Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1725
Research Article(ISSN: 2641-1725) 
Continue Lumbar Drainage for Intracranial Pressure Control of HIV-Associated Cryptococcal Meningitis Patients from Low to Middle Income Area/Country Volume 5 - Issue 3
Zezhou Wu1, He Luan1, Jianglong Qin2, Fang Xiao1, Peiqi Wan1 and Boming Liao1*
- 1Department of Infectious Diseases, 1st Affiliated Hospital of Guangxi Medical University, Nanning, Guangxi, P. R, China
- 2Department of Infectious Diseases, Nanning Infectious Hospital, Guangxi Medical University, Nanning, Guangxi, P. R. China
Received: September 15, 2020; Published: September 24, 2020
*Corresponding author: Boming Liao, Department of Infectious diseases, 1st Affiliated Hospital of Guangxi Medical University, Nanning, Guangxi, PR China
DOI: 10.32474/LOJMS.2020.05.000215
Abstract
Background: The aim of this pilot study was to compare the intracranial pressure (ICP) control between the continuous lumbar drainage (CLD) and repeated lumbar puncture (LP) on the patients with HIV-associated Cryptococcal Meningitis (CM).
Methods: From January 2017 to January 2019, a total of forty patients with HIV-associated CM patients were randomized and allotted into CLD or repeated LP groups, respectively. During the first two weeks of the treatment, either CLD or LP were used to control the ICP pressure except the routine antifungal therapy was given following the consensus and guidelines of CM. The ICP pressure, protein concentration and cell count from CSF were assayed and compared between the two groups.
Result: All the patients were survived. At the day 14 post treatment, a drop in ICP was observed among patients and clinical symptoms were relieved. The ICP of CLD group was significantly lower than those of LP group(P<0.05). The protein concentration and cell count from CSF of CLD group were significantly less than LP group(P<0.05).
Conclusions: CLD is a simple, safe or the first-choice control of intracranial hypertension in the patients with HIV associate cryptococcal meningitis. Especially, for patients were treated in primary and/or secondary hospitals located at the low-middle income areas/country.
Keywords: HIV-associated; cryptococcal meningitis; continuous lumbar drainage; low-middle income; cerebral spinal fluid; intracranial pressure
Abbreviations: HIV: Human Immunodeficiency Virus; CM: Cryptococcal Meningitis; ICP: Intracranial Pressure; CLD: Continuous Lumbar Drainage; LP: Lumbar Puncture; CSF: Cerebral Spinal Fluid; ART: Antiretroviral Therapy
Introduction
Cryptococcal meningitis (CM) is the most important causes of death among the human immunodeficiency virus associated (HIVassociated) patients in worldwide [1]. The mortality rate is up to 30% even in developed countries [2]. Mortality from cryptococcal meningitis in resource-limited settings is approximately 70% [3]. Survivor of CM often developed major irreversible neurological impairments like blindness and deafness. Besides the standard antifungal and antiretroviral therapy (ART), the management of elevated of intracranial pressure (ICP) plays a very important role in reducing the mortality and morbidity of HIV-associated CM patients, especially in the first two weeks post treatment. Along with medication, invasive therapeutic approaches are necessary for managing of the intracranial hypertension in CM patients. Presently, repeated lumbar puncture, drainage of cerebrospinal fluid (CSF) and Ventriculoperitoneal shunting (VP) are the main invasive methods used to reduce the ICP. If the patient is from a lower to middle income area and/or country and is hospitalized in the primary and secondary care hospital, the option for the ICP control will focus on continuous lumber drainage (CLD) and repeated lumber puncture (LP) rather than VP operation. A pilot prospective study was conducted to compare the CLD and LP within the first two weeks of onset of CM.
Materials and Methods
From Jan 2017 to Dec 2019, a total of forty patients diagnosed
with HIV-associated CM were recruited into this prospective
study. The written informed consent was obtained from each
patient. This study was approved by Ethical Committee of the
First Affiliated Hospital and infectious disease hospital of Guangxi
Medical University and has been performed in accordance with the
Declaration of Helsinki. The patients were randomized and divided
into the CLD group and repeated lumbar puncture (LP) group as
control. All the data obtained from the two groups are listed in
Table 1. The treatments followed the recommended guidelines from
IDSA 2010 [4] and Chinese medical association [5]. The treatment
includes primary therapy (induction and consolidation steps) and
maintenance therapy. The repeated LP was performed at the day 0,
2, 5, 7, 9,12 and 14 post the onset of treatment. The procedure of
CLD is as following:
a) Patient was in lateral recumbent position under close
monitoring.
b) A soft and sterile catheter (18 gauge) of lumbar drainage
was placed through the lumbar vertebral L4-5 interspace.
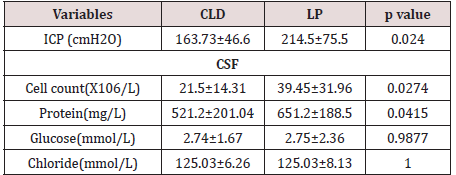
Table 1: Clinical features of forty HIV-associated CM.
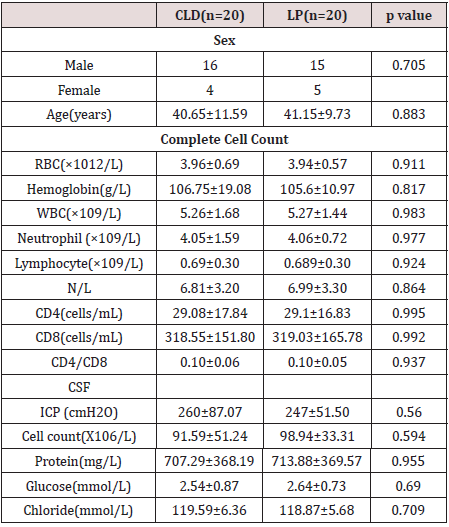
CLD: Continuous Lumbar Drainage, LP: Lumbar Puncture, RBC: Red Blood Cells, WBC: White Blood Cells, CSF: Cerebrospinal Fluid, ICP: Intracranial Pressure.
Total 3 4 cm long catheter tube was inserted and fixed. Another side of tube was cap and attached to a container for collecting CSF. The drainage level was kept at the same as the patient’s bed. The drainage speed was adjusted to 10- 20 ml per hour and the maximal daily drainage of CSF volume was under 400 ml. The drain was kept in place for up to two weeks. The ICP was monitored and recorded every 10 min during first 6 hours of procedure and every hour in first 72 hours. Then interval of observation was 2 hours within first 7 days and 3 hours between day 8 to 14. All the patients and their vital signs were monitored closely. The clinical outcomes and adverse effects were evaluated and monitored daily. The routine CSF assays were done, and results are expressed in Table 2. These assays include the pressure of CSF; cell counts and classification; the levels of protein, glucose, and chloride from CSF. Results are listed in Table 2.
Statistical analysis
Values are expressed as mean± SD. The P value <0.05 was considered statistically significant. Statistical analysis was performed by using a statistical software package (IBM® SPSS® Statistics, Version 19.0).
Results
All the patients survived by the end of day 14 post treatment either using CLD or LP. The catheter was changed after 14 days. No sign of sepsis or infections signs were observed at the site of puncture. As Table 2 demonstrated the CSF assay results. The ICP levels dropped in both methods, either CLD or LP. CLD group showed a significantly lower ICP values than LP group (P<0.05). The levels of protein and total cell counts from CSF has a significantly difference between the CLD group and LP group (P<0.05). However, the glucose and chloride values in CSF of both groups showed marginal differences (P>0.05).
Discussion
For HIV infected patients, the CM is one of the most common complication due to the patient’s immunodeficiency. The management of intracranial hypertension of these patients at the early stage of treatment are the critical to reduce the mortality of CM. Several guidelines for use of antifungal therapy on these patients, in low-income and middle-income counties are available [6]. One of the bigger challengers for clinicians is to control the ICP and reduce the symptoms as well its side effects. So far, besides the drug administration for the control of ICP, lumbar puncture (LP) and surgical shunt operation are two commends to control ICP and relief the symptoms for patients in worldwide [7]. Surgical shunt operation still needs the availability of highly trained surgeon and professional personnel. This surgical procedure is mostly conducted in the tertiary level hospitals. The demand of expensive equipment and the cost for the patients from the lower-middle income families remain a burden to the country. Obviously, for most patients with HIV associated CM, the primary and initial treatment was started at the primary and secondary level hospitals. Therefore, choice of either CLD or repeated LP to control ICP is priority decision taken by the physicians at these healthcare centers. Repeated LP during the first 1-2 weeks after onset of CM may cause the cerebral hernia and these procedures and interventions are very painful and stressful for the patients. From our preliminary pilot study, data shows that CLD is a more efficient method to reduce ICP. The levels of cell count and protein from CLD group were significantly lower than those of LP group. The possible reason may be related to better effectiveness of CDL to reduce the accumulation of CSF and enhanced elimination of cryptococcus from center nervous system. After controlling the ICP levels, the symptoms and signs of CM patients were relieved. In general, CLD is a safe and efficacious procedures in most patients [8,9].
Conclusions
From our pilot prospective study results indicated that the continuous lumbar drainage may be first choice to control ICP of HIV associated CM patients who are from lower to middle income area/country and initially treated at the primary and secondary hospitals, especially during the first crucial two weeks. Our preliminary study is first available to compare CLD and LP and a large multiple hospital study will be pursued in our area soon.
Acknowledgements
The authors would thank Dr Guanghan Luo, Dr Liyi Huang, Dr Jizhou Wu and Dr Jianning Jiang for their suggestions and critical review. Authors also want to thank all the patients who participants and contributed to this study.
Funding
This study was granted by the Health department, Guangxi Zhuang autonomous regions, P.R. China. But funding agency did not have the role in study design, data collection, analysis, as decision for publish and the preparation of the manuscript.
Conflict of interest
The authors declare that there are no conflicts of interest regarding the publication of current paper.
References
- (2018) World Health Organization (WHO) Guidelines for the diagnosis, prevention, and management of cryptococcal disease in HIV-infected adults, adolescents and children. Geneva: World Health OrganizationLicenseCC BY-NC-SA30 IGO pp: 62.
- Wu X, Shen Y (2019) Management of human immunodeficiency virus–associated cryptococcal meningitis: Current status and future directions. Mycoses 62(10): 874-882.
- Rajasingham R, Smith RM, Park BJ, Jarvis JN, Govender NP, et al. (2017) Global burden of disease of HIV-associated cryptococcal meningitis: an updated analysis. The Lancet infectious diseases 17(8): 873-881.
- Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR, et al. (2010) Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the Infectious Diseases Society of America. Clinical infectious diseases 50(3): 291-322.
- Liu ZY, Wang GQ, Zhu LP, Lyu XJ, Zhang QQ, et al. (2018) Expert consensus on the diagnosis and treatment of cryptococcal meningitis. Zhonghuaneike za zhi 57(5): 317-323.
- Loyse A, Burry J, Cohn J, Ford N, Chiller T, et al. (2019) Leave no one behind: response to new evidence and guidelines for the management of cryptococcal meningitis in low-income and middle-income countries. The Lancet Infectious Diseases 19(4): e143-e147.
- Liu Y, Peng X, Weng W, Zhu J, Cao H, et al. (2019) Efficacy of ventriculoperitoneal shunting in patients with cryptococcal meningitis with intracranial hypertension. International Journal of Infectious Diseases 88: 102-109.
- Hussein M, Abdellatif M (2019) Continuous lumbar drainage for the prevention and management of perioperative cerebrospinal fluid leakage. Asian journal of neurosurgery 14(2): 473-478.
- Macsween KF, Bicanic T, Brouwer AE, Marsh H, Macallan DC, et al. (2005) Lumbar drainage for control of raised cerebrospinal fluid pressure in cryptococcal meningitis: case report and review. Journal of Infection 51(4): e221-e224.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...