
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Research Article(ISSN: 2637-4544) 
Social Support of Pregnant Immigrants with Psychosocial Risk Volume 4 - Issue 3
Antonia Vollrath1*, Amelia S Figueiredo2, Estela Arcos3 and Antonia Arrate4
- 1School of Nursing, Faculty of Sciences, Universidad Mayor de Chile
- 2Institute of Health Sciences, School of Nursing, Universidade Católica Portuguesa, Lisbon, Portugal
- 3External Researcher of the CSOC 10 18-19 Project Sponsored by the Universidad Playa Ancha, Chile
- 4Faculty of Medicine, University of Chile
Received: May 13, 2021Published: May 27, 2021
Corresponding author: Antonia Vollrath, Associate Professor, Postdoctoral Portuguese Catholic University. School of Nursing, Faculty of Sciences, Universidad Mayor de Chile
DOI: 10.32474/IGWHC.2021.04.000194
Introduction
Background: Social support structure helps women facing migration processes to integrate and adapt to society, especially in unforeseen circumstances. To know the social support of pregnant immigrants with social risk. Descriptive cross-sectional study. A social survey was conducted prior to the signing of the informed consent.
Methods: Through the self-report, women identified primary and secondary relationships.
Results: Of the 37 immigrant women and their partners, the majority come from Latin American countries, especially Peru (62.2%), with ages between 20 and 34 years (64.9%), unmarried civil status (32.4%), head of household (27%) and the type of single-parent family (29.7%) are determinants of social risk for pregnant women, especially if they do not have social support. 75% of women had an unplanned pregnancy and one in two had depression.
Conclusions: The available social support network was reduced to the family network and the health center. The interactions that occur with the social network contribute to the well-being and self-esteem of the person, aspects that should be considered in prenatal care, because of the implications it has for the health of the woman and child.
Pregnancy is an incomparable event in a woman’s life, involving deep physical, physiological, and emotional changes, constituting, in adverse contexts, a state of stress during pregnancy and postpartum [1]. For this reason, the role of the social network such as couples, family, friends and health professionals, which can be the most significant source of social support for pregnant women, is fundamental [1]. It has been reported that having social support during the postpartum stage can reduce the risk of depression; also, good relationships with the couple have a protective “buffer” effect against those determinants that cause stress during pregnancy and postnatal stage thus decreasing the risk of depression [2-4]. According to a study in which emotional, instrumental and informational social support was provided during the third trimester of pregnancy and during the postpartum period, the results showed an average life satisfaction value of 24.52% in the third trimester of pregnancy, with 25,71% in the postpartum period [2]. In the case of women carrying out migratory processes, the existence of a social support structure favors the ability to adapt and integrate into society, such as being in contact with neighbors, having friends, acquaintances in the neighborhood and belonging to social groups [5] According to a study conducted in Spain, on the social support network of family members, friends and associations of Latin American, African and Eastern European immigrants, 2.2% reported having none of these networks, 23.3% reported having only the family and 37,3% reported having family and friends. A 37.2% reported having relatives, friends and members of the above-mentioned associations [5]. Another study reported a 32.0% estimated prevalence of prenatal depression and a 26% of probable postpartum depression using the Edinburgh Postnatal Depression Scale (EPDS) of ≥13. They investigated complex life circumstances, 26% were prone to develop depressive symptoms after birth, high levels of stress in life, general ill health, low social support and difficulty caring for their babies were observed [6].
In Portugal it has been observed that immigrant mothers have a higher risk of postpartum depression and less satisfaction with the social support received, the results revealed a higher risk of postpartum depression (OR = 6.118; IC del 95%: 1.991-18.798), p< 0,05 [7].n (OR = 6.444; IC of 95%: 1.858-22.344) and low satisfaction with social support (OR = 6.118; IC of 95%: 1.991- 18.798), p< 0,05 [7]. In addition, migrant women in situations of social vulnerability during pregnancy and childbirth face barriers to access to health services due to the lack of health insurance and the lack of financial resources to pay for services, or, failing to understand the administrative formalities to be carried out [8, 9]. Unfavorable socio-economic status appears to influence the quality of health care, associated with a lack of cultural sensitivity of health professionals, leading to non-use of health services [10]. In Chile, immigrant women have the right to receive health care during pregnancy and child-rearing periods, through the Comprehensive Child Protection System “Chile Crece Contigo (SChCC),” which aims to provide social support to populations of families in a situation of social vulnerability [11,12]. Given the background described the need to generate background on support networks in pregnant immigrant women was raised with the following research question, what are the support networks that immigrant pregnant women with psychosocial risk, who are served in centers of the public primary health network of an urban community in Santiago of Chile, have? allowing us to learn about psychosocial risk and support networks available to study participants.
Materials and Methods
A descriptive cross-sectional study was conducted in a universe of 37 immigrant pregnant women with psychosocial risk who entered the prenatal check-up from October 2015 to February 2016 in two primary health centers in the Santiago of Chile. Since we worked with the total universe, no samples were used. The technique used was the social survey. The primary information was obtained through the application of a structured interview that allowed obtaining the following antecedens of the woman, her family and her partner: psychosocial, mental health and obstetric, and institutional support. The interview was conducted by two female researchers in the health centers, after the voluntary signing of the informed consent certificate. Secondary information was obtained from the consultation of the conventional electronic clinical records of the health centers, this information was collected by a female investigator on the screening tests applied during the prenatal control, the history of childbirth and newbor, and the benefits received. The evaluation of the interviewed women, regarding to the perception of the size, structure, type and quality of the primary and secondary social network, was evaluated with an instrument that represents an ecomap. This instrument contained a set of symbolic figures that represented the relationships with networks of primary and secondary type and quality, which were identified with a traffic light-like drawing, which contained the four categories of the interviewee’s perception in relation to each of the social networks: bad, regular, good and no relation In this way each interviewee reported autonomously the type of relationship she had with each recognized social support network. The critical analysis and processing of the data was supported by the computational program S.P.S.S. Descriptive, position and dispersion statisticians according to the type of variable were calculated. Rates and ratios were calculated the comparison of proportions was made through the chi-square test.
Results
Table 1: Background of 37 immigrant pregnant women with psychosocial risk under the Chile Crece Contigo program, Santiago of Chile, 2015-2016.
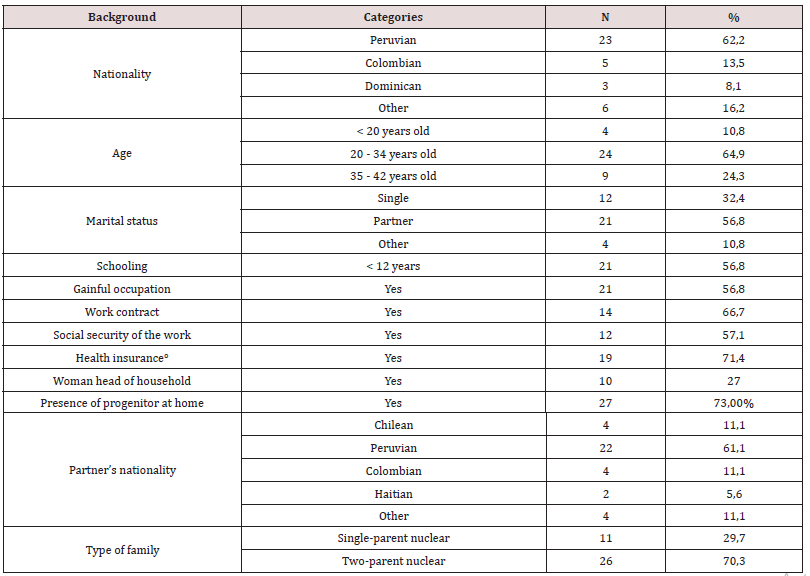
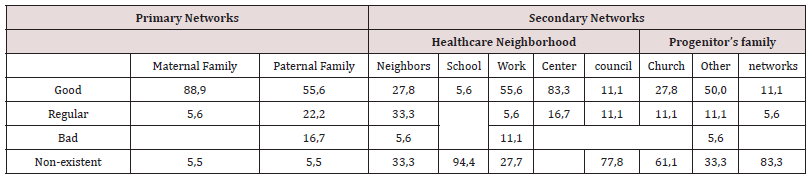
Of the 37 immigrant women and their partners, the majority come from Latin American countries, especially Peru (62.2%), with ages between 20 and 34 years (64.9%). However, the group of women who became pregnant between the ages of 35 and 42 (24,3%) should be highlighted because it defines a risk condition for reproductive and neonatal health. Also, unmarried civil status (32.4%), head of household (27%) and the type of single-parent family (29.7%) are determinants of social risk for pregnant women, especially if they do not have social support. One in two women had incomplete schooling and paid employment and, of those who worked, only two out of three had a contract of employment and social security. In 1 out of 4 households, the father was not present [Table 1]. With regard to reproductive health records, 75% of women reported unplanned pregnancies, most of them were multiparous with admission after 12 weeks of pregnancy to the prenatal check-up, and had a prevalence of depression in 54,3%, which was detected by the application of the Edinburgh Scale [Table 2]. These events marked a condition of high risk for women in their mental and reproductive heath, and child health. With regard to the most significant psychosocial risks identified, in psychosocial tests carried out at the first prenatal check-up of 37 immigrant women, it was revealed that 36% had depressive symptoms, regarding the time of admission to prenatal care 26% did it after 20 weeks of gestation and is striking that 12% reported rejection to pregnancy. In women with depression, it was observed that depressive symptoms and rejection to pregnancy were the most important (64.7%) Regarding the quality of the primary social support network, women reported a low average of interaction with neighborhood councils and schools, however, with the maternal and paternal family reported good quality interaction. In the secondary networks, it is noteworthy that the health center was mostly recognized as good quality social support, followed by the relationship with the work network and the family of their partner [Table 3]. A similar behavior was found in the social support network in women with depression [Table 4].
Table 2: Obstetric and psychosocial history of 37 immigrant pregnant women with psychosocial risk under the Chile Crece Contigo program, Santiago of Chile, 2015-2016.
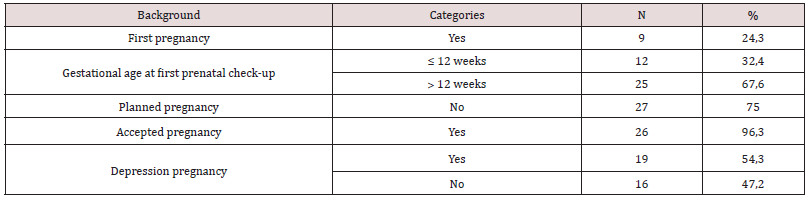
Table 3: Quality of the primary and secondary social support network of 37 immigrant women at psycosocial risk.
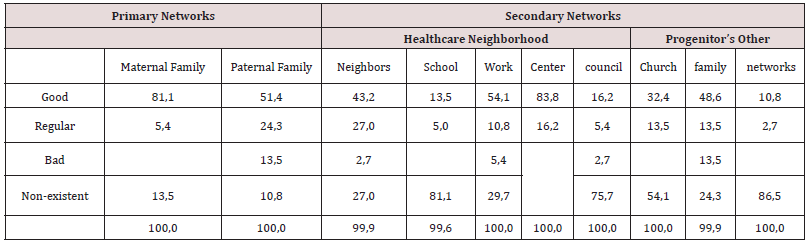
Table 4: Quality of the primary and secondary social support network of 37 immigrant women at psycosocial risk and depresion.
Discussion
Findings demonstrate that immigrant women’s reproductive health is exposed to a high rate of unplanned pregnancies, pregnancy rejection and late prenatal care admission, which is worse when the women are depressed. The ambivalence of identity development in some migrant populations may accommodate the social role of motherhood in women, coupled with difficulties of access and limited information on fertility regulation methods, increasing the likelihood of unplanned pregnancy [13-15]. On the other hand, late care is more frequent in unplanned pregnancies, this situation leads to an increase in the percentages of abortion, constituting a public health problem especially in countries where it is not legalized, resulting in an increase in morbidity and mortality related to clandestine abortions [16]. Appart from all the above mentioned, it has to be added the difficulties of care centers in meeting the needs of immigrant women in the area of family planning [17,18]. In terms of timely access to health care for early detection of pregnancy, this is crucial for women who did not plan a pregnancy because it has been observed that they recognize the pregnancy two weeks later than women with desired pregnancies. Early prenatal care can prevent the adoption of behaviors that promote reproductive health, especially among women with unwanted pregnancies. The negative effect of harmful behavior on health, such as drinking and smoking during the embryonic stage, results in most malformations [19]. This work revealed that immigrant women had an unplanned pregnancy coupled with depression, evidence indicates that such health conditions increase health care costs for them, identifying, sometimes, personal and family crises that may affect the results of the child’s upbringing and development [20,21]. As a result, being an immigrant, may generate a greater predisposition to develop depression both prenatal and postnatal. In addition, children born from unplanned pregnancies have lower birth weight and lower cognitive performance [22]. In the United States, reported maternal mortality and morbidity is highest among women from migrant groups, despite advances in prenatal care. There has also been an increase in the age of pregnancy and high infant mortality rates, mainly associated with prematurity, it should be noted that in Japan infant and stillbirth mortality rates are higher in immigrant women than in native women [23, 24]. On the other hand, the rates of chronic diseases such as obesity, hypertension, diabetes, use of illicit substances and congenital malformations have increased in these populations [24]. The fact that one in two pregnant immigrant women has depression represents the consequences of facing an unforeseen situation and in a context of social vulnerability. It has been pointed out that the impact of migration on pregnant women generates in the psychological area feelings of insecurity, isolation, discomfort in the circle of more intimate relationships and nostalgia for their culture and family [25-27].
In addition, low incomes with poor security conditions, low schooling and barriers to access to health care predispose women to a profound deterioration in mental health [25,27]. Another of the findings of this study showed the quality of social support networks. The primary network is the family and is essentially focused on the maternal family that remains in the country of origin of the women. According to studies carried out on social support for immigrant women, they corroborate the findings obtained about the support networks that are mainly concentrated in the primary network such as the family of origin, in most cases [28]. In relation to the secondary network is focused on the health center, family of the partner. It is relevant to mention that the revised literature indicates that pregnant immigrant women face high levels of stress in life and have poor social support and are therefore more likely to develop postnatal depression, anxiety, somatization and posttraumatic stress disorder than pregnant women with adequate and relevant social support [6,29]. Regarding social support networks, they are essential to counteract the social isolation because they provide the help, care and emotional support that immigrant women need in this process [10], which must be increased during pregnancy and postpartum. Also, having support networks of family, friends or other types such as care networks provides tools that reduce social isolation and facilitate integration into the host country [30]. The information provided has given rise to concern about showing the vulnerability of immigrant women in primary public health care. It is necessary to consider and incorporate in public policies strategies for survival and adaptation to the new contexts developed by the immigrant population, which must be based on the strengthening of their social networks and their interaction dynamics because it provides them with adaptive and integrative coping strategies [5,31]. It is essential to consider that motherhood in immigrant women has various difficulties, which requires the support of a cultural, social and health structure that provides care with a holistic and interdisciplinary approach [32]. The interactions that occur with each component of the social network contribute to personal well-being and self-esteem, aspects that have health implications, since social support is associated with life events, disease, mortality and health promotion [5]. The respect and dignity for the human, must be is the primary concern in the attention of health [33,34].
Conclusion
Confirming the conclusions of our research on the quality of social support in pregnant immigrant women with psychosocial risk, attended in public health centers in an urban community of Santiago de Chile, the support networks are essentially centered on the maternal and paternal nucleus and health-care centers. Based on studies carried out, we can affirm that one of the most relevant components in the above-mentioned topic is related to the health care provided by health professionals, mainly midwives and nurses who are responsible for the health care of this population during a long period of time, therefore the challenge is to provide care with a comprehensive approach and cultural sensitivity, in order to respond to the real needs of pregnant immigrant women, avoiding further harm to both the mother, child and family. Therefore, we can affirm that having a structure of social support networks contributes to well-being, quality of life and mental health especially in people facing migratory processes, these networks promote integration and adaptation to the host society, especially in unexpected circumstances. From a perspective of the contribution of these findings, they can be useful to promote comprehensive and crosscultural strategies and interventions in the population of pregnant immigrant women at psychosocial risk.
Funding
This work was supported by Dirección de Investigación, Universidad Andrés Bello de Chile [grant numbers DI-730-15/CB, 2015].
Disclosure statement
Disclosure statement
References
- Skurzak A, Kicia M, Wiktor K, Iwanowicz Palus G, Wiktor H (2015) Social support for pregnant women. Polish Journal of Public Health 125(3): 169-172.
- Gebuza G, Kaźmierczak M, Mieczkowska E, Gierszewska M, Banaszkiewicz M (2016) Adequacy of social support and satisfaction with life during childbirth. Polish Annals of Medicine 23(2): 135-140.
- Kim T H M, Connolly J A, Tamim H (2014) The effect of social support around pregnancy on postpartum depression among Canadian teen mothers and adult mothers in the maternity experiences survey. BMC Pregnancy and Childbirth 14(1): 162.
- Rini C, Schetter C D, Hobel C J, Glynn L M, Sandman C A (2006) Effective social support: Antecedents and consequences of partner support during pregnancy. Personal Relationships 13(2): 207-229.
- Dominguez Fuentes J M, Hombrados Mendieta M I (2012) Social support and happiness in immigrant women in Spain. Psychol Rep 110(3): 977-990.
- Tsao Y, Creedy D K, Gamble J (2015) Emotional well-being of Vietnamese immigrant women during the transition to motherhood: A descriptive cohort study. Nurs Health Sci 17(1): 49-56.
- Almeida L M, Costa Santos C, Caldas J P, Dias S, Ayres de Campos D (2016) The impact of migration on women’s mental health in the postpartum period. Rev Saude Publica 50.
- Balaam M C, Akerjordet K, Lyberg A, Kaiser B, Schoening E, et al. (2013) A qualitative review of migrant women’s perceptions of their needs and experiences related to pregnancy and childbirth. J Adv Nurs 69(9): 1919-1930.
- Martinez O, Wu E, Sandfort T, Dodge B, Carballo Dieguez A, et al. (2015) Evaluating the impact of immigration policies on health status among undocumented immigrants: A systematic review. J Immigr Minor Health 17(3): 947-970.
- Santiago M C F, Figueiredo M H (2015) Immigrant women’s perspective on prenatal and postpartum care: Systematic review. J Immigr Minor Health 17(1): 276-284.
- Arcos E, Muñoz L A, Sanchez X, Vollrath A, Gazmuri P, et al. (2013) Effectiveness of the Comprehensive Childhood Protection System for vulnerable mothers and children. Rev Lat Am Enfermagem. 21(5): 1071-1079.
- Ministerio de Salud (MINSAL) (2014a) Oficio Ordinario N° Atención en salud de población inmigrante en riesgo social y situación de permanencia no regular [Health care for the immigrant population at social risk and a situation of irregular permanence]. 2008.
- Coelho EAC, Andrade MLS, Vitoriano LVT, Souza JJ, da Silva, et al. (2012) Association between unplanned pregnancy and the socioeconomic context of women in the area of family health. Acta Paul Enferm 25(3): 415-422.
- Ministerio de Salud (MINSAL) (2014b) Protocolo de detección de la depresión durante el embarazo y posparto, y apoyo al tratamiento [Depression detection protocol during pregnancy and postpartum, and treatment support].
- Quelopana AM, Alcalde C (2014) Exploring knowledge, belief and experiences in sexual and reproductive health in immigrant Hispanic women. J Immigr Minor Health 16(5): 1001-1006.
- Yanikkerem E, Ay S, Piro N (2013) Planned and unplanned pregnancy: Effects on health practice and depression during pregnancy. J Obstet Gynaecol Res 39(1): 180-187.
- Andrade FMR, Simões Figueiredo A, Capelas ML, Charepe Z, Deodato S (2020) Experiences of homeless families in parenthood: A systematic review and synthesis of qualitative evidence. Int J Environ Res Public Health 17(8): 2712
- Casillas A, Bodenmann P, Epiney M, Gétaz L, Irion O, et al. (2015). The border of reproductive control: Undocumented immigration as a risk factor for unintended pregnancy in Switzerland. J Immigr Minor Health 17(2): 527-534.
- Ayoola A B (2015) Late recognition of unintended pregnancies. Public Health Nurs 32(5): 462-470.
- Garner A S, Shonkoff J P (2012) Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Adoption, and Dependent Care, & Section on Developmental and Behavioral Pediatrics. (2012) Early childhood adversity, toxic stress, and the role of the pediatrician: Translating developmental science into lifelong health. Pediatrics 129(1): e224-e231.
- McKeating A, Crosby D A, Collins M, O’Higgins A, McMahon L, et al. (2015) A longitudinal study of unplanned pregnancy in a maternity hospital setting. Int J Gynaecol Obstet 128(2): 106-109.
- Wellings K, Jones K G, Mercer C H, Tanton C, Clifton S, et al. (2013) The prevalence of unplanned pregnancy and associated factors in Britain: Findings from the third National Survey of Sexual Attitudes and Lifestyles (Natsal-3). Lancet 382(9907): 1807-1816.
- Frayne D J, Verbiest S, Chelmow D, Clarke H, Dunlop A, et al. (2016) Health care system measures to advance preconception wellness: Consensus recommendations of the clinical workgroup of the National preconception health and health care initiative. Obstet Gynecol 127(5): 863-872.
- Kita S, Minatani M, Hikita N, Matsuzaki M, Shiraishi M, (2015) A systematic review of the physical, mental, social, and economic problems of immigrant women in the perinatal period in Japan. J Immigr Minor Health 17(6): 1863-1881.
- Dahlen H G, Barnett B, Kohlhoff J, Drum M E, Munoz A M, et al. (2015) Obstetric and psychosocial risk factors for Australian-born and non-Australian born women and associated pregnancy and birth outcomes: A population based cohort study. BMC Pregnancy and Childbirth 15: 292.
- Hashimoto H, Ito K, Yamaji Y, Sasaki Y, Murashima S, et al. (2011) Difficulties of pregnancy, delivery, and child raising for immigrant women in Japan and their strategies for overcoming them. Kokusai Hoken Iryo 26(4): 281-293.
- Rumbold A R, Bailie R S, Si D, Dowden M C, Kennedy C M (2011) Delivery of maternal health care in Indigenous primary care services: Baseline data for an ongoing quality improvement initiative. BMC Pregnancy and Childbirth 11(1): 16.
- Simões Figueiredo A, Ferrito C, Santos AS, Deodato S, Seabra P, et al. (2020) Family transitions to homelessness: A qualitative approach. Rev Bras Enferm 73(5): e20190554.
- Stewart D E, Gagnon A J, Merry L A, Dennis C L (2012) Risk factors and health profiles of recent migrant women who experienced violence associated with pregnancy. Journal of Women’s Health 21(10): 1100-1106.
- Cabrera M, Prieto R, Sanz A, Estepa L, Bahillo E (2016) Asociacionismo, capital social y apoyo mutuo en las mujeres migrantes. Una aproximación cualitativa [Social capital and mutual support among migrant women. A qualitative approach]. CIAIQ 2016 (3): 326-334.
- Araujo K (2016) La calle y las desigualdades interaccionales [The Street and interactional inequalities]. Serie documentos de trabajo PNUD- desigualdad No. 2016 [UNDP working document series - inequality].
- Arcos E, Vollrath A, Sánchez X, Bailey C (2018) Motherhood inmigrant women in Chile: A qualitative study. Midwifery 66: 182-186.
- Simões Figueiredo A, Seabra P, Sarreira Santos A, Vollrath A, Medeiros Garcia L, et al. (2019) Nursing consultation in a public bathhouse: A community resource for the vulnerable population in a European capital. Issues Ment Health Nurs 40(1): 28-32.
- Simões Figueiredo A, Rasquilho Vidal T, Ferrito C, Neves Amado J, Sarreira Santos A, et al. (2020). Community mental health nursing consultation in a public bathhouse: A spiritual coping resource. Religions, 11(11): 618.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...





