Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Research Article(ISSN: 2637-4544) 
The Low Cost Intra-Uterine Balloon: An Innovative, Safe and Suitable Solution for Immediate Post-Partum Hemorrhagia (Hppi) By Uterine Atonia in Countries with Limited Resources Volume 4 - Issue 3
MM Niang*, A Mbodji, F Samb, M Thiam, ED Sy and CT Cisse
- Department of Obstetrics and Gynecology Hospital Institute of Social Hygiene of Dakar (Senegal)
Received:August 4, 2021Published: August 17, 2021
Corresponding author:Pr Mouhamadou Mansour NIANG, Associate Professor, Cheikh Anta Diop University of Dakar.
DOI: 10.32474/IGWHC.2021.04.000196
Abstract
Objectives: To assess the efficacy and safety of the low-cost intrauterine balloon in the management of immediate postpartum hemorrhage from uterine atony persisting after medical treatment.
Material and methods: This was a multicenter, prospective and descriptive study carried out between March 1, 2014 and August 31, 2016 (30 months) and concerning patients who presented an immediate postpartum hemorrhage by uterine atony and taken in load by the intrauterine balloon.
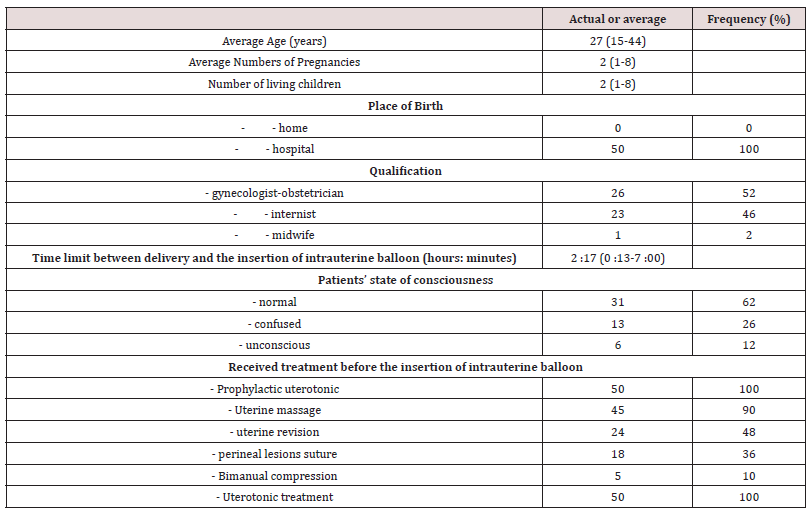
Results: Fifty patients met our inclusion criteria. They were on average 27 years old with an average parity of 2 and an average number of living children of 2. The intrauterine balloon was placed within an average of 2 hours 17 minutes after childbirth and removed in average 13 hours 58 minutes later. At the time of balloon insertion, 15 patients were in cardiovascular collapse, 13 of them with altered consciousness. Uterotonics were used for prophylaxis in all patients. The other therapeutic procedures performed before placing the intrauterine balloon were uterine massage (45/50), uterine revision (24/50), sutures of perineal lesions (18/50), bimanual compression (5 / 50) and the use of misoprostol (50/50). After insertion of the intrauterine balloon, 28 out of 50 patients (56%) received a blood transfusion. We had 90% success with stopping the bleeding and performed 4 hemostatic hysterectomies (8%). One case of acute anuric renal failure was noted and two maternal deaths recorded, for a case fatality of 2%. Conclusion: The intrauterine balloon appears to be an effective, safe and accessible means for the management of immediate postpartum hemorrhage from uterine atony in resource-limited settings.
Keywords: Maternal mortality; postpartum hemorrhage; uterine atony; intrauterine balloon
Introduction
Immediate postpartum hemorrhage (IPPH) is the leading cause of maternal mortality and morbidity in developing countries, with nearly 130,000 deaths each year and 2.6 million complications worldwide [1-3]. In Senegal, according to an assessment of emergency obstetric and neonatal care carried out between July 2012 and June 2013, the maternal mortality ratio was 222.9 per 100,000 live births, and haemorrhage was a direct cause of maternal death in 44,2% (SONU survey). In our limited resources countries, particularly in Senegal, available therapeutic means are: uterotonics (oxytocin, misoprostol), conservative surgery (triple arterial ligation, uterine artery ligation, hypogastric artery ligation, B- Lynch and Cho) and hysterectomy of hemostasis. These surgical treatments are not feasible by all health providers and are not available at the peripheral level (non-surgical health center, health post and health hut) where the majority of deliveries take place. Then, it is necessary to promote other therapeutic means better suited to our realities. To do this, the World Health Organization (WHO) recommends the use of the intra-uterine balloon as a second-line treatment for postpartum haemorrhage by uterine atony after failure of medical treatment and before resorting to surgery. However, due to their high cost, these devices are not accessible to developing countries. Over the past 5 years, a team at the Massachusetts General Hospital in the United States has designed and implemented a low-cost balloon (less than USD 5 or 3000 XOF) composing by two condoms, a catheter 24 gauge with an anti-reflux system, a 60 ml syringe and two small woolen threads. In collaboration with them, since March 2014, we have initiated a multicenter national study to evaluate the efficacy and safety of the low-cost intra-uterine balloon in the management of immediate postpartum hemorrhage by persistent uterine atony after medical treatment.
Patients and methods
Identification of study sites
Health structures had to meet the following criteria:
a) Be equipped with a maternity level 2 or 3 with a functional operating room,
b) Have a protocol for the management of HPPI that did not previously include the intra-uterine balloon,
c) Express an interest in the use of the intra-uterine balloon,
d) Identify a focal point for the structure that will participate in the training of trainers and be responsible for upgrading the rest of the medical staff and midwives and collecting data, be located in the regional capital.
Thirteen (13) health structures had met the above criteria and were selected: the regional hospitals of Thiès, Ziguinchor, Kaolack, Saint Louis, Youssou Mbargane Diop hospital in Rufisque, Grand Yoff General Hospital, Nabil Choucair Health Center, Philippe Maguilène Senghor Health Center, Abass Ndao Hospital, Ouakam Military Hospital, Pikine Hospital, Roi Baudouin Hospital in Guédiawaye and Principal Hospital in Dakar.
Training providers for the use of the intra-uterine balloon In order to accompany the introduction and the implementation of the intra-uterine balloon in Senegal, a four-hour practical training session for trainers was organized in March 2014 in collaboration with the team Of the General Hospital of Massachusetts. For each health center selected, an obstetric gynecologist and two midwives were trained. They were asked to use the intra-uterine balloon for the management of IPPH by uterine atony after failure of the preventive measures (active management of the third stage of delivery: AMTSL) and the medical treatment in force at Senegal (bladder sampling, uterine massage, sutures of perineal or cervical lesions, administration of uterotonics, artificial delivery and uterine revision) and prior to surgery. At the end of the training, 60 kits of intra-uterine balloon were distributed at a rate of 5 per health centers. Each kit contains two condoms, a 24-gauge catheter with an anti-reflux system, a 60 ml syringe, two small woolen threads, an illustrated checklist and a data collection sheet [Figure 1]. The condom is attached to the end of the catheter by the two small threads and the catheter-condom assembly, guided by the index and the medius, is introduced into the uterine cavity. Using the syringe, the balloon is filled with clean water. On average 300 to 500 ml are sufficient. If the hemorrhage stops, the balloon is left in place for 6 to 24 hours, on average 8 hours. A prophylactic dose of a broad-spectrum antibiotic (amoxicillin-clavulanic acid at 1g every 8 hours over 48 hours) and analgesic treatment (paracetamol perfusion at 1g every 12 hours until the balloon’s withdrawal) were recommended. When the patient is hemodynamically stable, the balloon is deflated with the syringe and removed from the uterine cavity while at the same time waiting for a resumption of bleeding. If bleeding resumes, the balloon is inflated again and left in place for 36 hours.
Figure 1: Components of the intrauterine balloon kit: two condoms, a 24-gauge catheter with an anti-reflux system, a 60 ml syringe, two small woolen threads, an illustrated checklist and a safety card data collection. Source: Division of Health and Human Rights, Department of Emergency Medicine, Massachusetts General Hospital, Boston, MA, USA.

Patient’s selection criteria
The study involved patients with immediate postpartum haemorrhage due to uterine atony, which persisted despite medical treatment in Senegal. The criteria for non-inclusion were allergy to latex and IPPH caused by other than uterine atony.
Data gathering
It was made using a data collection sheet containing the following items: the kit’s follow-up number, the name of the health structure, the age, the parity and the number of live children of the patient , The date and time of delivery, the treatment received before and after the use of the balloon, the patient’s state of consciousness at the time of balloon insertion, the need for maternal resuscitation, transfusion or hysterectomy of hemostasis, the efficacy and safety of the intra-uterine balloon and the patient’s outcome. The plug was filled immediately after the use of the intra-uterine balloon and sent as soon as possible to the study coordinator. The latter gives to the focal point of the health structure another kit to replace the one that has been already used.
Data analysis
A descriptive analysis was performed using Microsoft Excel 2007, Seattle, WA, USA and the Lexica Sphinx V5 Edition software.
It focused on the following parameters:
- characteristics of patients,
- delays of insertion and withdrawal of the intra-uterine balloon,
- difficulties encountered and the complications associated with its use,
- rate of blood transfusion and hysterectomy of hemostasis,
- maternal mortality rate and detailed analysis of deaths.
Results
Training of health providers
At the end of the training session, 36 health providers were competent to use the intra-uterine balloon in the management of IPPH by uterine atony. Twelve gynecologists-obstetricians and 24 midwives from 12 health structures (level 2 or 3 hospitals) were chosen to participate in the study. Between March 2014 and August 2016, the intra-uterine balloon was used at least once in 10 of the 13 health structures. A total of 50 intra-uterine balloon kits were used and distributed as follows in decreasing order:
- Pikine hospital (13/50),
- Health center Nabil Choucair (9/50),
- Thiès regional hospital (7/50),
- Ouakam military hospital (5/50)
- Ziguinchor Regional Hospital (4/50),
- Saint Louis Regional Hospital (3/50)
- Kaolack regional hospital (3/50),
- Youssou Mbargane Diop Hospital of Rufisque (2/50),
- General Hospital of Grand Yoff (2/50),
- Roi Baudouin hospital of Guédiawaye (1/50),
Among the 50 uses of intra-uterine balloon, we registered 45 successes (90%).
Characteristics of Patients
Patients were aged between 15 and 44 years with an average of 27 years. The most represented group was 32 years and over. Parity ranged from 1 to 8 with an average of 2. The number of live children averaged 2. All patients had delivered in a health structure that was a health center in the majority of cases (34%). The balloon was inserted by an obstetrician in 26 cases (52%), only one balloon was performed by a midwife. Before to balloon insertion, the patients had the following interventions: uterotonic prophylaxis (100%), uterine massage (45/50, 90%), uterine revision (45/50, 90%), sutures of perineal lesions (18/50, 36%), bimanual compression (5/50, 10%), uterotonic treatment (43/50, 86%). At the time of balloon insertion, 31 patients (62%) had clear consciousness, 13 (26%) were confused and 6 (12%) were unconscious. Hemodynamically, there were 15 cases of cardiovascular collapse (30%) [Table 1].
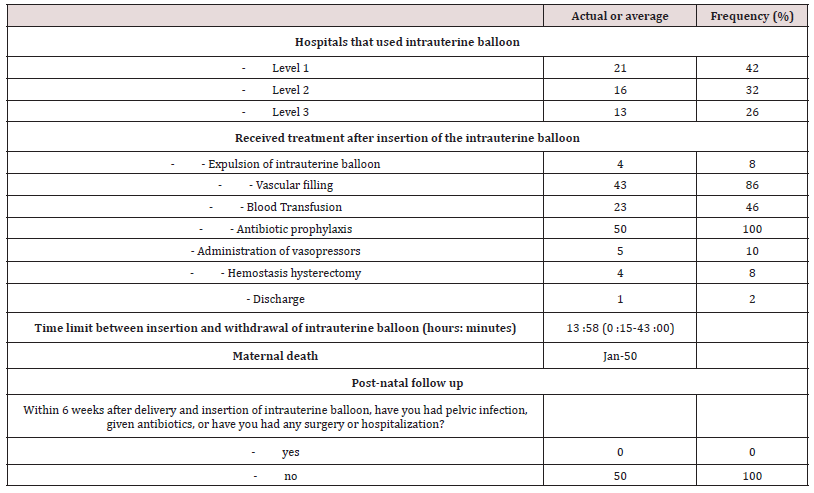
Management of intra-uterine balloon haemorrhage
The intra-uterine balloon was used in 16 cases (32%) at level 2 maternity. The delay between delivery and insertion of the intra-uterine balloon was between 13 minutes and 07 hours with an average 2 hours 16 minutes. After the intra-uterine balloon’s insertion, 45 patients (90%) stopped bleeding and a failure occurred in 5 cases (10%). In case of failure, we noticed in 3 cases that the bleeding immediately stopped, then restarted within a median time of 60 minutes; for the other two cases, there was a persistence of haemorrhage after intrauterine tamponade due to a malposition of the balloon for one patient. For those patients for whom the intrauterine balloon was found to be ineffective, in the management of delivery hemorrhage, 4 had had a hysterectomy of hemostasis (9.8%) and one patient had died (2.4%). In our study, the insertionwithdrawal time of the intra-uterine balloon varied between 15 minutes and 43 hours with an average of 13 hours 58 minutes. In the 6 weeks following the delivery and insertion of the intra-uterine balloon, no patient had an infection. The discharged patients were systematically on a curative dose of iron over 3 months. Antibiotic prophylaxis was also recommended for a minimum of 7 days [Table 2].
Table 2: Data on the management of immediate postpartum hemorrhage by the intrauterine balloon (N = 50).
Discussion
The principle of the tamponade to stop bleeding results from a play of pressure: the application of an extravascular pressure superior to the intravascular pressure in a prolonged way makes possible to seal the vessels and interrupts the bleeding [4]. Bakri was the first to mention it in the treatment of haemorrhages secondary to a placenta praevia or accreta during a caesarean section [5] by the use of several Foley probes inserted together in the uterine cavity. The main restriction to the use of the Foley probe was its filling volume limited to 150 mL [4]. We chose the balloon described above which has a greater capacity than the Foley probe and whose cost is more accessible for our limited resource countries. In our study, 50 immediate postpartum hemorrhage (IPPH) due to uterine atony were handled with the low-cost intra-uterine balloon. Despite the precarious hemodynamic status of the patients (15 cases of cardiovascular collapse including 13 with consciousness disorders) reflecting the severity of the IPPH, this treatment stopped bleeding 45 times out of 50 (90%). These results are encouraging and show the efficacy of the intra-uterine balloon in the management of IPPH. Several authors have reported results similar to ours [4- 8]. Indeed, in the Condous series of 16 patients with persistent bleeding, Sengstaken-Blakemore catheterization was effective in 14 of them, only 2 patients required a surgical procedure because of a placenta Praevia [7]. The main advantage of the balloon presented in the study is its cost (5 USD) which is far cheaper (40 times) than the Sengstaken-Blakemore probe (220 USD) for an equivalent efficiency. However, we performed four hysterectomies of haemostasis (%). One of them followed two unsuccessful attempts to use the balloon. The device was low located in the uterine cavity and As soon as it was filled it was externalized to find itself in the vagina. This was obviously a technical problem, showing the real need of training in balloon use. Therefore, in collaboration with the Ministry of Health and Social Action of Senegal, our objective should be to empower all providers who practice childbirth at all levels of the health pyramid for the use of this tool. Only one patient was evacuated after the insertion of the intrauterine balloon It was due to an acute renal anuric insufficiency. It has well evolved with a normalization of the renal function after a stay in intensive care and sessions of hemodialysis. This low rate of evacuation after use of the balloon (3.3%) makes us think that it is a therapeutic mean adapted to the remote and under medicalized areas of the country. Indeed, it could help to reduce the rate of evacuation of these peripheral structures which often, after the failure of the medical treatment, send patients to the higher-level structure where the surgery can be performed. In our study, the lethality was 2.4%; it was lower than the 2013 SONU survey’s result which was 4.1% for the lethality due to postpartum hemorrhage [9]. In several studies about the intra-uterine tamponade balloon, the lethality was zero; but it was a study with a small number of patients that did not allow the real assessment of lethality when intrauterine tamponade was introduced as a second line treatment in case of IPPH by uterine atony [10-13]. These lethality and morbidity rates in our serie reflect the efficacy and safety of the intra-uterine balloon when used by trained practicians. Also, there were no cases of endometritis. This is a reflection of the innocuousness of the intra-uterine balloon when used in combination with effective antibiotic prophylaxis. Almost all intra-uterine balloon (98%) were performed by medical staff (residents and gynecologist-obstetricians), and one (2%) by a midwife from a regional hospital. This was a limit in our study but could be explained by the fact that our study was carried out in reference hospitals where care is provided 24 hours a day by a resident or an obstetric gynecologist. However, this practice should be extended to midwives who perform the majority of deliveries and who generally practice in peripheral areas where surgery is often unavailable. In the Burke et al. study, 53% of intra-uterine balloon insertions were performed by midwives and the overall success rate was 95% [14]. This proves the feasibility of intrauterine balloon insertion by midwives.
Conclusion
The low-cost intra-uterine balloon is an affordable, effective, and safe method for the management of persistent IPPH after medical treatment in limited resource countries such as Senegal. However, a larger scale study including all health providers (gynecologist-obstetricians, residents, and midwives) and all levels of the health pyramid would be necessary to assess the feasibility of this intervention throughout the Senegalese territory.
References
- WHO Recommendations for the Prevention and Treatment of Postpartum Haemorrhage (2012) WHO Guidelines Approved by the Guidelines Review Committee. Geneva: WHO.
- FIGO Safe Motherhood and Newborn Health Committee (2012) FIGO guidelines: prevention and treatment of postpartum hemorrhage in low-resource settings. International Journal of Gynecology & Obstetrics 117: 108-118.
- The Royal College of Obstetricians and Gynecologists (2009) RCOG Green-Top Guideline 52 The Royal College of Obstetricians and Gynecologists. Prevention and management of postpartum hemorrhage.
- A Florian, G Carles, F Dallah, N Ibrahim, N Alassas, et al. (2013) Intérêt de la sonde de Linton-Nachlas dans la prise en charge des hémorragies du post-partum: une série de 25 cas. Journal of Obstetrics and Reproductive Biology 42(5): 493-498.
- Cho HY, Park YW, Kim YH, Jung I, Kwon JY (2015) Efficacy of intra uterine Bakri Balloon Tamponade in Cesarean Section for placenta previa patients. PLOS ONE 10(8): e0134282.
- Laas E, Bui C, Popowski T, Mbaku O M, Rozenberg P (2012) Trends in the rate of invasive procedures after the addition of the intrauterine tamponade test to a protocol for management of severe postpartum hemorrhage. American Journal of Obstetrics & Gynecology 207(4): 281.e1-287.e7.
- Grönvall M, Tikkanen M, Tallberg E, Paavonen J, Stefanovic V (2013) Use of Bakri balloon tamponade in the treatment of postpartum hemorrhage: a series of 50 cases from a tertiary teaching hospital. Acta Obstetricia et Gynecologica Scandinavica 92(4): 433-438.
- Martin E, Legendre G, Bouet P E, Cheve M T, Multon O, et al. (2015) Maternal outcomes after uterine balloon tamponade for postpartum hemorrhage. Acta Obstetricia et Gynecologica Scandinavica.
- Ministère de la Santé et de l'Action Sociale. Rapport d'évaluation des SONU au Sénégal (2012-2013). MSAS – UNFPA – OMS – UNICEF – CEFOREP 2014: 135.
- Alouini S, Bedouet L, Ramos A, Ceccaldi C, Evrard ML, et al. (2015) Évaluation du ballon de Bakri dans les hémorragies graves du post-partum et fertilité ulté Journal de Gynécologie Obstétrique et Biologie de la Reproduction 44(2): 171-175.
- Makosso M, Koné AB, Rossignol M, Bénos P, De Tayrac R, et al. (2015) Le méchage intra-utérin: utilité et place dans la prise en charge de l’hémorragie du post-partum immé À propos de 99 cas. L’expérience d’un centre hospitalier français de niveau 2 A. Journal de Gynécologie Obstétrique et Biologie de la Reproduction 44(1): 53-62.
- Raynal P. Le ballonnet de Bakri (2011) Gynécologie Obstétrique & Fertilité 39(7-8): 438-441.
- Nelson WL, O’Brien JM 2007 The uterine sandwich for persistent uterine atony: combining the B-Lynch compression suture and an intrauterine Bakri balloon. Am J Obstet Gynecol 196(5): e9-e10.
- TF Burke, R Ahn, BD Nelson, R Hines, J Kamara, et al. (2015) A postpartum haemorrhage package with condom uterine balloon tamponade: a prospective multicentre case series in Kenya, Sierra Leone, Senegal, and Nepal. BJOG 123(9): 1532-1540.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...