
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Research Article(ISSN: 2637-4544) 
Non-Penicillin Antibiotic Protocols Impact and Influence on Neonatal and Maternal Clinical Outcomes in Cases of Preterm Premature Rupture of Membranes Clinical Scenarios Volume 3 - Issue 5
Waleed Tawfik1* and Marwa Elsayed Ahmed2
- 1Obstetrics and Gynecology Department, Faculty of Medicine, Benha University, Egypt
- 2Pediatrics Department, Faculty of Medicine, Benha University, Egypt
Received:September 03, 2019; Published: September 23, 2019
Corresponding author: Waleed Tawfik, Lecturer of Obstetrics and Gynecology, Obstetrics and Gynecology Department, Faculty of Medicine, Benha University, Benha, Egypt
DOI: 10.32474/IGWHC.2019.03.000172
Abstract
Background: Preterm premature rupture of membranes is a challenging obstetric clinical scenario, since management requires a careful balance between maternal wellbeing and tolerance for continuation of pregnancy and fetal wellbeing and maturity issues.
Aim: The influence and effect of non-β-lactam antibiotic administration on the expectant management course of PPROM as regards the neonatal morbidity, mortality issues and maternal Additionally, infectious clinical outcomes.
Methodology: Research study subjects inclusive research criteria singleton, with no congenital fetal anomalies’ gestations affected by Preterm premature rupture of membranes at or beyond 240/7 gestational weeks of gestation and delivery at less than 350/7 gestational weeks. 350 research study subjects were recruited for the research study categorized into two research groups β- lactam and macrolide and non-β-lactam and macrolide research groups.
Results: Adjusted odds ratio of maternal and neonatal outcomes for women receiving a β-lactam and macrolide compared with a non-β-lactam regimen showing statistical significance as regards bronchopulmonary dysplasia, endometritis (p value=0.012, 0.007 consecutively), whereas neonatal composite clinical outcome and chorioamnionitis didn’t show statistical significance (p value=0.67,0.367).
Conclusion: Cases having preterm premature rupture of membranes that have been administered a β-lactam and macrolide regimen are at lower risk to develop endometritis. Additionally, among neonates with PPROM the administration of a β-lactam antibiotics doesn’t affect the neonatal morbidity rates.
Introduction
Preterm premature rupture of membranes is a challenging obstetric clinical scenario, since management requires a careful balance between maternal wellbeing and tolerance for continuation of pregnancy and fetal wellbeing and maturity issues. Furthermore, unexpected serious infectious complications are highly prevalent to arise particularly when proper preventive measures are not undertaken such as antibiotic administration such as chorioamnionitis development that could worsen the prognosis [1-3].
On the other hand the choice of the proper antibiotic regimen is crucial for the successful course of management .Penicillin remains the most safe antibiotic family implemented in those category of clinical scenarios since it is the most investigated antibiotic family investigated in research studies, however other antibiotic groups are required to be investigated since issues of antibiotic resistance is an area of global research interest and concerns. Restricted research data and studies for alternative antibiotic regimens narrows the management options available for cases having PPROM [4-6].
Neonatal clinical outcomes should almost always be respected as regards non penicillin antibiotic regimens investigatory research efforts, since the obstetric medicine art relies on both the maternal and perinatal safety issues [7-9].
Another issue of concern is how to deal with cases having PPROM and penicillin allergy that further narrows the available investigated antibiotics and their safety profile on neonatal levels in clinical scenarios of PPROM. Antibiotics as a management agent in cases of PPROM are of cornerstone importance since they prolong the latency period besides preventing and reduce some grave complications such as sepsis at maternal and neonatal levels [10- 13].
Aim of the Work
The influence and effect of non-β-lactam antibiotic administration on the expectant management course of PPROM as regards the neonatal morbidity, mortality issues and maternal Additionally, infectious clinical outcomes.
Methodology
This study was done at Benha University hospital in the Obstetrics & Gynecology and Radiology departments.
Research study subjects inclusive research criteria singleton, with no congenital fetal anomalies gestations affected by Preterm premature rupture of membranes at or beyond 240/7 gestational weeks of gestation and delivery at less than 350/7 gestational weeks. 350 research study subjects were recruited for the research study categorized into two research groups β-lactam and macrolide and non-β-lactam and macrolide research groups. Exclusive research criteria involved the presence of multi fetal gestation, gestations affected by chromosomal Anomalies. Cases administered the gold standard antibiotic protocol β- lactam and macrolide have been compared in analytical manner to cases administered a non-β- lactam and macrolide protocol. The primary research outcome has been neonatal clinical outcomes e.g. necrotizing enterocolitis, intraventricular hemorrhage, periventricular leukomalacia, bronchopulmonary dysplasia, neonatal mortality, sepsis, and cerebral palsy. Secondary outcomes research included, latency period of pregnancy, and endometritis and chorioamnionitis.
Statistical Analysis
Research Data were collected, revised, coded and entered to the Statistical Package for Social Science (IBM SPSS) version 23. Quantitative data were presented as mean, standard deviations and ranges when parametric and compared between the two groups using independent t-test while qualitative variables were presented as number and percentages and compared between groups using Chi-square test and/or Fisher exact test. Multivariable logistic regression analysis was done using backward stepwise regression model to assess the effect of β-lactam and macrolide after adjustment of covariates in the regression model including those significant in the bivariate analysis. The confidence interval was set to 95% and the margin of error accepted was set to 5%. So, the p-value was considered significant at the level of < 0.05.
Results
Table 1 reveals and displays the Demographic data, delivery data and neonatal characteristics between the two investigated research groups (β-lactam, and macrolide regimen research group, Non β-lactam regimen research group ) in which there was no statically significant difference as regards maternal age, High school education or less, Obese (BMI > 30), Multiparous, prior PTB , Smoking, GBS positive, Diabetes, any prenatal care, Any magnesium exposure, Corticosteroids, tocolytic exposure, Spontaneous labor, Gestational age at delivery (weeks), mean ± SD, Cesarean delivery, Mean birth weight (g), mean± SD, Male infant,5-minute Apgar’s score < 7 (p values=0.068, 0.644, 0.828, 0.432, 0.251, 0.956, 0.470, 0.756, 0.372, 0.869, 0.235, 0.943, 0.924, 0.058, 0.791, 0.123, 0.341, 0.738 consecutively) however there was statically significant difference between both research groups as regards drug usage, Gestational age at membrane rupture (weeks), mean± SD, Exposure to clindamycin (p values =0,043, 0.024, <0.001 consecutively).
Table 1: Demographic data, delivery data and neonatal characteristics between the two studied groups.
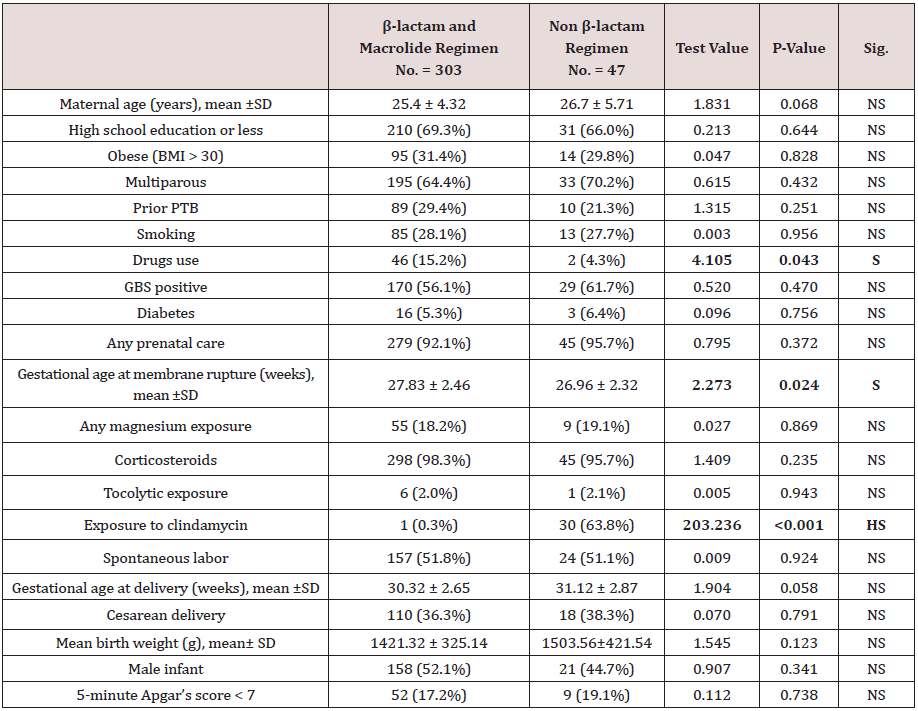
Bold indicates significant
BMI: Body Mass Index; GBS: Group B Strep; BEAM: Beneficial Effects of Antenatal Magnesium Sulfate; PCN: Penicillin; PPROM: Preterm Premature Rupture of Membranes; PTB: Preterm Birth.
Table 2 reveals and displays the comparative statistical analysis among both research groups as regards maternal and neonatal clinical outcomes in which there was no statistical significant difference as regards Maternal clinical outcomes Latency until delivery (days) mean± SD, Endometritis, Chorioamnionitis, Neonatal clinical outcomes Composite, Sepsis, Death in NICU, Severe IVH, PVL, Severe NEC, Any cerebral palsy (p values =0.452, 0.499, 0.512, 0.275, 0.274, 0.833, 0.814, 0.235, 0.206, 0.370), however there was statistically significant higher bronchopulmonary dysplasia among Non β-lactam regimen In comparison to β-lactam and macrolide regimen (p value=0.002); as shown in Figure 1.
Table 2: Comparative statistical analysis among both research groups as regards maternal and neonatal clinical outcomes.
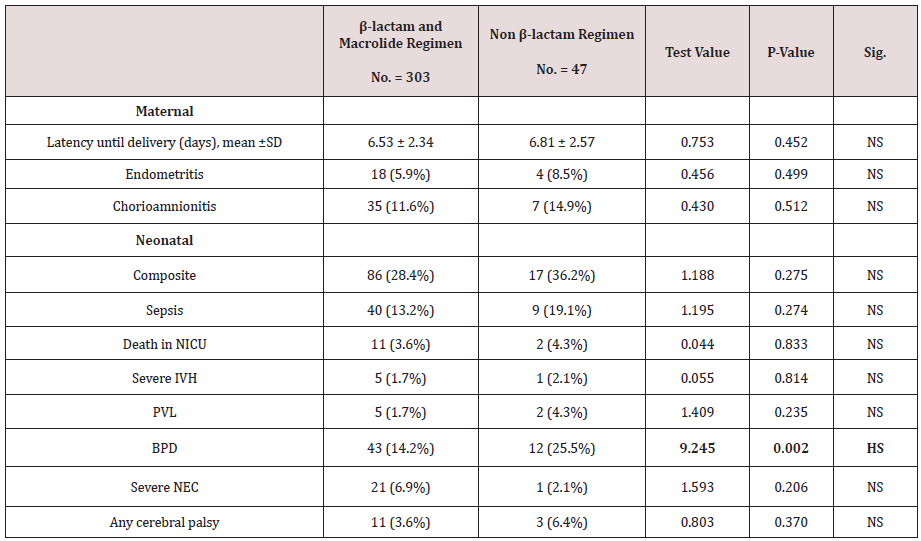
Bold indicates significant
BPD, Bronchopulmonary Dysplasia; IVH, Intraventricular Hemorrhage; NEC, Necrotizing Enterocolitis; NICU, Neonatal Intensive Care Unit; PVL, Periventricular Leukomalacia.
Figure 1: Comparative statistical analysis among both research groups as regards maternal and neonatal clinical outcomes.

Table 3 reveals and displays the Adjusted odds ratio of maternal and neonatal outcomes for women receiving a β-lactam and macrolide compared with a non-β-lactam regimen showing statistical significance as regards bronchopulmonary dysplasia, endometritis (p value=0.012,0.007 consecutively), whereas neonatal composite clinical outcome and chorioamnionitis didn’t show statistical significance (p value=0.67,0.367) . Table 1 Demographic data, delivery data and neonatal characteristics between the two studied groups
Table 3: Adjusted odds ratio of maternal and neonatal outcomes for women receiving a β-lactam and macrolide compared with a non-β-lactam regimen.
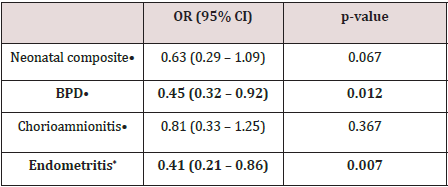
Bold indicates significant
OR: Odds Ratio; 95% CI: 95% Confidence Interval; BPD, Bronchopulmonary Dysplasia. •: Adjusted for marital status, maternal drug use, clindamycin exposure and gestational age at membrane rupture. *: Adjusted for marital status, maternal drug use, clindamycin exposure, gestational age at membrane rupture and chorioamnionitis.
Discussion
Antibiotics in management of preterm premature rupture of membranes clinical scenarios have a cornerstone safeguard role against developing highly morbid and serious maternal and perinatal infectious complications. The choice of antibiotic regimen administration and protocol is a decision that could be lifesaving since it prevents postpartum endometritis and sepsis particularly in early neonatal life [3,9,10].
A prior research team of investigators conducting a research study similar in approach and methodology to the current study it was revealed that cases having PPROM, that were administered a non-β-lactam and macrolide antibiotic protocol had a raised clinical risk of endometritis. Interestingly in harmony with the current research study findings prior research efforts have revealed that neonates delivered to cases that were administered the gold standard antibiotic protocol of a β-lactam and macrolide had lower clinical risk of developing bronchopulmonary dysplasia and on the other hand had raised risk of severe necrotizing enterocolitis [1,4,7,13]. Previous, multicentric large, randomized controlled clinical trials assessing the usage of ampicillin and erythromycin on a neonatal clinical outcome have revealed the valuable and effective role of this regimen in reducing grave infectious complications. Furthermore, in great similarity and harmony with the current study findings have demonstrated a reduction in neonatal morbidity rates, respiratory distress, necrotizing enterocolitis, sepsis, pneumonia, patent ductus arteriosus, bronchopulmonary dysplasia, and hyperbilirubinemia in cases that were administered the beta lactam and macrolide antibiotic regimens [2,5,6]. Interestingly previous research efforts have clearly demonstrated that antibiotics in general reduce maternal chorioamnionitis and pregnancy latency in cases affected by preterm premature rupture of membranes. Furthermore, it was interestingly observed by prior research teams and investigators that postpartum infectious morbidities are more frequent among cases that were administered non-β-lactam regimens [7,12]. Additionally, it is clearly displayed that rising rates of severe necrotizing enterocolitis among neonates administered a β-lactam protocol is well demonstrated by investigators all over the globe [9,11,13].
Prior research efforts have concluded that there is raised clinical risk of necrotizing enterocolitis correlated to usage of coamoxiclav, and ampicillin antibiotics. those research findings are justified at molecular and cellular levels that there is affection of neonatal microbiota that id a possible cause for the development of necrotizing enterocolitis. besides it is clearly proven that maternal antibiotic administration antepartum Alters the neonate’s bacterial colonization pattern within the intestine [2,8,12].
Conclusion and Recommendations for Future Research
Cases having preterm premature rupture of membranes that have been administered a β-lactam and macrolide regimen are at lower risk to develop endometritis. Additionally, among neonates with PPROM the administration of a β-lactam antibiotics doesn’t affect the neonatal morbidity rates. However future research efforts are required to be multicentric in nature to elucidate and analyses the detailed neonatal morbidity issues according to antibiotic regimens taking in consideration the usage of cephalosporins in cases that have penicillin allergy.
References
- Waters TP, Mercer B (2011) Preterm PROM: Prediction, prevention, principles. Clin Obstet Gynecol 54(2): 307–312.
- Macy E (2014) Penicillin and beta-lactam allergy: Epidemiology and diagnosis. Curr Allergy Asthma Rep 14(11): 476
- Kenyon S, Boulvain M, Neilson JP (2003) Antibiotics for preterm rupture of membranes. Cochrane Database Syst Rev (2): CD001058
- Hopkins MK, Dotters Katz S, Boggess K, Heine RP, Smid M (2018) Perioperative antibiotic choice in labored versus unlabored Cesareans and risk of post cesarean infectious morbidity. Am J Perinatol 35(2): 127–133
- Weintraub AS, Ferrara L, Deluca L, Moshier E, Green RS, et al. (2012) Antenatal antibiotic exposure in preterm infants with necrotizing enterocolitis. J Perinatol 32(9): 705–709.
- Hall CM, Milligan DW, Berrington J (2004) Probable adverse reaction to a pharmaceutical excipient. Arch Dis Child Fetal Neonatal 89(2): F184
- Silverman MA, Konnikova L, Gerber JS (2017) Impact of antibiotics on necrotizing enterocolitis and antibiotic associated diarrhea. Gastroenterol Clin North Am 46(1): 61–76
- Nogacka A, Salazar N, Suárez M, Milani C, Arboleya S, et al. (2017) Impact of intrapartum antimicrobial prophylaxis upon the intestinal microbiota and the prevalence of antibiotic resistance genes in vaginally delivered full-term neonates. Microbiome 5(1): 93
- Munyaka PM, Eissa N, Bernstein CN, Khafipour E, Ghia JE (2015) Antepartum antibiotic treatment increases offspring susceptibility to experimental colitis: a role of the gut microbiota. PLoS One 10(11): e0142536
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins-Obstetrics (2016) Practice Bulletin No. 172: Premature Rupture of membranes. Obstet Gynecol 128: e165-177
- Kenyon S, Boulvain M, Neilson JP (2013) Antibiotics for preterm rupture of membranes. Cochrane Database Syst Rev 2: CD001058.
- Wojcieszek AM, Stock OM, Flenady V (2014) Antibiotics for prelabour rupture of membranes at or near term. Cochrane Database Syst Rev 10: CD001807
- Saccone G, Berghella V (2015) Antibiotic prophylaxis for term or near-term premature rupture of membranes: metaanalysis of randomized trials. Am J Obstet Gynecol 212(5): e1-9.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...





