
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1725
Case Report(ISSN: 2641-1725) 
Complete Second Branchial Cleft Fistula Associated with Branchial Cyst: A Rare Case Scenario Volume 6 - Issue 2
Pavan T Lanjewar*, Sarojini Jadhav, Omar Khan and Vishakha Iyer
- Department of General Surgery, Government Medical College and Hospital, India
Received: July 18, 2022 Published: July 29, 2022
*Corresponding author: T Lanjewar, Department of General Surgery, Government Medical College and Hospital, Aurangabad, India
DOI: 10.32474/LOJMS.2022.06.000234
Abstract
Branchial arch anomalies are one of the differential diagnoses in patients of neck pathology during early childhood. Branchial anomalies of second arch being the most common among these anomalies. A complete fistula communicating with a branchial arch cyst is a very rare congenital anomaly of the branchial apparatus. These anomalies present on lateral aspect of neck anterior to sternocleidomastoid. Branchial cleft anomalies are usually asymptomatic and may present with mucoid discharge from the tract. The present case is 11-year-old boy with complete second branchial cleft fistula associated with branchial cyst managed by excision.
Keywords: Branchial Arch; Branchial Cleft Anomalies; Sternocleidomastoid
Introduction
Branchial arches in an embryo starts to form at around 4th week and total six paired branchial arches are formed in craniocaudal succession on either side of the pharyngeal foregut. During the embryonic development, the second arch grows caudally; envelops the third, fourth, and sixth arches; and forms the cervical sinus by fusing with the skin caudal to these arches. The ectoderm inside the fused tube disappears, while the edges of cervical sinus fuse. Anomalies of the second branchial arch are most common developmental anomalies (cysts, sinuses, fistulae or cartilaginous remnants) of the branchial apparatus counting up to 90% followed by first arch [1-3]. Complete second arch fistula with internal opening into the tonsillar region is rare and comprises 2% of all branchial anomalies [2]. Branchial fistula associated with a branchial cyst is an unusual presentation [4]. Branchial fistula usually present in childhood as a continuously discharging defect along the anterior border of sternocleidomastoid muscle at the junction of middle and lower 1/3rd of neck. The second branchial cleft and pouch fistula pass from the external opening in the mid or lower one-third of the neck at the anterior border of the sternocleidomastoid muscle, deep to the platysma along the carotid sheath, then pass medially deep between the internal and external carotid arteries after crossing over the glossopharyngeal nerve and hypoglossal nerve. Finally, it opens internally either on the anterior face of the upper half of the posterior pillar of the fauces or in the intratonsillar cleft in the tonsillar fossa [5].
Case Report
An 11 year old boy presented with chief complaints of opening over right side of neck since childhood with intermittent discharge from the opening since then. There was no past history of trauma or any surgical intervention. On examination, a pinpoint opening of size less than 0.1 x 0.1cm was present over right side neck at the skin over the junction of middle and lower third of anterior border of sternocleidomastoid with no active discharge while mucoid discharge expressed on pressing over the region. There were no local signs of inflammation. Patient had no associated upper respiratory tract infection. Per oral examination does not show any evidence of obvious opening or any discharge. Patient was investigated with Conventional Xray fistulogram showing evidence of opacified complete branchial fistula tract with cyst. Further, he was investigated by MRI fistulogram with administration of saline into the external opening showing second branchial cleft fistula with cyst (type III according to Bailey Classification).
Patient felt the contrast material fluid injected into the fistula tract coming inside the moth while investigations. Based on the clinical history and imaging, a diagnosis of complete branchial fistula in association with branchial cyst of second arch was considered. Patient was operated by brachial fistulectomy by external approach in following steps: Elliptical skin incision taken around the opening, incision deepened, underlying tract identified and dissected from surrounding structures till just above the level of submandibular gland almost in the area around the tonsillar fossa, the tract ligated at the base and around 6 cm length of tract excised. Inner surface of the tract was having mucosal lining with content of tract having mucinous consistency. Surgery was uneventful and patient tolerated the procedure well. Histopathology report was consistent with findings of branchial cyst and fistula. Patient was discharged uneventfully. Patient is followed up at 6 months after the procedure with no evidence of any recurrence (Figures 1-8).
Figure 6: Excised branchial fistula tract with cyst part cut opened. Evidence of inner mucosal surface of tract.
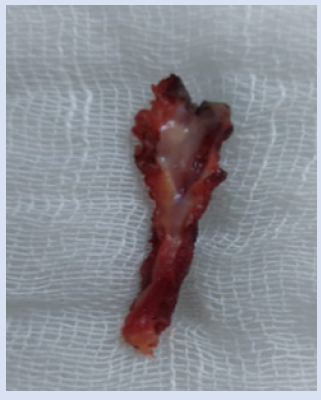
Figure 8: Postoperative clinical photograph at 6 month follows up. Evidence of scar mark at operative site.

Discussion
Von Baer first described the branchial apparatus, while anomalies in its development were described by Von Ascheron [6]. Anomalies of the second branchial arch are most common developmental anomalies (cysts, sinuses, fistulae or cartilaginous remnants) of the branchial apparatus. During 4-7th gestation, the second arch grows caudally and covers the 3,4 and 6th arches leading to formation of cervical sinus of His with the epipericardial ridge of the fifth arch. The ends of the sinus fuse and no defects are seen. The most common theory accepted was an incomplete obliteration of the branchial arch cleft or buried epithelial cells [7,8]. Bailey classified the second branchial cleft cysts into 4 subtypes, Type lies deep to platysma, anterior to sternocleidomastoid. Type II (most common type) lies abutting internal carotid artery and adherent to internal jugular vein, runs posterior to the submandibular gland. Type III runs along the lateral pharyngeal wall between the internal and external carotid arteries while Type IV arises from the pharyngeal mucosal space [9]. A branchial cleft cyst may often be associated with upper respiratory tract infection. If cyst get infected, shows signs of inflammation and become tender or may enlarge in size to produce symptoms like dysphagia, dyspnea and dysphonia [10]. Branchial cleft cyst can progress to carcinomas if left untreated [11]. Patient with branchial fistula usually present during childhood and early adolescence, with mucoid discharge from the opening at the anterior border of sternocleidomastoid being common symptom at presentation. Investigations like CT and MRI base of skull + neck aids in diagnosis. Surgical excision through trans cervical approach by single or stepladder incisions and combined pull through technique are the treatment options. Recurrence is one of the long-term complications of the surgery with 3% recurrence rate in fresh cases and 20% after second attempt of surgery, with other complications being secondary infection, injury to facial, hypoglossal, glossopharyngeal, spinal accessory nerves, injury to internal jugular vein, bad scar and hematoma formation [12].
Conclusion
Amongst the branchial arch anamolies, though second branchial cleft anamolies are most common but complete second branchial cleft fistula in association with branchial cyst is a rare occurrence. Treatment with complete excision of fistula tract during initial surgery is warranted with postoperative surveillance for recurrence.
Conflict of Interest
No competing interests.
Funding
No funding agency.
References
- Adams A, Mankad K, Offiah C, Childs L (2016) Branchial cleft anomalies: a pictorial review of embryological development and spectrum of imaging findings. Insights Imaging 7: 69-76.
- Ford GR, Balakrishnan A, Evans JN, Bailey CM (1992) Branchial cleft and pouch anomalies. J Laryngol Otol 106: 137-143.
- Burton MG (1980) Second branchial cleft cyst and fistula. Am J Radiol 134(5): 1067-1069.
- Sumana B, Sahaja K, Kalyani B, Swarupa K, Rao VRK (2019) Branchial Cyst with Branchial Fistula: A Rare Association. Indian J Otolaryngol Head Neck Surg 71(1): 633-636.
- Talaat M (1992) Pull-through branchial fistulectomy: technique for the otolaryngologist. Ann Otol Rhino Laryngol 101(6): 501-502.
- De PR, Mikhail T (1995) A combined approach excision of branchial J Laryngol Otol 109: 999-1000.
- Maran AG, Buchanan DR (1978) Branchial cysts, sinuses and fistulae. Clin Otolaryngol 3(1): 77-925.
- Liston SL, Siegel LG (1979) Branchial cysts, sinuses, and fistula. Ear Nose Throat J 58: 9-17.
- Bailey H (1923) The clinical aspects of branchial cysts. Br J Surg 10(40): 173-182.
- Lee HJ, Kim EK, Hong S (2006) Sonographic detection of intrathyroidal branchial cleft cyst: a case report. Korean J Radiol 7(2): 149-151.
- Bernstein A, Scardino PT, Tomaszewki MM, Cohen MH (1976) Carcinoma arising in a branchial cleft cyst. Cancer 37(5): 2417-2422.
- FC Agaton-Bonilla, Cosmay GE (1996) Diagnosis and treatment of branchial cleft cysts and A retrospective study of 183 patients. Int J Oral Maxillofac Surg 25: 449-452.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...










