
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1725
Case Report(ISSN: 2641-1725) 
A Case Report of the Use of a Novel Drug Delivery Device for the Treatment of Chronic Pulmonary Aspergillosis by Local Instillation of Amphotericin B under Radial Bronchial Ultrasound Guidance Volume 6 - Issue 3
Mingzhou Zhang1, Xueping Liu1, Ping Wang1, Guansong Wang1, Dan Fu2 and Zhi Xu1*
- 1Institute of Respiratory Disease, Xinqiao Hospital, Third Military Medical University, China
- 2The Medical Department, 3D Medicines Inc, China
Received: January 27, 2023 Published: February 24, 2023
*Corresponding author: Zhi Xu, Institute of Respiratory Disease, Xinqiao Hospital, Third Military Medical University, China
DOI: 10.32474/LOJMS.2023.06.000240
Chronic Pulmonary Aspergillosis (CPA) is a serious fungal infection of the lung and is often treated clinically by systemic administration of drugs such as oral or intravenous infusions. However, the duration of antifungal treatment is long and the effectiveness is poor, and long-term use of the drug may cause different degrees of damage to liver and kidney function. Therefore, there is a clinical need for a new antifungal treatment method. We have designed a novel drug delivery device that allows local injection of amphotericin B through a catheter after implantation of a guide sheath at the lesion site under Radial Endobronchial Ultrasound (R-EBUS) guidance via bronchoscopy, thereby increasing the local drug concentration and improving the anti-infective effect, while avoiding the adverse effects of reduced drug absorption due to airway reflux. Here, we report a case of chronic pulmonary aspergillosis treated with a new drug delivery device.
Keywords: Chronic Pulmonary Aspergillosis (CPA); R-EBUS; Amphotericin B; Catheter
Introduction
Chronic pulmonary aspergillosis is a relatively rare chronic infectious pulmonary disease caused by Aspergillus in immunosuppressed and pre-existing lung disease patients [1]. Aspergillus fumigatus infection accounts for more than 90% of cases [2,3]. Current treatment options for chronic pulmonary aspergillosis remain limited. Surgical indications are rare in patients with chronic pulmonary aspergillosis. Common alternatives for contraindications to surgery include intraluminal instillation or endobronchial administration of antifungal drugs [4]. Bronchoscopy plays an important role in the diagnosis and treatment of pulmonary aspergillosis. R-EBUS is a minimally invasive bronchoscopic technique that views structures within and adjacent to the airway wall, targeting deeper structures [5], and is commonly used to determine the exact location of extrabronchial lesions by ultrasound. Previous studies [6,7] have demonstrated the clinical success of transdermal intrathecal administration of amphotericin B under CT (Computed Tomography, CT) guidance. We present a case of an elderly male with CPA who was infused with amphotericin B under R-EBUS-guided using a novel delivery device of our design.
Case Report
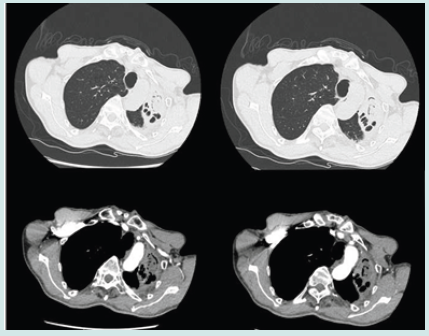
In May 2020, a 63-year-old male patient presented to our outpatient clinic with a cough, expectoration and blood in the sputum with no apparent inducements. He was diagnosed with Aspergillus infection and antifungal treatment was recommended, but he did not use antifungal medication for his own reasons. He underwent closed chest drainage for pneumothorax in 2005, kidney stone surgery in 2015 and rectal polypectomy in 2020. To make matters worse, his cough, expectoration and blood in sputum tended to deteriorate since April 2021. Combined chest CT and bronchoscopic findings suggest CPA (Figure 1). NGS examination of the pathogen of lavage solution suggested Aspergillus fumigatus. Subsequently, he received oral voriconazole antifungal therapy for one month with no significant change in lung lesions and persistent symptoms.
Figure 1: Chest CT showed bronchial dilatation and chronic inflammation in the anterior and posterior segments of the upper lobe of the left lung, with destruction of the left lung. Fibreoptic bronchoscopy showed a patent, twisted left main bronchus with congested mucosa. A large amount of purulent secretions was seen in the right branch of the left upper lobe.
On 7 June 2021, the patient was referred to our department and underwent relevant examinations. Physical examination showed good healthy condition, but the lesion was solidly enhanced compared to the previous CT (Figure 2). Combined with the patient’s previous examination results, he was diagnosed with left CPA. The patient was unable to undergo surgical resection due to adhesions in the chest wall and poor lung function. We decided to infuse amphotericin-B into the left upper lesion under the guidance of R-EBUS. First, the bronchoscope was passed through the nasal approach into the trachea and local anaesthesia was performed by injecting 2% lidocaine (<15 ml) into the trachea/right and left bronchi through a bronchoscopic biopsy forceps. A white secretion from the posterior segment of the left upper lobe tip (Figure 3A) is flushed and cleaned. Then, a sterile catheter was placed into the tip of the left upper lobe of the lung with a guide wire and secured in the bronchus with a rubber plug under R-EBUS guidance (Figures 3B & 3C). Prior to administration, we reconfirmed that the position of the catheter had not moved by direct auscultation or CT. Then 5 mg of amphotericin B was dissolved in 10 ml of saline and injected into the left bronchus via the catheter within 5 minutes. The same dose of drug was administered once daily for four days. The catheter and rubber plug were removed after the fourth intrabronchial instillation of amphotericin B. A total of 20 mg of amphotericin B was administered during the treatment period and oral voriconazole was continued after discharge.
Figure 2: After 1 month of oral voriconazole, preoperative CT examination showing left upper lobe bronchiectasis with obstructive atelectasis and inflammation. The upper left pleura was thickened.
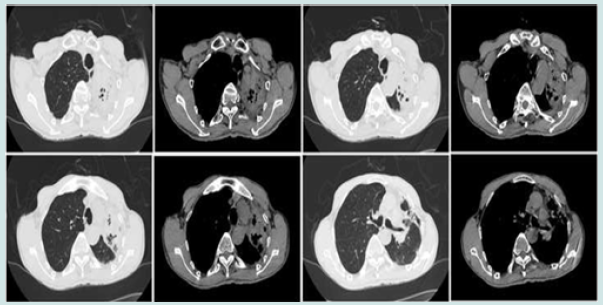
Figure 3: 3A. Preoperative tracheoscopic image showed a large purulent secretion. 3B. R-EBUS localization image. 3C. Tracheoscopic image during catheterization. 3D. Tracheoscopic image 5 days after catheterization (carina) showed a fewer granulation tissues.
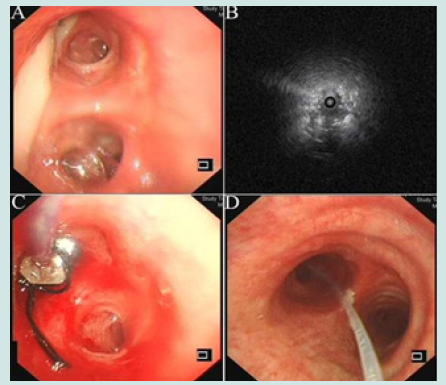
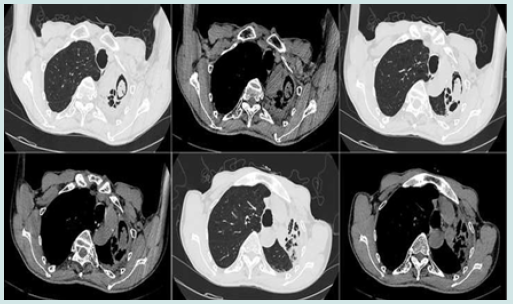
However, he developed fever after endobronchial instillation of amphotericin B, was given appropriate antipyretics, and granulation tissue proliferated 5 days after catheter placement (Figure 3D) without other significant systemic or additional complications. After 1 month of follow-up, a CT scan showed vacuolation of the left upper lobe lesion, forming an air moon sign (Figure 4), and the necrotic area had been resorbed. In addition, the patient’s haemoptysis had stopped and he recovered well. After discharge, the patient decided to stop taking oral voriconazole on his own after one month. To date, the patient is in good health with no clinical recurrence.
Figure 4: Follow-up CT image showed lesion of left upper lobe undergo cavitation and formation of the air crescent sign.
Discussion
CPA is a more serious fungal infectious disease of the lung with a high mortality rate, which is difficult to diagnose and treat [8]. The vast majority of patients with pulmonary aspergillosis are unlikely to be cured, so treatment aims to alleviate symptoms, stabilise the disease, prevent deterioration and reduce haemoptysis and fibrosis [8,9]. Oral itraconazole or voriconazole is used as the primary treatment for CPA [10] and alternative treatments include amphotericin B liposomes, isavuconazole or amphotericin B other lipid preparations [11]. Surgery is the optimal choice for some patients with CPA, but the patient was an elderly with poor lung function and chest wall adhesion. The efficacy of voriconazole was poor after one month of oral administration. Yoshii, et al. [12] reported that using liposomal amphotericin B successfully treated for invasive pulmonary aspergillosis caused by aspergillus terreus diagnosed under virtual bronchoscopic navigation and endobronchial ultrasonography with guide sheath. Parikh, et al. [13] reported EBUS-guided transbronchial needle injection of liposomal amphotericin B for the treatment of symptomatic aspergilloma. Herein, we gave to local infusion of amphotericin B using R-EBUS-guided new drug delivery device implantation, and achieved very good results.
Local infusion of amphotericin B can achieve higher drug concentrations in lung tissue, while avoiding various adverse reactions caused by systemic administration [14]. R-EBUS is a suitable solution for precisely locating the lung lesion and the bronchi connected to it, as well as for precisely planning the bronchoscope entry route. Previous methods of local administration include direct intraluminal administration through percutaneous thoracic needle or catheter placement and endobronchial instillation of antifungal medication [15,16]. The latter is more appropriate for lesions close to the central airway and cannot target peripheral lesions. In addition, repeated bronchoscopies increase pain, cost and operative risk for the patient.
We have designed a new type of anti-infective therapy device for localised pulmonary lesions that equipped with a drug catheter, a rubber stopper and a syringe. Direct exposure of drugs to lung lesions can more effectively deliver anti-infective effects. This device avoids repeated bronchoscopic operations. Secondly, it avoids drug reflux into the airway, retains the drug in the lesion for as long as possible and prolongs the duration of action, reducing the incidence of adverse reactions. The device has the advantages of simple structure, reduced cost, convenient operation and improved efficiency of medical staff.
At present, there is no clear standard for the dosage and duration of antifungal medication for treatment of pulmonary aspergillosis [16]. The initial dose of local infusion of amphotericin B for the treatment of chronic pulmonary aspergillosis is 5-10 mg and the maintenance dose is 15-20 mg according to the guidelines [10]. Therefore, in this case, the disease was effectively controlled after the local infusion of the amphotericin B 5mg per day for 4 days. The successful treatment of this case can provide evidence to support the subsequent clinical application and promotion of this device.
Author Contributions
ZX was responsible for the organization and coordination of the case. MZZ was the attending physician. XPL, PW and GSW contributed to data collection. MZZ and DF were responsible for original draft preparation. All the authors contributed to the review and editing of the final manuscript.
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
Informed consent was obtained from the patient for publication of this case report and accompanying images.
References
- Sehgal IS, Dhooria S, Prasad KT, Muthu V, Aggarwal AN, et al. (2021) Anti-fungal agents in the treatment of chronic pulmonary aspergillosis: Systematic review and a network meta-analysis. Mycoses 64(9): 1053-1061.
- Chamilos G, Luna MA, Lewis RE, Bodey GP, Chemaly RF, et al. (2006) Invasive fungal infections in patients with hematologic malignancies in a tertiary care cancer center: an autopsy study over a 15-year period (1989-2003). 917: 986-989.
- Pagano L, Candoni A, Offidani M, Fianchi L, Martino B, et al. (2006) The epidemiology of fungal infections in patients with hematologic malignancies: the SEIFEM-2004 study. Haematologica 91(8): 1068-1075.
- Ledoux MP, Guffroy B, Nivoix Y, Simand C, Herbrecht R (2020) Invasive Pulmonary Aspergillosis. Semin Respir Crit Care Med 41(1): 80-98.
- Anantham D, Koh MS, Ernst A (2009) Endobronchial ultrasound. Respir Med 103(10): 1406-1414.
- Hargis JL, Bone RC, Stewart J, Rector NT, Hiller FC(1980) Intracavitary amphotereicin B in the treatment of symptomatic pulmonary aspergillomas. 68(3): 389-394.
- Kravitz JN, Berry MW, Schabel SI, Judson MA (2013) A modern series of percutaneous intracavitary instillation of amphotericin B for the treatment of severe hemoptysis from pulmonary aspergilloma. Chest 143(5): 1414-1421.
- Hayes GE, Novak-Frazer L (2016) Chronic Pulmonary Aspergillosis-Where Are We? and Where Are We Going?. J Fungi (Basel) 2(2): 18.
- Kanj A, Abdallah N, Soubani AO (2018) The spectrum of pulmonary aspergillosis. Respir Med. 141: 121-131.
- Denning DW, Cadranel J, Beigelman-Aubry C, Ader F, Chakrabarti A, et al. (2016) Chronic pulmonary aspergillosis: rationale and clinical guidelines for diagnosis and management. Eur Respir J 47(1): 45-68.
- Ullmann AJ, Aguado JM, Arikan-Akdagli S, Denning DW, Groll AH, Lagrou K et al. (2018) Diagnosis and management of Aspergillus diseases: executive summary of the 2017 ESCMID-ECMM-ERS guideline. Clin Microbiol Infect 24(Suppl 1): e1-e38.
- Yoshii N, Yamada K, Niki M, Imoto W, Yamairi K, et al. (2021) Invasive pulmonary aspergillosis caused by Aspergillus terreus diagnosed using virtual bronchoscopic navigation and endobronchial ultrasonography with guide sheath and successfully treated with liposomal amphotericin B. Infection 49(5): 1049-1054.
- Parikh MS, Seeley E, Nguyen-Tran E, Krishna G (2017) Endobronchial Ultrasound-guided Transbronchial Needle Injection of Liposomal Amphotericin B for the Treatment of Symptomatic Aspergilloma. J Bronchology Interv Pulmonol 24(4): 330-333.
- Yi GWLPS (2012) Utility of topical use of amphotericin B in the treatment of fungal infections. Chinese Journal of Infection and Chemotherapy 12(5): 397-400.
- Lang M, Lang AL, Chauhan N, Gill A (2020) Non-surgical treatment options for pulmonary aspergilloma. Respir Med 164: 105903.
- FENG Jing WB, ZHANG Jing, LI Cai-li (2019) The theoretical basis and operational procedure of local instillation of amphotericin B into lungs by bronchoscopy. Tianjin Med J 47(4): 365-367.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




