Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Research Article(ISSN: 2637-4544) 
Levonorgestrel Intrauterine System Effects Versus Copper Intrauterine Device on Changing of Menstruation and Uterine Artery Doppler Volume 4 - Issue 2
Nareman Elhamamy*
- Department of Obstetrics and Gynecology, Tanta University, Egypt
Received: February 25, 2020; Published: July 01, 2020
Corresponding author: Nareman Elhamamy, Lecturer of Obstetrics and Gynecology, Faculty of Medicine, Tanta University, Tanta, Egypt
DOI: 10.32474/IGWHC.2020.04.000184
Abstract
Background: The most effective methods for birth control are the long-acting reversible contraceptives LARCs include Paragard IUD in silver, Mirena IUD in hormonal (progesterone) and hormonal contraceptive implant. The intrauterine levonorgestrelreleasing system (LNG‐IUS) and the intrauterine copper unit (Cu‐IUD) influenced changing of menstruation and uterine artery Doppler indices.
Aim of the work: Comparison of the effects of copper intrauterine device (Cu‐IUD) and an intrauterine levonorgestrel releasing system (LNG‐IUS) on changing of menstruation and Doppler indices of uterine arteries.
Methods: This was RCT was completed between February 2017 to January 2020 at the Obstetrics and Gynecology department, Tanta University hospitals. There were two group first group A: LNG‐IUS (N=200) and second group B Cu‐IUD (N=200), they were randomly assigned to 400 multiparous women preferring intrauterine contraception., the UA pulsatility index (PI) and the resistant index (RI) were determined at the beginning, and the associations with irregular bleeding were evaluated three and six months after insertion
Results: In group A: LNG‐ IUS, some women registered irregular bleeding (28 percent) than in the Cu‐IUD group (52 percent) at the beginning of the study (P<0.001). There was bleeding irregularity (73 percent) in the group(A): LNG‐IUS and severe menstrual bleeding (68 percent) in the Cu‐IUD group. The uterine artery PI was associated with bleeding irregularity at value of 1.40, with a curve area (AUC) of 0.91, 90 percent sensitivity, and 100 percent specificity. Uterine artery RI was associated with 0.65 with 0.22 AUC bleeding irregularity, 95 percent sensitivity and accuracy 100 percent.
Conclusion: LNG‐ IUS related irregular bleeding was linked to changes in the blood flow of uterine arteries that were not evident among Cu‐IUD users.
Keywords:Intrauterine devices; LNG-IUS; cu-IUD, Long-acting reversible contraception; ultrasonography; Doppler; Color; Power Doppler
Introduction
Long acting reversible contraceptives (LARCs) are the most
effective methods for regulating birth. LARCs include silver
Paragard IUD, hormonal Mirena IUD (progesterone), and hormonal
implant contraceptive. Such birth control methods can prevent
unwanted pregnancies up to 20 times better than birth control pills,
patches and vaginal rings [1].
The intrauterine levonorgestrel releasing system (LNG-IUS) has
demonstrated its effectiveness both as a long acting contraceptive
and for its non-contraceptive advantages, including high efficacy
in the treatment of severe menstrual bleeding. However, twentytwo
and sixty seven percent of women had persistent or repeated
bleeding in the first months after placement, which decreased by
first year ending [2].
On the other hand, was associated with an increase of 30%
to 50% in menstrual blood loss and about 10% to 20% in users
requesting withdrawal by first year ending of use [3]. While some
studies have indicated that the LNG‐IUS raises the Doppler UA index three months after use due to an increased blood flow impedance in
the uterine arteries, [4-5] Others found no changes in the Pulsatility
Index (PI) or Resistance Index (RI) of the uterine artery between
LNG‐IUS users three months after insertion [6-7]. Similarly, studies
of the indices of uterine artery Doppler reported contradictory
results to identify the association between use of Cu‐IUD and heavy
menstrual bleeding [8-9].
Knowing changes in the uterine vasculature among IUD users
is important both in terms of physiological and pathophysiological
changes to help inform women about their contraceptive choices
[5]. The purpose of this study was to assess the impact of LNG‐IUS
versus Cu‐IUD on menstrual changes and Doppler uterine artery
indices 3 and 6 months after use.
Materials and Methods
The latest randomized clinical trial among new users of IUD was
performed between January 2017 to August 2019 at the Obstetrics
and Gynecology department, Tanta University hospitals. The study
procedure had been accepted by the ethical review committee of
the Faculty of Medicine, Tanta University.
The study included multiparous women attending a normal
menstrual cycle at the family planning clinic who requested
long acting reversible contraception and met the intrauterine
contraception criteria after providing a complete history and
undergoing clinical examination and transvaginal ultrasonography.
Criteria is omitted: Nulliparity, pregnancy, previous month’s genital
infection, undiagnosed uterine bleeding, medical conditions and
any contraindications to progestin administration or IUD insertion.
Participants were assigned to one of two classes by using computergenerated
simple random tables. Women received group 1 LNG‐IUS
(Mirena, Bayer HealthCare, Berlin, Germany); women received
group 2 copper T‐380 IUD (Copper IUD, DPK, Egypt). Blinding
was not done due to the clear distinction between the two forms
of IUDs. Uterine artery Doppler was conducted in the Department
of Radiology with a 7-MHz transvaginal probe and an EUB‐7000
ultrasound instrument (Hitachi, Tokyo, Japan) prior to insertion of
the contraceptive tool, and three and six months after insertion. For
avoiding interobserver volatility.
The primary outcome measures were menstrual changes and
improvements in the three- and six-months following application of
uterine artery Doppler indices. In order to evaluate the correlation
between uterine artery Doppler indices and subsequent regular
or serious menstrual bleeding, a regression analysis included
all women affected by an excessive bleeding at the three-and sixmonths
follow-up. The secondary results were side effects, and
female satisfactoriness.
Women were given calendars of menstruation to chart the days
they suffered bleeding the WHO suggested. The menstrual segment
included both a bleeding episode, and a bleeding-free cycle.
Vaginal spotting was defined as very slight bleeding which did not
require sanitary protection, while heavy bleeding was defined as
hemorrhage which required sanitation. Analysis on side effects
was done with appropriate managing of stated symptoms at each
scheduled visit.
Statistical analysis
Data entry, processing and statistical analysis was carried
out using MedCalc ver. 18.2.1 (MedCalc, Ostend, Belgium). Tests
of significance (Kruskal-Wallis, Wilcoxon’s, Chi square, logistic
regression analysis, and Spearman’s correlation) were used.
Data were presented and suitable analysis was done according
to the type of data (parametric and non-parametric) obtained for
each variable. P-values less than 0.05 (5%) was considered to be
statistically significant.
To evaluate predictors of bleeding irregularity, multiple logistic
regression was used. The feature of the receiver operator (ROC)
curve analysis was used to determine the optimal cutoff value
and sensitivity, and PI and RI specificity to predict bleeding. A P
value less than 0.05 has been found statistically significant. The
confidence interval was set at 95% and the accepted error margin
was set at 5%. So, at the level of < 0.05, the p-value was considered
significant.
Results
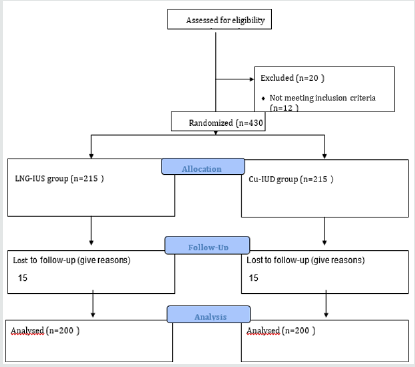
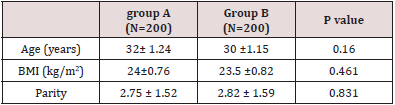
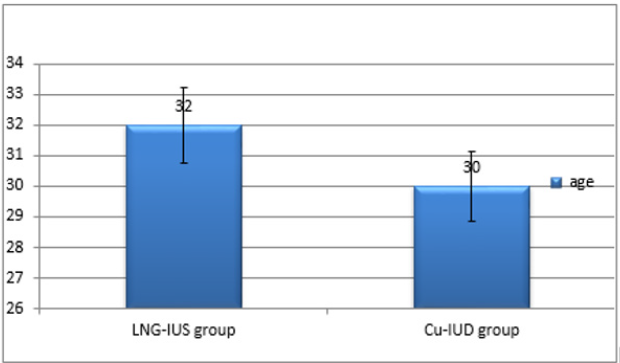
Overall, 450 females met the study criteria and were employed into the clinical trial. Of these, the 6-month follow-up study was attended and completed by 400 women (LNG‐IUS group, n=200; Cu‐IUD group, n=200) (Figure 1 & Table 1).
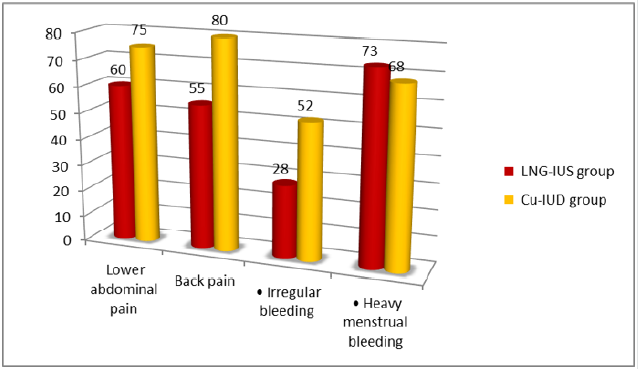
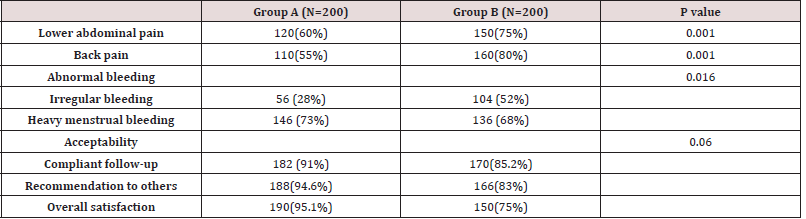
Figure 2 & Table 2 showing that there was high statistically significant difference between two groups regarding side effects and acceptability of females two wards the contraceptive methods (P<0.001). at the beginning of the study, In LNG‐IUS group fewer females had irregular bleeding (28 percent) than in the Cu‐IUD group (52 percent). The bleeding was primarily in the form of irregular bleeding (73 percent) in the LNG‐IUS community and extreme menstrual bleeding (68 percent) in the Cu‐IUD group among those who had abnormal bleeding. The number of women experiencing irregular bleeding was down at six months in both groups. Also, there was high statistically significant difference between two groups regarding overall satisfaction (p<0.05) (Figure 3 Table 3).
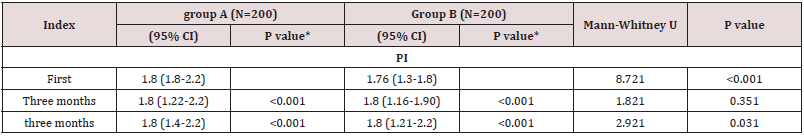
Table 4 showing that there were significantly different regarding
the first PI (P<0.001) and RI (P<0.001) were of which were higher
among women in the LNG‐IU group. Also, both groups at three and
six months, that there were significantly different regarding PI and
RI with the first Doppler indices (all P<0.001).
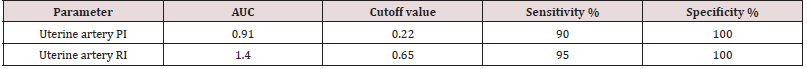
The ROC curve study associated uterine artery PI with irregular
bleeding at a cutoff value of 1.40 with a curve area (AUC) of 0.91,
90 percent sensitivity, and 100 percent accuracy. Uterine artery RI
was associated with 0.65 with 0.22 AUC bleeding irregularity, 95
percent sensitivity& accuracy. 100 percent (Figure 4 & Table 4).
Figure 4: ROC curve analysis of the relationship between pulsatility index (PI) and resistance index (RI) of an irregular bleeding and uterine arteries.
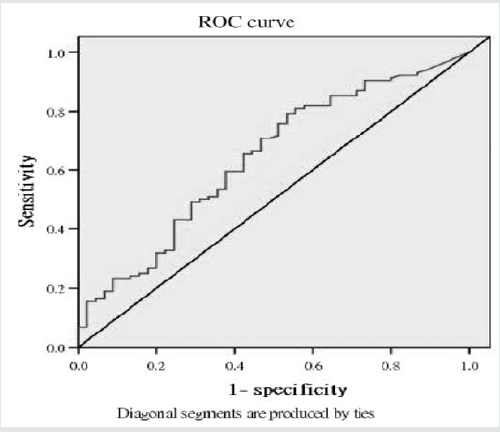
Table 4: Comparison between the studied groups regarding Uterine artery resistance index by study group.
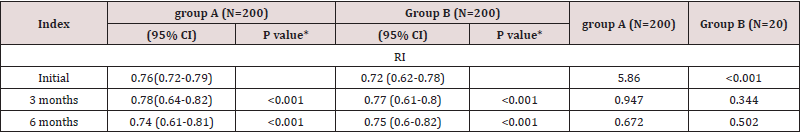
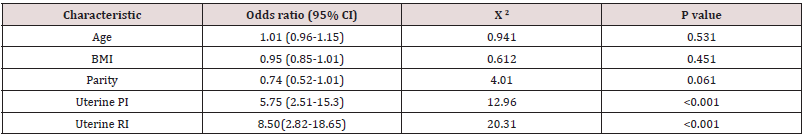
Table 5 showing that Multiple logistic regression analysis of bleeding abnormality and female features shown a significant correlation between uterine artery PI and RI at baseline (P<0.001).
Discussion
Long acting reversible contraception (LARC) methods such
as intrauterine levonorgestrel releasing (LNGIUS) are safe and
highly effective in preventing pregnancy. Previous studies had
been done Doppler indices of the uterine artery and correlate
with menstrual abnormalities reported conflicting results [4-6].
Women that use LNG-IUS will experience excessive or unusual
bleeding in the first months following placement, as reported by
22% and 67% of users, respectively, and this abnormal bleeding
will decrease by the end of the first year [2]. As expected, in this
study, women using LNG-IUS reported lower rates of menstrual
disorders and greater acceptability compared to cu-IUD, which
could be largely attributed to menstrual irregularities and fear
of declining future fertility. Women using LNG-IUS experienced
greater acceptability in terms of overall satisfaction (p<0.001) and
method recommendation to other women (p<0.05). In the current
study, excessive uterine bleeding has been shown to be positively
associated with hemodynamic changes in the uterine artery, with
a significant decline in PI and RI among new users of LNG‐IUS but
not Cu‐IUD.
Jiménez et al. [5] LNG‐IUS first recorded positive effect on
uterine artery PI. It was found that LNG‐IUS was independently
associated with increased uterine artery PI among 27 women after
age and parity control, whereas in a study evaluating PI just before
mid-luteal insertion and three months after insertion there was
no difference among 25 women receiving TCU 380A IUD. Recently,
more so. Similarly, Järvelä et al. [4] Who in 13 postmenopausal
symptomatic women who obtained transdermal estradiol 1 month
before combining LNG‐IUS with replacement estrogen therapy
measured uterine PI. The same group subsequently stated in a
study of 27 healthy, regularly menstruating women that LNG‐IUS
injection in the mid-luteal phase in combination with serum LNG
and associated decrease in serum progesterone tended to increase
impedance to the uterine arterial blood flow Another longitudinal
study Conducted by Bastianelli et al. [6] concluded that LNG‐IUS
not only altered endometrial thickness but also significantly altered
uterine blood flow among women with excessive bleeding, Zalel et
al. [10] After insertion of LNG‐IUS in 47 women and insertion of Cu‐
IUD in 35 women, no changes in blood flow in the uterine artery were
identified when measured prior to and after use. Dane et al. [11]
Reduced sub endometrial vascularization and higher spiral artery
uterine PI among 25 new users of Depo-medroxyprogesterone
acetate injection but no improvements among 25 new LNG‐IUS
users.
More recently, Cihangir et al. [7] reported that there was no
significant change in the volume of ovaries or uterine RI and PI at
6 or 12 months with respect to the pre-insertion values among 49
users of LNG‐IUS. Regarding the Cu‐IUD, recent studies identified a
lack of significant changes in the uterine artery’s PI and RI with or
without side effects, including dysmenorrhea, heavy menstruation
and dyspareunia, 3 or 6 months after insert. [5,9-12] high menstrual
bleeding associated with the Cu‐IUD could be due to the mediated
development of vasoactive agents other than prostaglandins in
the surrounding tissue [13]. The differences among the above studies may be due to the small sample sizes, or the measurement
of Doppler indices at specific menstrual cycle periods or times
of the day, or by various ultra-sonographers. Such contradictory
variables had been omitted in the current study. Indeed, the design
of the study and the greater number of participants form the main
strengths of the study [14]. Regarding the study’s weaknesses. no
extension of the duration of follow-up or comparison of other longacting
contraceptive methods was needed.
Conclusion
In conclusion, LNG‐IUS-related irregular bleeding was linked to changes in blood flow to the uterine artery that were not apparent among Cu‐IUD users. Uterine artery Doppler is an easy, affordable, and readily available method for diagnosing women with irregular uterine bleeding after insertion of the LNG‐IUS for contraception. Future research will focus among new users of Cu‐IUD on the predictive value of Doppler indices on the uterine artery and subsequent heavy menstruation.
References
- Winner B, Peipert JF, Zhao Q (2012) Effectiveness of long-acting reversible N Engl J Med 366:1998-2007.
- Suvisaari J, Lähteenmäki P (1996) Detailed analysis of menstrual bleeding patterns after postmenstrual and postabortal insertion of a copper IUD or a levonorgestrel-releasing intrauterine system. Contraception 54(4): 201-208.
- Momtaz M, Zayed M, Rashid K, Idriss O (1994) Doppler study of the uterine artery in patients using an intrauterine contraceptive device. Ultrasound Obstet Gynecol 4(3): 231-234.
- Järvelä I, Raudaskoski T, Tekay A, Jouppila P (1997) Effect of the levonorgestrel-releasing intrauterine system on the uterine artery pulsatility index in postmenopausal hormone replacement therapy. Ultrasound Obstet Gynecol 10(5): 350-355.
- Jiménez MF, Vetori D, Fagundes PA, de Freitas FM, Cunha-Filho JS (2008) Subendometrial microvascularization and uterine artery blood flow in IUD-induced side effects (levonorgestrel intrauterine system and copper intrauterine device). Contraception 78(4): 324-327.
- Bastianelli C, Farris M, Rapiti S, Vecchio RB, Benagiano G (2014) Different bleeding patterns with the use of levonorgestrel intrauterine system: Are they associated with changes in uterine artery blood flow? Biomed Res Int.
- Cihangir U, Ebru A, Murat E, Levent Y (2013) Mechanism of action of the levonorgestrel-releasing intrauterine system in the treatment of heavy menstrual Int J Gynecol Obstet 123(2): 146-149.
- Hurskainen R, Teperi J, Paavonen J, Cacciatore B (1999) Menorrhagia and uterine artery blood Hum Reprod 14(1): 186-189.
- De Souza MA, Geber S (2006) Doppler color flow analysis of the uterine arteries before and after intrauterine device insertion: A prospective study J Ultrasound Med 25(2): 153-157.
- Zalel Y, Shulman A, Lidor A, Achiron R, Mashiach S, et al. (2002) The local progestational effect of the levonorgestrel-releasing intrauterine system: A sonographic and Doppler flow study. Hum Reprod 17: 2878-2880.
- Dane B, Akca A, Dane C, Evcimen S, Cetin A (2009) Comparison of the effects of the levonorgestrel-releasing intrauterine system (Mirena) and depot-medroxyprogesterone acetate (Depo-Provera) on suben- dometrial microvascularisation and uterine artery blood flow. Eur J Contracept Reprod Health Care 14: 240-244.
- Mutlu I, Demir A, Mutlu MF (2014) Can uterine artery Doppler parameters predict copper intrauterine device-induced side effects? Eur J Contracept Reprod Health Care 19(1): 51-56.
- Järvelä I, Tekay A, Jouppila (1998) The effect of diclofenac on uterine artery blood flow resistance during menstruation in patients with and without a copper intrauterine device. Hum Reprod 13(9): 2480-2483.
- Parks C, Peipert JF (2016) Eliminating health disparities in unintended pregnancy with long-acting reversible contraception (LARC). Am J Obstet Gynecol 214(6): 681-688.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...