
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1725
Case Report(ISSN: 2641-1725) 
Combination of Turner Syndrome Crohn’s Disease and Thyroiditis a Rare Occurrence Volume 6 - Issue 1
Rewanth R Katamreddy, Saraswathi Lakkasani*, Gowthami Sai Kogilathota Jagirdhar, Scott Digiacomo and Yatinder Bains
- Department of Gastroenterology and Department of Internal Medicine, Saint Michael’s Medical Center in New York Medical College, USA
Received: January 25, 2022 Published: February 2, 2022
*Corresponding author: Saraswathi Lakkasani, Department of Gastroenterology and Department of Internal Medicine, Saint Michael’s Medical Center in affiliation with New York Medical College, USA
DOI: 10.32474/LOJMS.2022.06.000231
Abstract
Turner’s syndrome is a genetic condition in the female population caused by the partial or complete loss of X-Chromosome. Previous case reports in the literature and prior studies established the association between Turner’s syndrome and multiple Autoimmune Diseases (AID). We present a 38-Year-old female with Turner’s syndrome, Thyroid disease and multiple admissions for Fistulizing Crohn’s disease. X chromosome deletions and alterations predispose to auto-immune antibodies per prior studies.
Introduction
Turners Syndrome is seen in 1 in 2000 to 1 in 2500 live female births. Predisposition for Autoimmune Diseases (AID) occurs in 30- 40% of these patients. In the past there have been cases reported with Turner syndrome and Inflammatory bowel disease, and Turner syndrome and Thyroiditis. However, there is limited data reporting the combination of multiple autoimmune diseases: Turner syndrome, Inflammatory Bowel Disease, and Thyroiditis. In light of this we present a case of Turner syndrome, associated with hypothyroidism and Crohn’s disease who underwent partial colectomy with colostomy presenting with Colo-cutaneous fistula.
Case Report
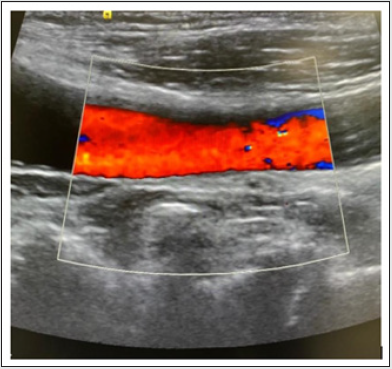
A 38-year-old female who is a known case of Turner syndrome with Hypothyroidism on thyroxine replacement, Crohn’s disease post left hemicolectomy with colostomy and Colo-cutaneous abdominal wall fistula, Osteoporosis with history of femoral neck fracture presented with pus discharging wound on the anterior abdominal wall for a few days. She also had a painful erythematous rash over the right half of the face. On physical examination, her height is 121.9cm and her Weight is 50.5kgs. Hematology workup revealed anemia with Hemoglobin and Hematocrit of 11g/dL and 33.2%. Thyrotropin receptor antibody (TSH Ab) of <1.10 IU/L (Normal range:0-1.7IU/L), Anti-Thyroglobulin Antibody of 1.5 IU/L (Normal Range:0-0.9IU/L) and Anti-Thyroid Peroxidase antibody (TPO Ab) of 35 IU/L (Normal range: 0-34IU/L). CT scan of the abdomen showed evidence of Colo vesical fistula and Peri colonic inflammation with fat stranding (Figure 1). Patient underwent Incision and Drainage of the Colo-cutaneous fistula and placement of Penrose drain. Culture and sensitivities were obtained, and appropriate antibiotics were started. Patient underwent colonoscopy later which showed erythematous, friable mucosa, a hemorrhagic appearance and ulceration 5 cm from the Colostomy opening (Figure 2) Biopsy of the lesion showed preserved crypt architecture and lymphoid aggregates without acute inflammation or lymphocytic infiltration. Patient was followed up with a USG neck which showed a small, heterogeneous, and mildly hyperechoic gland (Figure 3). Patient continues to be on levothyroxine. Dexa scan showed a T score of -3.1 in the lumbar spine and -2.7 in the right hip. Patient is on alendronate. Patient was discharged with followup in the Gastroenterology clinic and is currently on Vedolizumab.
Figure 1: CT Abdomen-Rim-enhancing air and fluid filled fistulous tracts/collections, possibly communicating with each other, extending inferiorly from the colostomy loop within the subcutaneous tissues and towards the skin surface of the left anterior lower abdomen/pelvis.
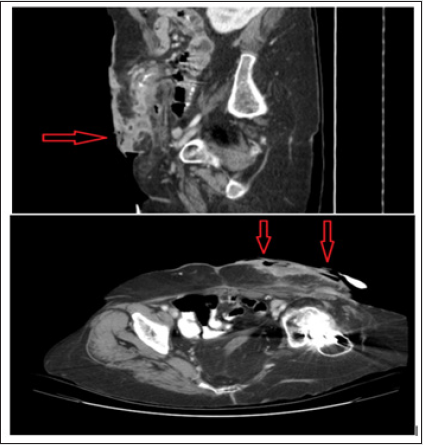
Figure 2: Colonoscopy-Showing patent end colostomy in the transverse colon characterized by erythema, friable mucosa, a hemorrhagic appearance, and ulceration 5cm from colostomy opening.
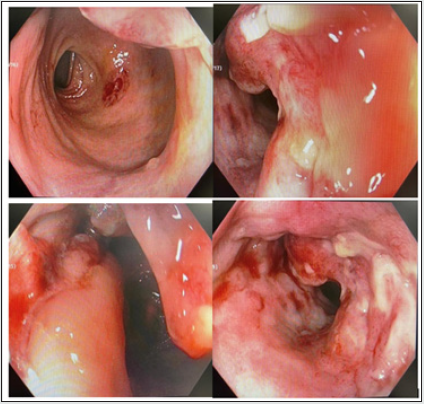
Figure 3: Colonoscopy-Showing patent end colostomy in the transverse colon characterized by erythema, friable mucosa, a hemorrhagic appearance, and ulceration 5cm from colostomy opening.
Discussion
The case mentioned above emphasizes the association of
autoimmune disorders in patients with Turner’s syndrome. Female
sex has a predisposition for AID. Patients with Turner syndrome
have twice the risk compared to the female population. The cause
of autoimmunity in Turner’s syndrome has been theorized and
studied without a definitive answer. X chromosome genes including
a Major Histocompatibility complex were found to play a major role
in immune response [1,2]. Haplo-insufficiency [3,4], alterations and
microdeletions of the X chromosome are one of the major attributed
causes for AID. Turner syndrome females with chromosome Xp
deletion showed a higher prevalence of thyroid and Crohn’s disease
[4].
Lack of exposure to self-antigens in the thymic epithelial
cells and T-cells with autoreactivity can also be the cause for
auto-immunity [2,3]. Turner syndrome patients were found to
have low levels of Immunoglobulin G and M in some studies [5].
Exposure to estradiol treatment has also been debated to be a
trigger for AID development through hormonal imbalance inciting
immunopathogenic response [6]. Further studies on the link
between AID and X chromosome can help to clearly understand the
pathogenetics involved. The most common AID in Turner’s appears
to be related to the thyroid gland. Hypothyroidism is more common
compared to hyperthyroid disease. Ulcerative colitis, Crohn’s
disease, celiac disease, juvenile rheumatoid arthritis, diabetes
mellitus, Addison’s disease, psoriasis, vitiligo and alopecia. This
patient was diagnosed with Hashimoto’s thyroiditis and Crohn’s
disease around the age of 20. The patient had a femoral neck
fracture and osteoporosis diagnosed around 25 years of age. Many
patients have sub clinical presentations and close follow up of
patient’s symptoms is necessary. Medical management in patients
with Turner’s syndrome should include screening and monitoring
for AID regularly with appropriate treatment. The Turner syndrome
study group published guidelines on Screening and medical care for
turner’s syndrome patients.
References
- Goldacre MJ, Seminog OO (2014) Turner syndrome and autoimmune diseases: record-linkage study. Arch Dis Child 99(1): 71-73.
- Larizza D, Calcaterra V, Martinetti M (2009) Autoimmune stigmata in Turner syndrome: when lacks an X chromosome. J Autoimmun 33(1): 25-30.
- Ilaria Bianchi, Ana Lleo, Gershwin ME, Invernizzi P (2012) The X chromosome and immune associated genes. J Autoimmun 38(2-3): 187-192.
- Stoklasova J, Zapletalova J, Frysak Z, HanaV, Cap J, et al. (2019) An isolated Xp deletion is linked to autoimmune diseases in Turner syndrome. J Pediatr Endocrinol Metab 32(5): 479-488.
- Jensen K, Petersen PH, Nielsen EL, Dahl G, Nielsen J (1976) Serum immunoglobulin M, G, and A concentration levels in Turner's syndrome compared with normal women and men. Comparative Study Hum Genet. 31(3): 329-334.
- Bakalov VK, Gutin L, Cheng CM, Zhou J, Sheth P, et al. (2012) Autoimmune disorders in women with turner syndrome and women with karyotypically normal primary ovarian insufficiency. J Autoimmun 38(4): 315-321.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




