Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Research Article(ISSN: 2637-4544) 
Pethidine Infiltration in Intra Fascial Layer After Abdominal Hysterectomy Volume 3 - Issue 1
Raafat TA1* and Mostafa M Serry2
- 1 Obstetrics and Gynecology Department, Ain Shams University, Egypt
- 2 Anesthesia Department, Ain Shams University, Egypt
Received:December 30, 2018; Published: January 10, 2019
Corresponding author: Tarek Aly Raafat, Assistant professor of Obstetrics and Gynecology, Obstetrics and Gynecology Department, Ain Shams University, Cairo, Egypt
DOI: 10.32474/IGWHC.2019.03.000153
Abstract
Introduction: multimodal analgesia regimen has a cornerstone component involving local wound infiltration with analgesic agents to manage and enhance post-operative pain to increase patient satisfaction.
Aim: assessment and evaluation of effectiveness of local pethidine infiltration as a local analgesic in total abdominal hysterectomy.
Methodology: A cohort of 151 cases that have undergone abdominal hysterectomy have been categorized randomly into two research groups research group I (n=74 cases), involved women that were administered both wound infiltration and IM pethidine; and research group II (n=77 cases), involving women that were administered IM pethidine.
Results: The median 10-cm VAS for postoperative pain was significantly lower in women who received both WI and IM pethidine when compared to women who received only IM pethidine, 1 hour, 6 hours, 12 hours and 24 hours postoperatively. The mean total morphine consumption was lower in women who received both WI and IM pethidine when compared to women who received only IM pethidine.
Conclusion: Pethidine when administered in a simultaneous manner intrafascially and intramuscularly in cases undergoing total abdominal hysterectomy is more effective in reducing post-operative pain levels
Introduction
Post-operative pain management in cases undergoing total abdominal hysterectomy is considered a major challenge for both gynecologists and anesthesiologists aiming for enhancing patient satisfaction and level of health care service requiring multidisciplinary management and planning regarding the pathway of pain management of pain [1,2]. Despite the fact that epidural form of analgesia is an efficient mode of managing post-operative pain in abdominal surgeries however less invasive forms are considered more practical and applicable for many health care systems [3,4].
Local analgesia infiltration is considered a simple and efficient mode of pain management that has reduced costs in comparison to epidural analgesia. Advancing the pain management protocols could enhance patient post-operative recovery and improve clinical outcomes [5,6]. A widely implemented synthetic opioid known as pethidine causes its analgesic action by Functioning as an agonist on opioid receptors, furthermore it has been revealed and displayed to exert a local anesthetic impact chiefly via Linked to its interfaces with sodium‑ion Channels that are voltage‑dependent. peripheral nerve conduction blockage action has been revealed and displayed widely in various in vivo and in vitro experimental animal research studies that makes its applicability in clinical practice in humans a promising protocol of management [7,8].
Furthermore, pethidine has been shown to block conductivity in both motor and sensory neural systems via electrophysiological research studies making this issue a matter of interest to investigate its impact on patients undergoing abdominal surgeries via research studies aiming to merge from them evidence-based protocols in practice [9,10]. The privilege of local anesthetic agents’ infiltration interestingly has revealed that there are no local anesthetic toxicity issues arise if properly administered in a professional manner, no wound infection or healing issues due to usage of this form of analgesia making it an attractive mode for postoperative pain management for both gynecologists and anesthesiologists [11,12].
Aim of the Study
Assessment and evaluation of effectiveness of local pethidine infiltration as a local analgesic administered intrafascially in total abdominal hysterectomy.
Methodology
A randomized controlled research trial performed at Ain Shams University Maternity Hospital 151 cases that have undergone abdominal hysterectomy have been categorized randomly into two research groups research group I (n=74 cases), involved women that were administered both wound infiltration and IM pethidine; and research group II (n=77 cases), involving women that were administered IM pethidine. Oral and written consent form was obtained from the study subjects with the American Society of Anesthesiologists physical Status I‑II, aged range 45 to 65 years, who were recruited for total abdominal hysterectomy and bilateral salpingo‑oophorectomy, under general anesthesia via performing a Pfannenstiel incision. The exclusive research criteria involved malignancy, cases on chronic analgesic agents, known allergy to local anesthetics, morphine, pethidine, or nonsteroidal anti‑inflammatory drugs, with chronic hepatic disease, chronic renal impairment, coagulation abnormalities and DM. After performance of wound closure, cases recruited for wound infiltration research group were administered 1mg/kg of pethidine dosage divided half intrafascially, prepared in a 15ml saline syringe and an half IM injection in simultaneous manner in a solution of 2.5ml saline, while the cases recruited for the IM research group were administered an IM injection of 1mg/kg pethidine in a solution of 2.5ml saline with simultaneous infiltration of 15ml of normal saline intrafascially.
Pain assessment
was conducted by usage of a point visual analogue scale (VAS) at 1, 6, 12 hours, at 24 at rest and with cough in the post-operative period. The study subject was asked to mark on the line the pain she feels. The usage of standard 10cm visual analogue scale (VAS) for scoring pain level was explained to the patient during the preoperative visit represented 0=no pain and 10=the most severe pain.
Ethical approval
The research study had approval from the Ethical Committee of the Department of Obstetrics and Gynecology, Faculty of Medicine, Ain Shams University and fulfilling declaration of Helsinki ethical principles for medical research involving human study subjects 2001.
Sample size justification
Data from a previous study Stamatakis et al. [12] showed that the mean values for 24-hour total morphine consumption in cases who received wound infiltration and in those who received intramuscular pethidine were 11.33 ± 8.3 mg and 15.56 ± 9.69 mg, consecutively (p< 0.05). Calculation according to these values, setting the type-1 error (α) at 0.05 and the power (1-β) at 0.8, produced a minimal sample size of 72 women in each group. Assuming a drop-out rate of 5%, a total number of 154 cases were needed to be randomized into two groups.
Statistical methods
Statistical analysis was performed using Microsoft Excel version 2016 and SPSS for Windows version 22.0. Data were presented as range, mean and standard deviation (for normally distributed data); range, median and interquartile range (for discrete or skewed data); or number (percentage) for categorical data. Difference between the two groups was analyzed using independent student’s t-test (for normally distributed data); Mann-Whitney’s U-test (for discrete or skewed data); or chi-squared test for categorical data. The mean differences and risk ratios were presented with their 95% confidence intervals, as well. Significance level was set at 0.05.
Results
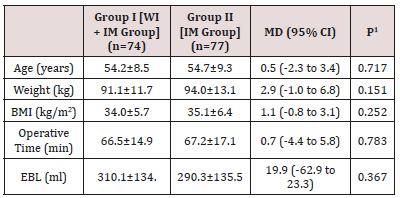
WI wound infiltration
IM intramuscular
BMI body mass index
EBL estimated blood loss
Data presented as mean ± standard deviation
MD (95% CI) mean difference and its 95% confidence interval
1 Analysis using independent student’s t-test
Table 1 reveals and displays that there was no statistically significant difference as regards age (years), weight (kg), BMI (kg/m2), operative time (min), estimated blood loss (ml) (p values =0.717,0.151,0.252,0.783,0.367, consecutively).
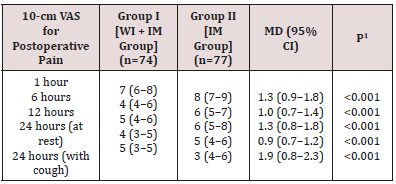
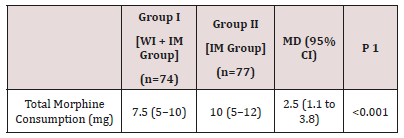
A total of 151 women who underwent abdominal hysterectomy completed the study were included in the final analysis. They were randomized into one of two groups: group I (n=74), including women who received both wound infiltration and IM pethidine; and group II (n=77), including women who just received IM pethidine. (Table 1) shows the initial characteristics of included women in Citation: Raafat TA, Mostafa M S. Pethidine Infiltration in Intra Fascial Layer After Abdominal Hysterectomy. Int Gyn & Women’s Health 3(1)- 2019. IGWHC.MS.ID.000153. DOI: 10.32474/IGWHC.2019.03.000153. 3/4 both groups. There were no significant differences between women of both groups, regarding the age, weight, BMI, estimated blood loss and operative time. The median 10-cm VAS for postoperative pain was significantly lower in women who received both WI and IM pethidine when compared to women who received only IM pethidine, 1 hour, 6 hours, 12 hours, and 24 hours postoperatively (Table 2, Figure 1). The mean total morphine consumption was lower in women who received both WI and IM pethidine when compared to women who received only IM pethidine (Table 3). As regards the pethidine-related adverse effects, the rates of nausea/ vomiting were comparable in both groups of women. The median sedation score was, however, significantly higher in women who received both WI and IM pethidine when compared to women who received only IM pethidine (Table 4).
WI wound infiltration
IM intramuscular
VAS visual analogue scale
Data presented as median (interquartile range)
MD (95% CI) mean difference and its 95% confidence interval
1 Analysis using Mann-Whitney’s U-test
Table 2 reveals and displays interestingly a statistically significant difference as regards VAS scoring between group I and group II at 1,6,12,24 (at rest), 24 (with cough) (p values < 0.001) being lower in research group I (wound infiltration +IM).
WI wound infiltration
IM intramuscular
Data presented as median (interquartile range)
MD (95% CI) mean difference and its 95% confidence interval
1 Analysis using Mann-Whitney’s U-test
Table 3 reveals a statistically significantly lower morphine consumption levels in the research group administered both wound infiltration and IM pethidine administration than the IM only research group. (p value< 0.001).
WI wound infiltration
IM intramuscular
Data presented as median (interquartile range); or number (percentage)
MD (95% CI) mean difference and its 95% confidence interval
RR (95% CI) risk ratio and its 95% confidence interval
1 Analysis using Mann-Whitney’s U-test
2 Analysis using Chi-Squared test
Table 4 reveals clearly that sedation score levels were much higher in a statistically significant manner in the research group administered both wound infiltration and IM pethidine administration than the IM only research group. (p value< 0.001) whereas there was no statistically significant difference as regards nausea and vomiting between both research groups (p value=0.420).
Discussion
Infiltrative form of analgesia locally acts by blockage of pain transmission due to triggering of voltage‑dependent sodium channels, and additionally, sensitizes noci receptors by decreasing inflammatory mediators release responsible for pain [13,14]. Exploring and advancing post-operative pain management is a crucial issue in gynecological practice particularly in frequently performed procedures such as total abdominal hysterectomy .Pethidine as a frequent and preferred analgesic implemented for control of pain could be administered in a more efficient manner when considering its usage in a local and systemic manner that raises the effectiveness in the total performance level of the agent as an analgesic [1,3,5]. The current research study revealed and displayed the following findings that prove the higher privilege in administering I.M pethidine and local fascial layer infiltration to reduce pain levels without increasing side effects such as nausea and vomiting in which sedation score levels were much more higher in a statistically significant manner in the research group administered both wound infiltration and IM pethidine administration than the IM only research group.(p value< 0.001) whereas there was no statistical significant difference as regards nausea and vomiting between both research groups (p value=0.420).
Figure 1: VAS for Postoperative Pain in Included Women in Both Groups. Figure 1 displays clearly lower VAS scoring levels in cases having simultaneous administration of Pethidine intrafascially and intramuscular forms in research group I in comparison to research group II having intramuscular pethidine only. .
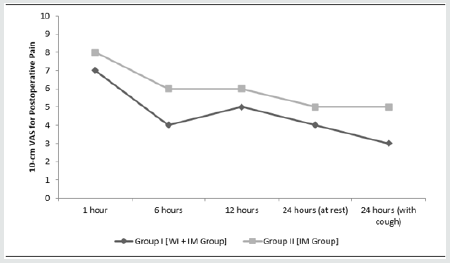
Concerning pain levels estimated by using VAS scoring system Table 2 reveals and displays interestingly a statistically significant difference as regards VAS scoring between research group I and research group II at 1,6,12,24 (at rest), 24 (with cough) (p values < 0.001) being lower in research group I (wound infiltration +IM). That finding could be justified by the fact that both the local action of pethidine on sodium channels and systemic action on opioid receptors have been elicited by using wound infiltration in the fascial layer and I.M forms of administration adding a clinical value in patient recovery within the post-operative period.
As regards morphine consumption that is an issue of concern for clinicians and surgeons due to the fear of possible clinical side effects Table 3 reveals a statistically significantly lower morphine consumption levels in the research group administered both wound infiltration and IM pethidine administration than the IM only research group. (p value< 0.001). Similarly, a prior research study similar to the current research have revealed that the effectiveness of wound infiltration during performance of total abdominal hysterectomies, in decreasing the opioid consumption levels during the first 24 hours of postoperative period that is in great harmony with the current research study results that issue could be justified by a hypothesized mechanism demonstrated in abdominal surgeries by usage of a neuroanatomical approach. Similarly, prior research groups have revealed interestingly that subcutaneous administration of pethidine, in comparison to bupivacaine, have an opioid‑sparing impact after cesarean delivery procedures [7,9,11].
Similarly another research study performed by a similar methodology performed to evaluate the effectiveness of sole administration of pethidine intrafascially in comparison to I.M injection have shown that Postoperative VAS scoring levels have revealed no statistically significant privilege between wound infiltration and intramuscular method, whereas the total consumption of morphine was lower in the IM, in comparison to the wound infiltration research group (27.2%). The research team in that study came to the conclusion that local wound infiltration with pethidine after total abdominal hysterectomy did not decrease the total morphine consumption levels within the first 24 hours postoperatively that shows great contradiction to the current research study findings [12].
As a sole agent pethidine, was displayed by prior research team of investigators to be efficient and effective in accomplishing a successful transversus abdominis blockage during conductance laparoscopic cholecystectomy [2,4,15]. Furthermore, there are numerous research studies assessing the local analgesic effectiveness of pethidine, particularly in performing peripheral blockage action. Additionally, in orthopedic surgery research wound infiltration analgesia implementing pethidine causes a postoperative analgesic impact in cases undergoing total hip replacement, chiefly by blockage voltage‑activated sodium channels present within the nerve endings and by interaction with opioid receptors [6,8]. Contradicting with the current research study findings it was revealed priorly that pethidine showed failure to control pain by wound infiltration after performance of laparoscopic tubal ligation. The finding was justified by the research team due to the dosage used, and to the issue that the visceral pain experienced by the cases was more overriding, in comparison with the pain correlated to the wound due to trocar insertion, where the infiltration was conducted. Furthermore, contradicting with the current research study in a similar fashion it was shown that wound infiltration using a local anesthetic had no opioid‑sparing impact after performing total abdominal hysterectomy, as regards morphine consumption levels [10].
Conclusion
Pethidine when administered in a simultaneous manner intrafascially and intramuscularly in cases undergoing total abdominal hysterectomy is more effective in reducing post operative pain levels. However, the current study results should be interpreted with caution as other variables are required to be put in consideration in future research studies such as racial and ethnic differences and normal anatomic integrity such as cases with prior abdominal incisions could have more fibrosis affecting drug absorption levels intra facially. Future research efforts are recommended to be performed in a multicentric fashion with larger numbers of cases to elucidate the usefulness of local pethidine administration by wound infiltration in comparison with other analgesic agents and at different anatomical planes in ac comparative manner such as subcutaneous layer. Other gynecological procedures should be put in consideration in future research such as total laparoscopic hysterectomy and commonly performed obstetric procedure such as cesarean section deliveries in which wound infiltration should be implemented in a manner permitting useful implementation of clinical guidelines aiding in improving postoperative recovery.
References
- Raghvendra KP, Thapa D, Mitra S, Ahuja V, Gombar S, et al. (2016) Postoperative pain relief following hysterectomy: A randomized controlled trial. J Midlife Health 7(2): 65‑68.
- O Sullivan M, Iohom G (2014) Epidural or wound infusion? Minerva Anestesiol 80(7): 756‑758.
- Rawal N (2016) Current issues in postoperative pain management. Eur J Anaesthesiol 33(3): 160‑171.
- Thornton PC, Buggy DJ (2011) Local anaesthetic wound infusion for acute postoperative pain: A viable option? Br J Anaesth 107(5): 656‑658.
- Imani F, Entezary S, Razi M, Jafarian AA, Yousefshahi F, et al. (2015) The effect of intra‑articular meperidine and bupivacaine 0.5% on postoperative pain of arthroscopic knee surgery; a randomized doubleblind clinical trial. Anesth Pain Med 5(1): e27470.
- Hashemi SJ, Soltani H, Heidari SM, Rezakohanfekr M (2013) Preemptive analgesia with intra‑articular pethidine reduces pain after arthroscopic knee surgery. Adv Biomed Res 2: 9.
- Vassiliadis RM, Taylor PG (2013) Spinal pethidine for elective caesarean section. Anaesth Intensive Care 41(1): 113‑115.
- Joshi GP, Schug SA, Kehlet H (2014) Procedure‑specific pain management and outcome strategies. Best Pract Res Clin Anaesthesiol 28(2): 191‑201.
- Onutu AH, Iacob IM, Todor A, Lucaciu DO, Acalovschi I (2012) Wound infiltration with 1% pethidine provided an opioid sparing effect after uncemented total hip arthroplasty: A prospective randomized study. Rom J Anaesth Intensiva Care 19(1): 5‑12.
- Hayden JM, Oras J, Karlsson OI, Olausson KG, Thörn SE, et al. (2017) Post‑operative pain relief using local infiltration analgesia during open abdominal hysterectomy: A randomized, double‑blind study. Acta Anaesthesiol Scand 61(5): 539‑548.
- Joshi GP, Janis JE, Haas EM, Ramshaw BJ, Nihira MA, et al. (2016) Surgical site infiltration for abdominal surgery: A novel neuroanatomical‑based approach. Plast Reconstr Surg Glob Open 4(12): e1181.
- Stamatakis E, Kalopita K, Hadzilia S, Theofanakis C, Valsamidis D (2018) Local analgesic effect of pethidine infiltrated intrafascially after total abdominal hysterectomy: A randomized, double-blind study. J Nat Sc Biol Med 9(2): 211-216.
- Jabalameli M, Safavi M, Honarmand A, Saryazdi H, Moradi D, et al. (2012) The comparison of intraincisional injection tramadol, pethidine and bupivacaine on post cesarean section pain relief under spinal anesthesia. Adv Biomed Res 1: 53.
- Khalaf WM, Ibrahim MEM, Safwat S (2018) Subrectal and Subcutaneous Wound Infiltration with Bupivacaine versus Pethidine for Post Cesarean Section Pain Relief: Randomized Controlled Trial. Open Journal of Obstetrics and Gynecology 8(11): 1071-1083.
- Breazu CM, Ciobanu L, Bartos A, Bodea R, Mircea PA, et al. (2017) Pethidine efficacy in achieving the ultrasound‑guided oblique subcostal transversus abdominis plane block in laparoscopic cholecystectomy: A prospective study. Bosn J Basic Med Sci 17(1): 67‑73.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...