Jackuliak1, Magdaléna Kovářová1, Andrea Martonová2, Viera Žufková³, Andrea Gažová4*, Ján Kyselovič1 and Juraj Payer1
- 1Department of Internal Medicine, Comenius University Faculty of Medicine, Slovakia
- 2Department of Anaesthesiology and Intensive Medicine, Comenius University Faculty of Medicine, Slovakia
- 3Department of Languages, Comenius University Faculty of Pharmacy, Bratislava, Slovakia
- 4Institute of Pharmacology and Clinical Pharmacology, Faculty of Medicine, Comenius University, Slovakia
Received: December 01, 2021 Published: December 8, 2021
*Corresponding author: Andrea Gažová, Institute of Pharmacology and Clinical Pharmacology, Faculty of Medicine, Comenius University, Slovakia
DOI: 10.32474/LOJMS.2021.06.000229
Abstract
Introduction: Biguanides (metformin) and sulfonylurea molecule (gliclazide) are oral antihyperglycemic drugs. Metformin can
make lactate accumulation in patients with hepatic or renal failure or in patients with a suicide attempt. Gliclazide has very low
toxicity, and it can develop acute renal failure in patients with massive ingestion in a suicide attempt.
The patient’s Primary Concerns and Critical Clinical Findings: A 53-year-old patient with a personal history of type 2
diabetes mellitus was treated with metformin 1000 mg twice daily and gliclazide 60 mg twice daily. On December 26th, 2018, in the
evening hours, he consumed 90 tablets of metformin 1000 mg (total dose 90 grams) and 95 tablets of gliclazide 60 mg (total dose
5.7 grams) for suicide. According to the report, he had been sicking all night and suffered from muscle pain, diarrhoea, and vomiting.
The Primary Diagnoses, Interventions, and Outcomes: We concluded the diagnosis as a high anion gap metabolic acidosis.
As a consequence of metformin intoxication, lactate level was furthermore elevated (24 mM).
Conclusion: Metformin and gliclazide are commonly using as effective drugs in patients with type 2 diabetes mellitus. Our case
report described fatal intoxication with metformin and gliclazide. The aim is to remember the risk of daily used antidiabetic drugsin
high doses, in combinations, they can lead to pancreatitis, renal failure, or so long-known lactic acidosis.
Keywords: Intoxication; Metformin; Gliclazide; Case report
Abbreviations: T2DM: type 2 Diabetes Mellitus; ECTRs: Extracorporeal Treatments; BP: Blood Pressure; BPM: Beat per Minute; BE: Base excess; BB: Buffer Base; ICU: Intensive Care Unit; CPCR: Cerebral Cardiopulmonary Resuscitation; DIP: Drug-induced pancreatitis
Introduction
Metformin can accumulate lactate in patients with hepatic or renal failure or in patients who eat a high dosage of drugs (suicide attempt). Metformin toxicity, a challenging clinical entity, is associated with a mortality of 30%. Metformin poisoning can cause severe toxicity, including death. Various treatments are used, in particular extracorporeal treatments (ECTRs) such as hemodialysis and hemofiltration. Indeed, a recent literature review noted that metformin poisoning was the most common toxicological indication for ECTR [1]. Metformin poisoning with lactic acidosis appears to be amenable to extracorporeal treatments [2]. Gliclazide, a sulfonylurea molecule, is used to control glycaemia in patients with diabetes mellitus type II. Acute and chronic toxicity studies with gliclazide, conducted in various animal species, have demonstrated very low toxicity. The LD50 was calculating 330-1300 times greater than the dose administered to humans. However, there are also case reports in which a patient developed acute renal failure due to low acute tubular necrosis following massive gliclazide ingestion in a suicide attempt [3]. In the case report [3] 42-year-old male ingested 350 tablets (28 grams) of gliclazide and survived after 20 days of hospitalisation. In our case report, the patient took 9 grams of metformin and 5.7 grams of gliclazide together after three days.
Patient Information
A 53-year-old patient with a personal history of type 2 Diabetes Mellitus (T2DM) was treated with metformin 1000 mg twice daily and gliclazide 60 mg twice daily, otherwise, without a personal history of treating other chronic diseases. He smoked about 40 cigarettes a day and was an occasional alcohol consumer.
Clinical Findings
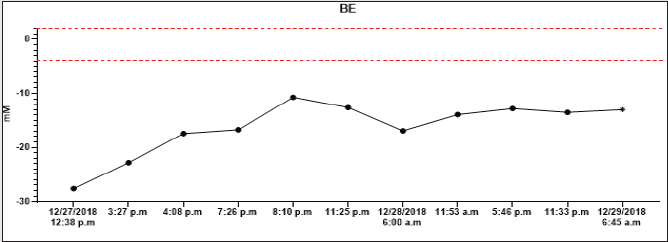
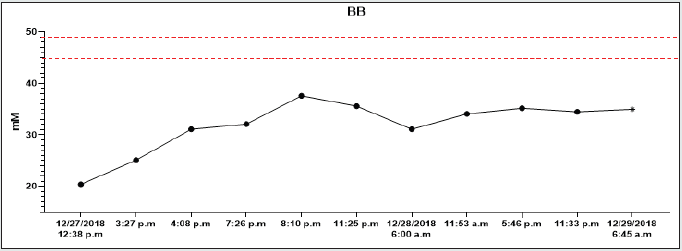
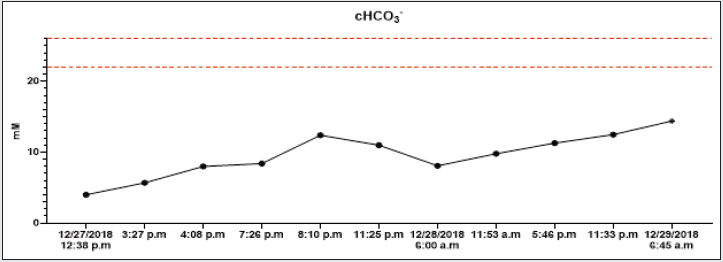
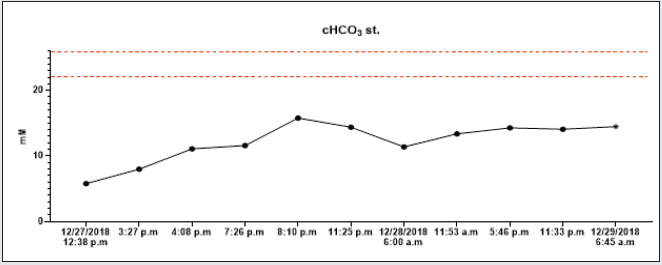
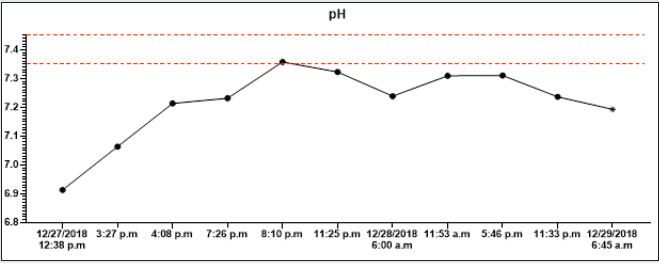
On December 26th, 2018, in the evening hours, he consumed 90 tablets of metformin 1000 mg (total dose 90 grams) and 95 tablets of gliclazide 60 mg (total dose 5.7 grams) for suicide. According to the report, he had been sicking all night and suffered from muscle pain, diarrhoea, and vomiting. On the next (in December 27th2018), he called the emergency. The patent was hypotensive (blood pressure (BP) 80/60 mmHg), and O2 saturation was 94% on its arrival. In the clinical picture, tachypnoea and hyperventilation were present-the hospital’s personal transported the patient to the emergency room. By admission, the patient was still hypotensive (BP 82/45 mmHg), heart rate was 80 beats per minute (BPM), hypoxemic (saturation O2 only 85%), and cyanotic. He had tachypnoea (30 breaths per minute) and Kussmaul’s breathing. The lab test results depicted hyperglycaemia (26mM), renal insufficiency (urea 9.21mM, serum creatinine 288.4mmM), hyperosmolality (340mOsm/l), and elevated levels of myoglobin (998,0ug/l). There was present severe metabolic acidosis pH: 6.913, Base excess (BE): -27.6 mM, Buffer base (BB): 20.40 mM, cHCO3-: 4.00 mM, cHCO3 stand.: 5.80 mM. The anion gap was 44.0 mM (corrected to albumin level 45.08 mM), delta ratio 2.3, delta gap 32.0.
Diagnostic Assessment
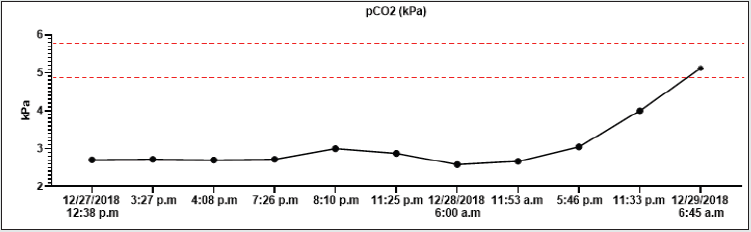
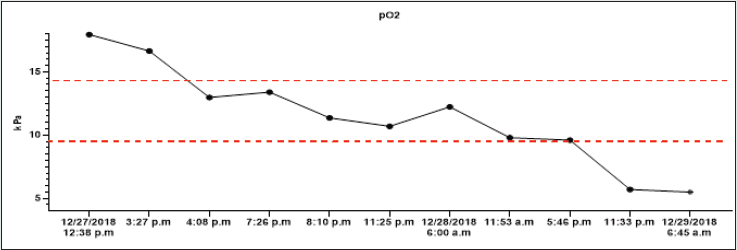
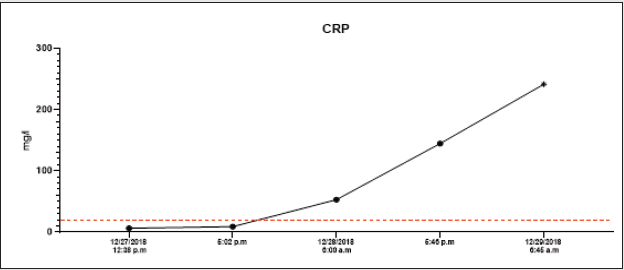
All lab tests were completed from 12/27/2018 to 12/29/2018, and all results were on graphs (Graphs 1A-1H). A high anion gap metabolic acidosis was the result of the diagnosis. As a consequence of metformin intoxication, the lactate level elevated (24mM). We started the treatment with 500 ml 4.2% bicarbonate infusion, omeprazole 40 mg and metoclopramide IV 10mg. On account of hypotension, norepinephrine was moreover given, followed by empiric antibiotic treatment (cefotaxime 2g). The patient was admitted to the Intensive Care Unit (ICU). The therapy continued with rehydration and bicarbonate infusions (1000 ml of 4.2% NaHCO3, 1500 ml of FR 1/1), vasopressor support of norepinephrine.
The Therapeutic Intervention
Because of the intoxication and severe metabolic acidosis, we indicated urgent haemodialysis. Dialysis has lasted for 8 hours, with ultrafiltration of 400 ml. As a result of the hypotension, the norepinephrine dose (to 0.3 μg/kg/min) was necessary to increase. As the next step, an infusion of 20% glucose was continuously administered intravenously to maintain normoglycemia. Due to the progressing of acute renal failure, another haemodialysis was identified. On the next day, inflammation markers increased (CRP: from 6.40 to 241.68 mg/L), and there was an elevation of amylases (39.53 mkat/l) and lipases (60.58 mkat/l). We construed it as drug-induced pancreatitis, which is also described for metformin overdoses.
Follow-up and Outcomes
On December 29th, 2018, in the morning hours, and asystole occurred. For that reason, Cerebral Cardiopulmonary Resuscitation (CPCR) was initiated. There was only electromechanical dissociation despite twenty-five minutes of effort without a palpable pulse present, and the patient passed away. The patient died 2.5 days after intoxication and 1.5 days after admission to the hospital of multiple organ failure, although we had provided aggressive management, including continuous renal replacement therapy.
Discussion
In an extensive series of metformin-treated patients with lactic acidosis reported, 55% of patients survived, and these patients had a median arterial lactate level of 13.1mM. Neither arterial lactate levels nor plasma metformin concentrations were of prognostic significance concerning mortality in this sample of metformintreated patients with lactic acidosis. Death in these patients appeared instead to be associated with other hypoxic diseases or underlying ill-health [3]. Some other case reports referred to fatal metformin intoxication also despite aggressive treatment together with ECTR [4]. Metformin intoxication should be highly suspected if patients have presented with a wide anion gap metabolic acidosis after a suicide by taking drugs. Haemodialysis or continuous renal replacement therapy should be initiated as soon as possible with other supportive care. Patients with acute metformin overdose who died had much lower serum pH nadirs and much higher peak serum lactate and metformin concentrations than those who survived [5]. Although our patient’s clinical problems combined metformin and gliclazide poisoning, there concluded in anion gap metabolic acidosis, renal failure, and drug-induced pancreatitis. Druginduced Pancreatitis (DIP) is assumed to be a relatively rare entity, and its incidence is reported between 0.1 and 2% of acute pancreatitis cases [6-8]. However, the true incidence of DIP is still unknown. Little evidence has been obtained from clinical trials. Most incidences have been documented as case reports generally limited by the absence of inadequacy of diagnostic criteria for acute pancreatitis, failure to rule out common etiologies of acute pancreatitis, and lack of a re-challenge test. Metformin is one of the most widely prescribed oral hypoglycemic agents, linked to pancreatitis, secondary to overdose or in case of impaired renal function [9,10]. This medication is safe if not used in the presence of contraindications - renal failure, liver disease, alcohol abuse, or congestive heart failure [11]. In our case, there was present a combination of metformin overdose and renal failure. The exact pathomechanism is unknown, but toxicity is probably secondary to acinar cell injury leading to intercellular leakage of digestive enzymes from ductules [12]. Also, sulphonylureas, another widely prescribed drug class, has been implicated in causing acute pancreatitis. Most case reports and population-based casecontrol studies of DIP were possibly related to glimepiride, and another possibly due to gliclazide were published in a French gastroenterology journal [13].
Patient Perspective
Our patient took the combination of metformin and gliclazide poisoning, there concluded in anion gap metabolic acidosis, renal failure, and drug-induced pancreatitis with fatal results.
Conclusion
Metformin and gliclazide are effective antidiabetic drugs in patients with type 2 diabetes mellitus. Although antidiabetics are not commonly used for intoxication in suicide attempts, our case report describes fatal intoxication with metformin and gliclazide. The message is to remember the risk of daily used antidiabetic drugs-in high doses, in combinations, they can lead to pancreatitis, renal failure, or so long-known lactic acidosis.
References
- Mardini J, Lavergne V, Roberts D, Ghannoum M (2014) Case reports of extracorporeal treatments in poisoning: historical trends. Semin Dial 27: 402-406.
- Calello DP, Liu KD, Wiegand TJ, Roberts DM, Lavergne V, et al. (2015) Extracorporeal Treatment for Metformin Poisoning: Systematic Review and Recommendations From the Extracorporeal Treatments in Poisoning Workgroup. Crit Care Med 43: 1716-1730.
- Barracca A, Ledda O, Michittu B, Pili GF, Manca O (1998) Acute renal failure after massive ingestion of gliclazide in a suicide attempt. Renal Failure 20: 533-537.
- Lalau JD, Race JM (1999) Lactic acidosis in metformin-treated patients. Prognostic value of arterial lactate levels and plasma metformin concentrations. Drug Saf 20: 377-384.
- Chang CT, Chen Y, Fang J, Huang C (2002) High anion gap metabolic acidosis in suicide: Don't forget metformin intoxication--two patients' experiences. Ren Fail 24: 671-675.
- Dell'Aglio DM, Perino LJ, Kazzi Z, Abramson J, Schwartz MD (2009) Acute metformin overdose: examining serum pH, lactate level, and metformin concentrations in survivors versus nonsurvivors: a systematic review of the literature. Ann Emerg Med 54: 818-823.
- Nitsche CJ, Jamieson N, Lerch MM, Mayerle JV (2010) Drug-induced pancreatitis. Best Pract Res Clin Gastroenterol 24: 143-155.
- Wolfe D, Kanji S, Yazdi F, Skidmore B, Moher D (2019) Methods for the early detection of drug-induced pancreatitis: a systematic review of the literature. BMJ Open 9: e027451.
- Alsubaie S, Almalki MH (2013) Metformin induced acute pancreatitis. Dermato-endocrinology 5: 317-318.
- Giorda CB, Nada E, Tartaglino B, Marafetti L, Gnavi R (2014) A systematic review of acute pancreatitis as an adverse event of type 2 diabetes drugs: From hard facts to a balanced position. Diabetes Obes Metab 16: 1041-1047.
- Nisse P, Mathieu‐Nolf M, Deveaux M, Forceville X, Combes A (2003) A Fatal Case of Metformin Poisoning. Journal of Toxicology: Clinical Toxicology 41: 1035-1036.
- Mallick S (2004) Metformin induced acute pancreatitis precipitated by renal failure. Postgrad Med J 80: 239-240.
- Krentz AJ, Patel MB, CJ Bailey (2008) New drugs for type 2 diabetes mellitus: What is their place in therapy?. Drugs 68: 2131-2162.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...