
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Mini Review(ISSN: 2637-4544) 
Role of Ultrasonography and Uterine Doppler Parameters to predict Endometrial Receptivity in Infertile Patients Volume 5 - Issue 3
Brinderjeet Kaur*
- Consultant, Dept of Obstetrics and Gynecology, Santokba Durlabhji Memorial Hospital & Research Centre, India
Received:May 09, 2022; Published: May 18, 2022
Corresponding author: Brinderjeet Kaur, Consultant, Dept of Obstetrics and Gynecology, Santokba Durlabhji Memorial Hospital & Research Centre, Jaipur, India
DOI: 10.32474/IGWHC.2022.05.000215
Abstract
Infertility is on increase with rising trend observed in carrier-oriented couples. The influence of infertility can be immense and devastating. The impact affects the social wellbeing with loss of self-esteem, disappointment and depression. The investigations of many such couples do not exhibit any perceptible cause and are labeled as ‘unexplained infertile’ - which accounts for around 15-30 percent of the cause of infertility. Such couples have normal ovulatory function, normal semen analysis, normal tubal patency and normal endometrial cavity. It is often hard to explain to such couples their inability to reproduce. The vital step in conception is the efficacious implantation which necessitates a normal and functioning embryo at developmental stage of blastocyst, a receptive endometrium and a synchrony between embryonic and maternal tissue. The article discusses the role of ultrasound and color Doppler compiled with Uterine Biophysical scores (UBP), Uterine Scoring System for Reproduction (USSR) as noninvasive tools to assess endometrial receptivity and pregnancy outcome.
Keywords: Infertility; Endometrial Receptivity; Uterine Biophysical Profile (Ubp); Uterine Scoring System for Reproduction (Ussr)
Introduction
Infertility is on increase with rising trend observed in carrieroriented couples [1]. However, the influence of infertility can be immense and devastating. The impact affects the social wellbeing with loss of self-esteem, disappointment and depression. The investigations of many such couples do not exhibit any perceptible cause and are labeled as ‘unexplained infertile’ [2] - which accounts for around 15-30 percent of the cause of infertility [3]. Such couples have normal ovulatory function, normal semen analysis, normal tubal patency, and normal endometrial cavity [4]. It is often hard to explain to such couples their inability to reproduce. The vital step in conception is the efficacious implantation which necessitates a normal and functioning embryo at developmental stage of blastocyst, a receptive endometrium, and a synchrony between embryonic and maternal tissue [5]. Implantation is an important step in establishing pregnancy and scientific basis of failure of implantation is still to be deciphered. Implantation is difficult to study because our knowledge of what happens during the first week of human life in vivo is limited. It requires decoding the interaction between a blastocyst and a receptive endometrium [6-8]. Numerous diagnostic parameters have been projected to estimate endometrial receptivity. These tools include histologic dating of an endometrial biopsy, endometrial cytokines in uterine flushing, or molecular expression of vasoactive compounds, the genomic study of a timed endometrial biopsy or more commonly a noninvasive ultrasound examination of endometrium with Colour Doppler –all relying on angiogenic factors helping in implantation. The recent approach is to visualize endometrial perfusion noninvasively or vascularity of endometrium during peri implantation period at endometrial –sub endometrial junction and assessing the Uterine Biophysical Profile [9].
Physiology Of Implantation
The physiological process of implantation is a well-organized and orchestrated process. The endometrium undergoes series of changes which synchronize with formation of blastocyst. The changes include –
1. Attachment of blastocyst to endometrium
2. Penetration of blastocyst into the stroma
The stroma helps in anchoring, sustaining the embryo, control the invasiveness of trophoblast, produce growth factors and substrates and functions in response to proteins and hormones of ovary and embryo.
Endometrial Changes During Implantation
The change in endometrium occurs in response to the blastocyst development and are in a way picked up on Ultrasound
1. In follicular phase the endometrial growth is tortuous
2. Till ovulation there is increase in glands
3. At ovulation, the glands become tortuous and formation of spiral arteries
4. During implantation time (20, 21, 22 days) the endometrium becomes thick, edematous with predecidual cells. Epithelial lining is filled with mucus film, microvilli and pin pods. These changes are not present at day 16 and vanish by day24 in both spontaneous and induced cycles. These changes and pin pods are said to help in the process of anchoring and sustaining the embryo.
Ultrasound Assessment of Endometrium
During the reproductive years of normal female, the uterus undergoes ultrasonographically detectable changes which are characterized by cyclical changes in the echo pattern of the endometrium. From the first day of the menstrual cycle till the midcycle, the normal endometrium progressively thickens and develops sonographically detectable strata. The appearance is described as layered, trilaminar or five lines. After the mid cycle, the normal endometrium brightens and progressively thins. These sonographically patterns are related to the changes in the glandular and vascular elements of endometrium during the menstrual cycle. The endometrium either sloughs off if no pregnancy or will undergo changes in the event of pregnancy. In preparation for implantation, the endometrium undergoes transformations influenced by the ovarian hormones produced in the early secretory phase. These modifications include increase in the blood flow, number of cells populating the stroma and epithelium, uterine oxygen consumption oxygen diffusion into the uterine lumen and a generalized edema. The endothelium of spiral arteries undergoes proliferation, thickening of the wall and coiling. The chances for a normal implantation may be reduced if the spiral arteries are inadequately developed. Changes in the endometrial vascularity may be picked up on color Doppler. By Ultrasound and color Doppler the endometrial changes picked up on histologic examination by pathologist may be complemented or substantiated. The endometrial and peri endometrial areas can be divided into four zones:
Zone 1- A 2mm thick area surrounding the hyperechoic outer layer of endometrium
Zone 2- The hyperechoic outer layer of the endometrium
Zone 3 – The hypoechoic inner layer of endometrium
Zone 4- The endometrial cavity
The variations in the depth of vascular penetration before, during and mid cycle of menstrual cycle can be seen on ultrasound. Most patients demonstrate flow into zone 3 by mid –cycle and are presumed normal (Tables 1 & 2). Also sub endometrial arteries doppler indices (RI and PI) are studied at 1-2 mm lateral to the outer edge of the endometrium. Uterine artery PI and RI were recorded from the uterine artery main branch on the lateral edge of the cervix. Applebaum [10] in his scoring system proposed USSR perfect score of 20 has been associated with 100 percent chances of conception Scores of 17-19 have been associated with 80 percent chances of conception. Scores of 14 to 16 have 60 percent while score of 13 or less resulted in no pregnancy.
Table 1: Uterine Biophysical Profile [10] Certain sonographic qualities of the uterus may be noted during the normal mid cycle. These include 7 parameters.
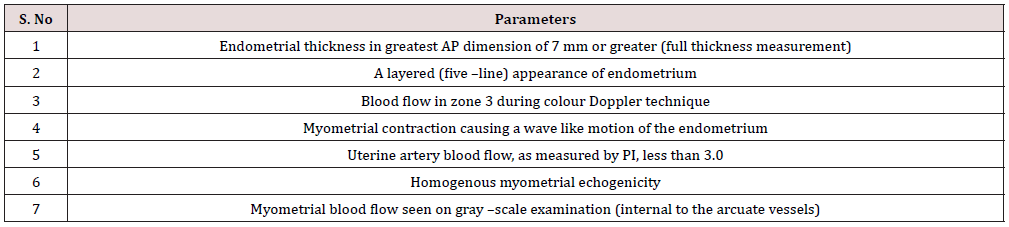
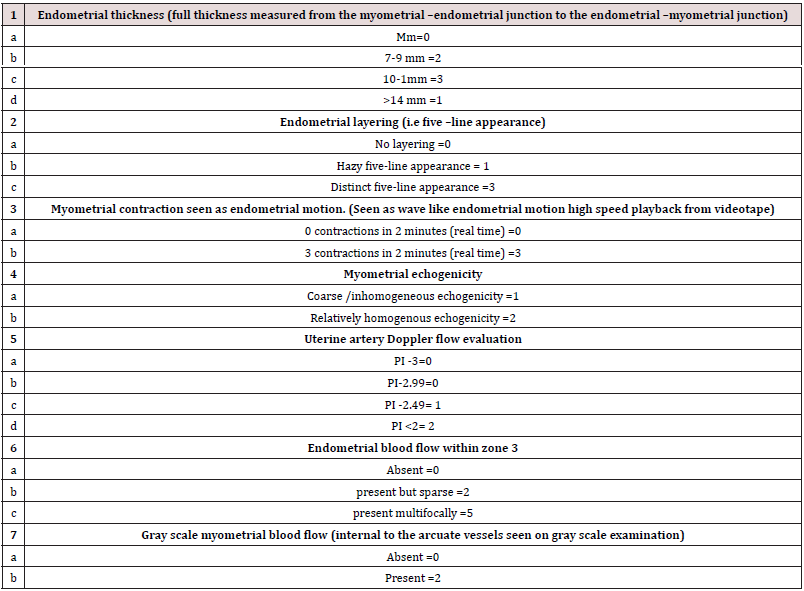
Table 2: The Uterine scoring system for reproduction (USSR) comprises evaluation of the following parameters with a score.
Discussion
Implantation appears to be the weakest link for the success of any ART procedure. Several parameters and techniques have been studied to assess the implantation potential of endometrium. Several studies have found better implantation rates when the endometrium was multilayered with echogenicity’s in the hypoechoic areas in between the lines [11,12]. Conventionally, endometrial thickness (ET) of greater than 7 mm and a triple –layered endometrial pattern were considered as markers of endometrial receptivity. No doubt other factors apart from sonographic signs of ‘uterine receptivity ‘are at work in determining conception. However, Doppler Ultrasound could be used as a parameter to predict negative outcome especially in IVF cycle pretransfer. If failure could be predicted, the embryos could be frozen until a more favorable cycle appears based on scoring criteria like USP and USSR [10,13]. This could prevent embryo wastage and subsequent patient disappointment. Human placentation is a complex interplay of factors involving the endometrium and the blastocyst and abnormalities of placentation are associated with diseases such as miscarriage and pre-eclampsia [14]. Both these complications stem from a defect in early trophoblast invasion and a failure to convert the spiral arteries into low resistance channels. Therefore, defective placentation’s is mainly characterized by a thinner and fragmented trophoblastic shell and reduced cytotrophoblast invasion of the lumen at the tips of the spiral arteries [15]. It is now possible to predict early, and late pregnancy complications related to abnormal placentation on account of the ability of the colour Doppler imaging to detect small vessels such as the terminal part of the uteroplacental circulation.
A temporary but exclusive sequence of factors that make the endometrium amenable to embryonic implantation has been referred to as endometrial receptivity [16]. It is only the period of implantation window that there is an optimal time for blastocyst implantation. The endometrium otherwise gives a non-receptive environment for blastocyst implantation. During a regulated implantation window on day 6-10 post ovulation can a human embryo develop while rest of the time is surrounded by refractory endometrial status [16]? Tissue remodeling and angiogenesis are hallmark events during implantation and decidualization. The dynamic changes in the endocrine state of female during the menstrual cycles and pregnancy result in extensive remodeling of the uterine tissue. The secretory phase of 21 to 22 days of cycle is characterized by endometrial stromal edema with an increase in vascular surface area. These changes may be the result of estrogen and progesterone mediated increase in prostaglandins and VEGF production in the endometrium causing vascular permeability. One of the strongest predictors of implantation is ET, which is dependent on several factors including reproductive age, phase of menstrual cycle, ovarian hormone concentration and endometrial hormone receptor density [17]. Substantiating information has been reported in various other cases where the assessment of ET was used to predict pregnancy outcome following IVF-E [18]. Studies suggest that the highest pregnancy rate (50%) was seen when ET was around 8-10 mm, least (2.5%) when the ET was either more than 14 mm or less than 8 mm [19] Oliveria JB [20] by their study concluded that pregnancies did not occur when the endometrial thickness was less than 7 mm. others reported a minimal endometrial thickness of 6 mm to be acceptable for implantation [21].
However, the implantation rates may be more correlated to the vascularity of the endometrium rather than only the thickness and morphology of the endometrium. Varying distribution of vascular zones suggesting poor vascularity has also been recognized as endometrial receptivity marker. Reports from studies show higher pregnancy rates in highly vascular endometrium in contrast to increased miscarriages in pre pregnancy poor vascular endometrium even after successful IVF-ET [22-24]. A substantially higher concentration of growth factors and interleukins are produced by good healthy vascular endometrium aiding in better implantation and better pregnancy outcome .The zones of vascularity as defined by Appelbaum [10] as zone 1 when the vascularity on power doppler is seen only at endometrial myometrial junction , zone 2 when vessel penetrate through the hypoechogenic endometrial edge, zone 3 when it reaches the intervening hyperechogenic zone and zone 4 when they reach the endometrial cavity Singh et al [25] in their study found a higher pregnancy rate when the blood flow to the endometrium was in the zone III (51.8%) as compared to Zone I (14.8 %).Another study [26] emphasized that sub endometrial flow is vital to determine pregnancy outcome.
Conclusion
Infertile couples undergo immense stress and depression. If the basic treatment does not make them conceive then various methods of assisted reproduction techniques demand great amount of time, energy, mental, physical exhaustion and substantial finances drainage. UBP and USSR may be utilized as simple, rapid, noninvasive parameters to predict uterine environment and assess the pregnancy outcome. The article highlights the role of UBP and USSR, endometrial thickness and peri ovulatory endometrial blood flow in predicting favorable outcome in the form of pregnancy in couples of unexplained fertility while undergoing IVF. However, its role in spontaneous conceptions is limited and yet to be assessed.
Sources of Funding
Nil.
Conflict of Interest
Nil.
References
- Torry DS, Leavenworth J, Chang M, Maheshwari V, Groesh K, et al. (2007) Angiogenesis in implantation. J Assist Reprod Genet 2: 303-315.
- World Health Organization (2020) Infertility definitions and terminology.
- Walker MH, Tobler KJ (2021) Female Infertility. In Stat Pearls Florida Stat Pearls Publishing, USA.
- Yang ICM (2020) A journey of hope: an institutional perspective of Japanese outbound reproductive tourism. Curr Issues in Tourism 23: 52-67.
- Maurya VK, DE Mayo FJ, Lydon JP (2002) Illuminating the Black Box of early pregnancy loss. Hum Reprod Update 8(4): 333-343.
- Hertig AT, Rock J, Adams EC (1956) A description of 34 human ova within the first 17 days of development. Am J Anat 98(3): 35-91.
- Croxatto HB, Diaz S, Fuertealba BA (1972) Studies on the duration of egg transport in human oviduct. Fertil Steril 23(7): 47-58.
- Buster JE, Bustilo M, Rodi IA (1985) Biologic and morphologic development of donated human ova recovered by nonsurgical uterine lavage. Am J Obstet Gynecol 153(2): 211-217.
- Khan MS, Sheikh A, Ratnai R (2016) Ultrasonography and Doppler Study to Predict Uterine Receptivity in Infertile Patients Undergoing Embryo Transfer. J Obstet Gynaecol Inia 66 (Suppl 1) 9: 377-382.
- Applebaum Michael (1997) The Uterine Biophysical Profile (UBP 0Endosonography in Obstetrics and Gynaecology. Gautam Allahabadia (Ed) Rotunda Medical Technologies (P) Ltd. Mumbai, India pp. 33-52.
- Smith B, Porter R, Ahuja K, Craft I (1984) Ultrasonic assessment of endometrial changes in stimulated cycles in an in vitro fertilization and embryo transfer program. J In Vitro Fertile Embryo Transfer 1(4): 233-238.
- Gonen Y, Casper RF (1990) Prediction of implantation by sonographic appearance of the endometrium during controlled ovarian stimulation for in vitro fertilization (IVF). J In Vitro Fertil Embryo Transfer 7(3): 146-152.
- Appelbaum M, Cadkin AV (1992) Decidual flow-An early sign of pregnancy. Ultrasound obstetric gynecology 2: 26.
- Jauniaux E, Johns J and Burton GJ (2005) The role of ultrasound imaging in diagnosing and investigating early pregnancy failure. Ultrasound Obstet Gynecol 25(6): 613-662.
- Hassold TJ (1986) Chromosome abnormalities in human reproductive wastage. Trends Genet 2: 105-110.
- Lessey BA, Kim JJ (2017) Endometrial Receptivity in Eutopic Endometrium of Women with Endometriosis, it is affected, let me show you why. Fertile Steril 108(1): 19-27.
- Teh WT, McBain J, Rogers P (2016) What is the contribution of embryo –endometrial asynchrony to implantation failure? J Assist Reproduc Genet 33(11): 1419-1430.
- Wolff EF, Vahidi N, Alford C, Richter K, Widra E (2013) Influences on endometrial development during intrauterine insemination: Clinica; experience of 2929patients with unexplained infertility. Fertil Steril 100(1):194-9. e1.
- El Zenneni H, Moustafa R, Abdel Hafeez M, El Salally H, Abdel Kder A (2015) Assessment of uterine, subendometrial blood flows and endometrial gland vascular endothelial growth factor (EG-VEGF)in women with unexplained infertility .Middle East Fertile Soc J 20(2): 119-126.
- Abdel Kader M, Abdelmeged A, Mahran A, Abu Samra MF, Bahaa H (2016) The usefulness of endometrial thickness, morphology and vasculature by 2D Doppler ultrasound in prediction of pregnancy in IVF/ICSI cycles. Egypt J Radiol Nucl Med 47(1):341-346.
- Oliveira JB, Baruffi RL, Mauri AL, Petersen CG, Borges MC, et al. (1997) Endometrial ultrasonography as a predictor of pregnancy in an in vitro fertilization programme after ovarian stimulation and gonadotrophin –releasing hormone and gonadotrophins. Hum Reprod 12 (11): 2515-2518.
- Coulam CB, Bustilo M, Soenksen DM, Britten S (1994) Ultrasonographic predictors of implantation after assisted reproduction. Fertil Steril 62(5) :1004 -1010.
- Wang l, Qiao J, Li R, Zhen X, Liu Z (2010) Role of endometrial blood flow assessment with colour Doppler energy in predicting pregnancy outcome of IVF-ET cycles. Reprod Biol Endocrinol 8: 122.
- Singh N, Bhadur A, Mittal S, Malhotra N, Bhatt A (2011) Predictive value of endometrial thickness, pattern and sub–endometrial blood flows on the day of HCG by 2D Doppler in in vitro fertilization cycles: A prospective study from a tertiary care unit. J Hum Reprod Sci 4(1): 29-33.
- Gupta P, Chandra S, Kaushik A, Jain PK (2014) Evaluation of uterine biophysical profile to assess its role in predicting conception among unexplained primary infertility patients. Indian J Community Health 26(4): 1-5.
- Singh N, Bhadur A, Mittal S, Malhotra S, Malhotra N (2011) Bhatt A Predictive value of endometrial thickness, pattern and subendometrial blood flows on the day of Hcg by 2D Doppler in invitro fertilization cycles: Aprospective clinical study from a tertiary care unit. J Hum Reprod Sci 4(1): 29-33.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...





