
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1725
Case Report(ISSN: 2641-1725) 
An Unusual Location of Metastatic Breast Cancer Volume 3 - Issue 4
Jihene Marrakchi1, Maha Mejbri1*, Mohamed Ben Amor1, Sobhy Houissa2, Ghazi Besbes2 and Hafedh Jemel2
- 1ENT Department, La Rabta Hospital, Tunisia
- 2Neurosurgery Department, Institute of Neurology of Tunis, Tunisia
Received: September 13, 2019; Published: September 30, 2019
*Corresponding author: Maha Mejbri, ENT department, La Rabta Hospital, Tunisia
DOI: 10.32474/LOJMS.2019.03.000167
Abstract
Metastasis of breast cancer in paranasal sinus are rare. Only few cases have been reported until now. The presence of rhinological or neurological signs in a patient with a past history of breast cancer should raise the awareness of the practitioner. The treatment is generally palliative. We report, in this manuscript, the case of a 50-year-old female patient treated for breast cancer ten years ago for breast cancer, who presented with a metastasis to the sphenoid sinus.
Keywords: Breast cancer; paranasal sinus; metastasis; palliative treatment; neurological signs; rhinological signs
Introduction
Breast cancer is the most common cancer in women [1]. The frequent metastatic sites are lymph nodes, lungs, bones, liver and brain [2]. Metastasis to head and neck region, particularly paranasal sinuses are rare. To our knowledge, only few cases have been reported in the literature [3]. Threw this case report, we tried to illustrate the clinical presentation of a metastasis to the sphenoid sinus in a patient with a past history of a breast cancer.
Case Report
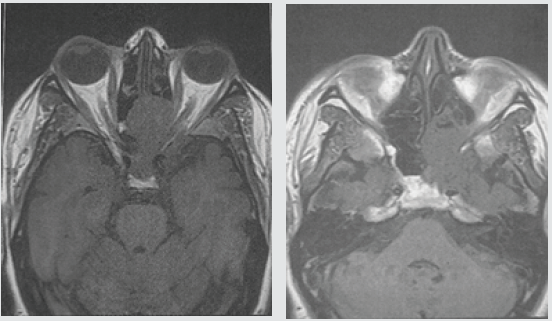
A 50 -year-old diabetic female presented with numbness of the left facial side, decreased visual acuity, diplopia and headaches evolving for 6 months. The patient did not report any rhinological signs. She had a history of left breast cancer ten years ago. She underwent surgery followed by chemotherapy and radiotherapy. No evidence of recurrence has been noticed during the ten years follow up. At the physical examination, the patient was found to have convergent strabismus, left exophthalmia and ptosis. The nasal cavities were tumor free. Computed tomography (CT scan) and magnetic resonance imaging (MRI) showed a 48 mm mass of the left sphenoid sinus with an extension to the cavernous sinus and the ethmoid bone that compresses the left optic nerve (Figure 1). An endoscopic exploration of the sphenoid sinus and multiples biopsies of the tumor were performed. The histopathological examination completed by histoimmunochemical study concluded to a metastasis of intraductal carcinoma. The patient was referred to oncological unit for palliative treatment. She is currently receiving chemotherapy.
Figure 1A & Figure 1B: Axial T1 weighted MRI sequence images: mass of the left sphenoid sinus with an extension to the cavernous sinus and the ethmoid bone that compresses the left optic nerve.
Discussion
Despite being the most frequent cancer in women, metastasis of breast cancer to nasal cavity and paranasal sinuses are very rare [3]. The most common metastatic sites are the sphenoidal, the frontal and the ethmoid sinuses [4]. Few cases were reported in the literature and most of these patients underwent palliative treatment. Their prognosis was poor.
The pathogenesis of tumor spread remains unclear. It is thought to be an hematogenous spread via the prevertebral venous plexus [4]. The lymphatic route is also suggested. It’s exceptional that a distant metastasis is revealed before local recurrence or lymph nodes metastases [5].
The clinical presentation is usually unspecific; thus, the diagnosis is generally delayed [6]. Symptoms may be those of rhinosinusitis. Main signs are: epistaxis, nasal obstruction and facial pain [7]. Orbital signs such as exophthalmia, ptosis, diplopia secondary to abducens palsy or a blurred vision may also occur when the tumor develops into the orbit [8]. Reviewing patient medical history is essential to guide the diagnosis. Patients who express the human epidermal growth factor receptor 2 (HER- 2) have a higher incidence of metastasis to paranasal sinuses compared to HER-2 negative patients [9]. Metastasis generally occurs in the fifth or sixth decades of life [10].
Using imaging techniques is useful; CT scan guides the diagnosis of malignant tumor by showing bone erosion, angiogenesis and invasion of skull base. MRI makes a better study of the extension to the orbit, cranial nerves and intracranial spread. Positron emission tomography (PET scan) is useful to detect earlier lesions [3]. The diagnosis is not always easy to establish. The use of an expanded panel of immunohistochemistry markers helps the achievement of the correct diagnosis.
The therapeutic approach cannot be radical. It aims to improve patient quality life [5]. The treatment is generally palliative based on radiotherapy which purpose to limit tumor spread and to relieve pain [11]. Chemotherapy or hormone therapy can be helpful for some patients. These treatments are associated with improvement of local symptoms and vision. Surgery, if feasible remains palliative and restricted to some cases. It is generally not recommended because complete tumor resection is difficult to obtein. The prognosis is generally poor [12]. Most of patients died few months after diagnosis [4].
Conclusion
Although metastases of breast cancer to nasal cavity and paranasal sinuses are rare, the presence of orbital signs or rhinosinusitis symptoms in a patient with a past history of breast cancer even if it’s cured should raise the awareness of the practitioner. The prognosis remains poor for the majority of reported cases in literature.
Ethical Statement
Authors declares that they have no conflict of interests. The case report is a retrospective study based on patient’s data. There was no experimentation on humans or animals.
References
- Xiong J, Chen J, Zheng L, Yang S, Zhao G, et al. (2017) Rare metastasis to paranasal sinuses from triple-negative breast cancer: A case report and literature review. Medicine 96(47): e8718.
- Johnston J, George M, Karkos PD, Dwivedi RC, Leong SC (2013) Late metastasis to macroscopically normal paranasal sinuses from breast cancer. Ecancermedicalscience 7: 298.
- Xiong J, Chen J, Zheng L, Yang S, Zhao G, et al. (2017) Rare metastasis to paranasal sinuses from triple-negative breast cancer: A case report and literature review. Medicine 96(47): e8718.
- Namad T, Benbrahim Z, Najib R, Mohammed A, Baggar S, et al. (2014) Maxillofacial metastasis from breast cancer. The Pan African medical journal 19: 156.
- Carnelio S, Rodrigues G (2005) Maxillary metastasis of gastric adenocarcinoma. International Journal of Oral-Medical Sciences 3(3): 159-162.
- Weber AL, Stanton AC (1984) Malignant tumors of the paranasal sinuses: radiologic, clinical, and histopathologic evaluation of 200 cases. Head & neck surgery 6(3): 761-776.
- Monserez D, Vlaminck S, Kuhweide R, Casselman J (2001) Symmetrical ethmoidal metastases from ductal carcinoma of the breast, suggesting transcribrosal spread. Acta oto-rhino-laryngologica belgica 55(3): 251-257.
- Barrs DM, McDonald TJ, Whisnant JP (1979) Metastatic tumors to the sphenoid sinus. The Laryngoscope 89(8): 1239-1243.
- Sanna G, Franceschelli L, Rotmensz N, Botteri E, Adamoli L, et al. (2007) Brain metastases in patients with advanced breast cancer. Anticancer research 27(4C): 2865-2869.
- Garrity JA, Henderson JW, Cameron JD (2007) Henderson's orbital tumors: Lippincott Williams & Wilkins, USA.
- Hirshberg A, Shnaiderman-Shapiro A, Kaplan I, Berger R (2008) Metastatic tumours to the oral cavity–pathogenesis and analysis of 673 cases. Oral oncology 44(8): 743-752.
- Ashab Yamin MR, Kalantarhormozi A, Hamdamjo F, Razi Z (2014) Breast ductal carcinoma metastasis to jaw bones: a case report. Novelty in Biomedicine 2(1): 31-35.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




