Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Research Article(ISSN: 2637-4544) 
Laparoscopic Colpopexy is it an Effective Intervention for Urinary Incontinence Associated with Female Pelvic Organ Prolapse? Volume 3 - Issue 2
Walid Mohamed Elnagar1* and Ibrahem Ismail Samaha2
- 1Department of Obstetrics and Gynecology, Zagazig University, Egypt
- 2Head of Urodynamic Unit, Zagazig University, Egypt
Received:May 12, 2019; Published: May 22, 2019
Corresponding author: Walid Mohamed Elnagar, Department of Obstetrics and Gynecology, Zagazig University, Egypt
DOI: 10.32474/IGWHC.2019.03.000159
Abstract
Background: Pelvic organ prolapse is a distortion in normal anatomical correlations and integrity resulting in chronic distressing symptoms. Laparoscopic sacrocolpopexy is a frequently performed mesh-based surgical procedure for severe forms of pelvic organ prolapse having a high cure rate. Functional clinical outcomes evaluation after repair of pelvic prolapse is one of the cornerstone issues that determines the quality of health care service implemented. Aim: To investigate and evaluate the functional clinical outcomes of conducting laparoscopic sacrocolpopexy by comparing and contrasting preoperative and postoperative urodynamic testing in cases clinically classified to have stages II to IV pelvic organ prolapse.
Methodology: A prospective research study conducted on 48 research study subjects from January 2016 till February 2018 undergoing laparoscopic sacrocolpopexy due to stage II–IV pelvic organ prolapse.
Results: urodynamic indices pre and post-operative in which as regards there was statistically significant difference regarding uroflowmetric indices, Qmax (maximum urinary flow), Elevated PVR (p value<0.001,0.001 consecutively ) as regards cystometric indices there was statistically significant difference between pre and post-operative findings concerning, low bladder compliance , involuntary detrusor contractions, detrusor muscle pressure, involuntary detrusor contractions, positive Valsalva (vesical) leakpoint pressure, (p values =0.016,0.001, <0.001 and 0.016 consecutively) although there was no statistical significant difference concerning maximum cystometric capacity, Abdominal VLPP positive(p value=0.098,0.617 consecutively. As regards pressure flow study indices there was statistical significant difference between pre and post-operative readings as regards Qmax, PVR, mean +/- SD Opening pressure , mean +/-SD Pdet Qmax (detrusor pressure at maximum flow), Median (IQR) of Time to maximum flow, Voiding time, Urogenital Distress Inventory, BOO bladder outlet obstruction, (p values<0.001 ,0.001) Whereas projected isovolumetric pressure <35 wasn’t statistically significant pre and post-operative (p value=0.063).
Conclusion and recommendations: Laparoscopic sacrocolopexy when properly performed on required cases results in marked improvement of most urodynamic indices. Future research efforts should be conducted in a multicentric manner to evaluate the effectiveness of this mode of management on long term.
Keywords: Pelvic organ; Laparoscopic sacrocolpopexy; Urogynecological; Peritoneum
Introduction
Pelvic organ prolapse is a distortion in normal anatomical correlations and integrity resulting in chronic distressing symptoms that could be severe to affect the quality of life particularly in advanced stages [1-3].
Irritative or storage voiding symptoms or urinary incontinence could result from this anatomically altered clinical scenario frequently presented in every day gynecological practice particularly among post-menopausal women sometimes urinary incontinence is masked due to change within the urethral angle resulting from obstructive impact of pelvic organs prolapsed [4-6].
The chief presenting symptom for pelvic organ prolapse is urinary stress incontinence and various issue correlated to distortion of normal anatomical support of the urinary system crucial for normal functioning resulting in repeated urinary tract infections and overactive bladder symptoms that cause social embarrassment of cases affected [7-9].
Prolapse surgical repair procedures result in improvement of voiding functions however sometimes new symptoms arise from the procedure itself or recurrence that is common particularly when predisposing factors are not corrected [10,11].
Functional clinical outcomes evaluation after repair of pelvic prolapse is one of the cornerstone issues that determines the quality of health care service implemented in urogynecological practice [12,13].
Researchers recently have increased interest in enhancing quality of life in that category of cases not only by proper choice and technique of operative intervention but in addition by close follow up of those patients that would improve the long-term outcomes [14-16].
Laparoscopic sacrocolpopexy is a frequently performed mesh-based surgical procedure for severe forms of pelvic organ prolapse having a high cure rate with limited number of operative complications reported [17-19].
Aim of the work
To investigate and evaluate the functional clinical outcomes of conducting laparoscopic sacrocolpopexy by comparing and contrasting pre-operative and post-operative urodynamic testing in cases clinically classified to have stages II to IV pelvic organ prolapse.
Methodology
A prospective research study conducted on 48 research study subjects from January 2016 till February 2018 undergoing laparoscopic sacrocolpopexy inclusive research criteria stage II–IV pelvic organ prolapse classified according to the Pelvic Organ Prolapse Quantification system, cases preferring to preserving their uteri after exclusion of any uterine pathology clinically by sonographic examination and not requiring concomitant incontinence procedures. Exclusive research criteria are cases that require incontinence procedures e.g. TVT, TOT, cases that have undergone hysterectomy. All recruited subjects have undergone full assessment for clinical functional outcomes by pre- and postoperative urodynamic investigations.
Full relevant clinical medical history, examination, multichannel urodynamics, was conducted for all recruited cases.
Cases had clinical follow up at 1, 3, 6, and 12 months consecutively after performance of the operative procedure. After surgery by 6 months, all cases performed a urodynamic re- assessment and filled an assessment questionnaire.
Surgical intervention
Four trocars were used for the laparoscopic procedure as follows: a sub umbilical 12-mm trocar for the 0° scope, a 10-mm trocar medial to the superior–anterior iliac spine, another 5-mm trocar medial to the superior–anterior iliac spine on the other side, and a 5-mm trocar midway between the umbilicus and symphysis. A polypropylene mesh rectangular in shape have been fixed to the anterior wall of the vagina using four sutures (polyglycolic 1-0) after bladder dissection till the bladder neck. An additional rectangular polypropylene mesh has been fixed to the posterior aspect of the vagina by using four sutures (polyglycolic 1–0) after surgical dissection downwards till reaching the levator ani tissue plane the retroperitoneum was opened using monopolar diathermy from sacral promontory to vault. The mesh size has been accustomed to suit the patient. Both meshes have been fixed by one or two non-absorbable sutures (2.0 prolene) to presacral ligament in the promontory with an undue tension. Another option is to use self-tailored H shaped mesh. The peritoneum is closed over the mesh to prevent any bowel entrapment. No associated surgical intervention for anti-incontinence was conducted.
Urodynamic assessment
Cystometry, the bladder was filled with room-temperature saline solution at 50ml/min with the patient in a supine position. No prolapse reduction was performed during evaluation. Detrusor over activity have been clinically defined as involuntary detrusor contractions During cystometry filling phase, spontaneous, provoked, phasic or terminal, revealing a cystometrogram wave form variable in both duration and amplitude. Bladder outlet obstruction was observed according Defreitas Nomogram [maximum flow at uroflowmetry ≤12ml/s and a detrusor pressure at maximum flow phase throughout pressure-flow study ≥25cm H2O]. All urodynamic investigations were conducted by a consultant specialized uro- gynecologist. Bladder compliance calculated by division of the change in volume by detrusor pressure changes. Two typical indices have been used the beginning of filling and cystometric capacity.
Statistical analysis
Data were collected, revised, coded and entered to the Statistical Package for Social Science (IBM SPSS) version 23. The quantitative data were presented as mean, standard deviations and ranges when parametric and median with inter-quartile range (IQR) when non-parametric and percentiles was used to assess the distribution of some parameters. Also paired groups regarding qualitative variables were done by using McNemar test while with quantitative parameters were done using paired t-test when parametric and Wilcoxon rank test when non-parametric. The confidence interval was set to 95% and the margin of error accepted was set to 5%. So, the p-value was considered significant at the level of < 0.05.
Results
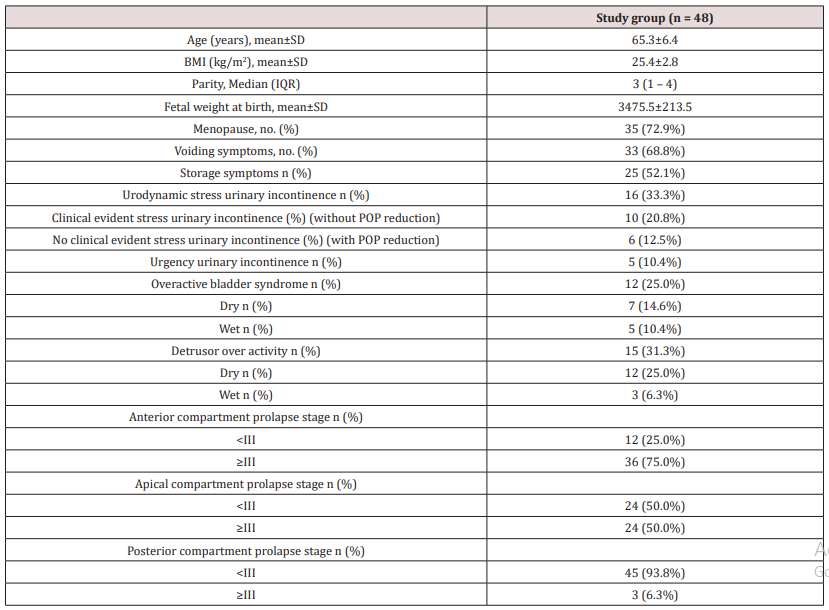
(Table 1) reveals and displays the demographic and basic clinical features of the research study cohort in which mean /SD of age, BMI, fetal weight at birth =65.3±6.4 years , 25.4±2.8kg/m2, , 3475.5 ± 213.5 grams, whereas parity median (IQR)= 3 (1 – 4),35 cases were menopausal representing 72.9% of the research study cohort ,33 cases had voiding symptoms representing 68.8% of the research study cohort ,storage symptoms was present in 25 cases(52.1%),16 cases had Urodynamic stress urinary incontinence (33.3%), Clinical evident stress urinary incontinence without POP reduction was present in 10 cases (20.8%), No clinical evident stress urinary incontinence with POP reduction was present in 6 cases (12.5%),5 cases had Urgency urinary incontinence (10.4%),12 cases had Overactive bladder syndrome (25.0%) 7 of them were dry and 5 were wet ,15 cases had detrusor over activity (31.3%) 12 cases were dry and 3 cases were wet , Anterior compartment prolapse stage <III was present in 12 cases(25.0%) whereas stage ≥III was present in 36 cases (75%), Apical compartment prolapse stage <III was present in 24 cases (50%),whereas stage ≥III was present in 24 cases also(50%), Posterior compartment prolapse stage <III was present in 45 cases (93.3%),whilst stage ≥III existed in 3 cases only (6.3%).
(Table 2) reveals and displays the urodynamic indices pre and post-operative in which as regards there was statistically significant difference concerning Uroflowmetry indices, Qmax, Elevated PVR (p value<0.001,0.001 consecutively ) as regards Cystometry indices there was statistically significant difference between pre and post-operative findings concerning, Low bladder compliance, involuntary detrusor contractions, Detrusor pressure, involuntary detrusor contractions, Positive Valsalva (vesical) leak-point pressure, (p values =0.016,0.001,<0.001 and 0.016 consecutively )Whereas there was no statistical significant difference as regards Maximum cystometric capacity , Abdominal VLPP positive(p value=0.098,0.617 consecutively. As regards pressure flow study indices there was statistical significant difference between pre and post-operative readings as regards Qmax (maximum urinary flow rate, PVR (post voidal residual urine), mean +/-SD Opening pressure, mean +/-SD Pdet Qmax detrusor pressure at maximum flow, Median (IQR) of Time to maximum flow, Voiding time, Urogenital Distress Inventory, BOO bladder outlet obstruction,(p values <0.001, 0.001) Whereas projected isovolumetric pressure <35 wasn’t statistically significant pre and post-operative (p value=0.063).
Table 2: Urodynamic findings pre and post-operative among research study cohort.

Q max maximum flow, PVR post void residual, PVR >30% of voided volume, IDC involuntary detrusor contractions, VLPP Valsalva (vesical) leak-point pressure, P det max detrusor maximum pressure, Pdet Qmax detrusor pressure at maximum flow, PIP projected isovolumetric pressure, BOO bladder outlet obstruction, UDI Urogenital Distress Inventory
*McNemar test
*: Paired t-test
Discussion
Urodynamic evaluation in uro-gynecologic corrective procedures is a challenging issue due to complexity of functional components of voiding processes. Anatomical correlations regained by surgical interventions is the cornerstone aim of all urogynecologists trying to achieve the best short and long term functional out comes however some components of micturition function could be still affected and clinical follow up in a systematic manner would enhance the quality of life of those cases [20-22].
Complexities arise also due to frequent comorbid clinical scenarios such as DM and hypertension making management protocols for those cases best achieved by multidisciplinary approach [23,24].
The lack appropriate cutoff values for uroflowmetry indices is considered a research challenge when Investigating voiding functions in females having pelvic organ prolapse issues [25,26].
Prior research groups of investigators have revealed that the voiding dysfunction within prolapse patients have a statistically estimated range of 12.8% to 39% in addition a prior research study similar to the current research in approach and methodology have shown that voiding dysfunction rate among cases having pelvic organ prolapse was about 39% whereas another prior research team of investigators mentioned a rate of 29.25%, 67 of 229 cases having clinical symptoms of lower urinary tract. Functional various facts and issues could elucidate the cause for the high incidence observed in some prior research studies such as postmenopausal state severe forms pelvic organ prolapse , besides it was interestingly observed by experienced uro-gynecologists that anterior vaginal wall prolapse cases are more liable to suffer voiding functional disorders due to urethral compression by prolapsed pelvic organs [27,28].
Prior researchers have observed and displayed among their research study findings that around 78% of preoperative voiding dysfunction could be resolved after abdominal sacrocolpopexy, and newly developed voiding disorders developed in 3% of patients another group of investigators have revealed and displayed that around 28% of cases suffering pelvic organ prolapse had preoperative voiding dysfunction, and 10% had persistent voiding dysfunction issues postoperatively [1,3,9].
Additionally, in an interesting fashion a prior research team of investigators have revealed and observed among their research study findings that around 89% of cases with severe forms of Pelvic organ prolapse and raised post voiding residual urine indices had normalization of PVR after POP surgical corrective procedures. Similar to the current research study consecutive urodynamic evaluation before and after laparoscopic sacrocolpopexy research findings and results revealed that bladder volume indices at first sense of desire to void was statistically significantly raised and that maximal detrusor pressure during voiding have been statistically significantly reduced. Besides, it was observed that there were no unfavorable urodynamic results after laparoscopic sacrocolopopexy. Interestingly those research findings show great similarity and harmony with the current research study findings [4,10,15].
A prior prospective research study recruited Forty-nine cases that have undergone a modified laparoscopic sacrocolpopexy/hysteropexy procedure. The investigators aimed to investigate the impact of surgical intervention on pelvic anatomy, urodynamic observations, cases satisfaction and symptom scoring levels. The research team of investigators revealed and displayed the following results in which they observed that Laparoscopic sacrocolpopexy corrected successfully vaginal vault prolapse. In all cases assessed by urodynamics workup six months after the procedure in which the bladder volume during start of voiding desire had statistically significantly increased and the maximal detrusor pressure at voiding phase have been statistically significantly reduced. Furthermore, the irritative and storage voiding complains have been reduced in a considerable manner showing statistical significance [17-22].
Another priorly conducted research studies assessed and evaluated the voiding functional changes at 3 months after performance of laparoscopic sacrocolpopexy. They came to the conclusion that preoperative voiding dysfunction is powerfully correlated and linked to pelvic organ prolapses and considerably improves in a statistically significant fashion at 3 months after performance of laparoscopic sacro- colopopexy [19,24,28].
The current research study findings that have shown great improvement in urodynamic findings could be justified by the fact that the sacrocolpexy procedure improves the anatomical pelvic structural positioning and support therefore enhances the urinary continence function.
Conclusion and Recommendations
Laparoscopic sacrocolopexy when properly performed on required cases results in marked improvement of most urodynamic indices and parameters ,however future research efforts should be conducted in a multicentric manner to evaluate the effectiveness of this mode of management on long term .Racial ,ethnic and anatomical variations in the presentation of the pelvic organ prolapse should be put in consideration in efforts of future research to aid in enhancement and improvement of urodynamic practice and health care requirement for those category of cases.
References
- Costantini E, Lazzeri M, Bini V, Del Zingaro M, Frumenzio E, et al. (2012) Pelvic organ prolapse repair with and without concomitant Burch colposuspension in incontinent women: a randomized controlled trial with at least 5-year follow- up. Obstet Gynecol Int: 967923.
- Serati M, Giarenis J, Meschia M, Cardozo L (2015) Role of urodynamics before prolapse surgery. Int Urogynecol J 26(2): 165-166.
- Hwang SM, de Toledo LGM, da Silva Carramão S, Frade AB, Matos AC, et al. (2018) Is urodynamics necessary to identify occult stress urinary incontinence? World J Urol 37(1): 189-193.
- Abrams P, Cardozo L, Wagg A (2016) International Consultation on Incontinence ICUD/ICS.
- De Boer TA, Salvatore S, Cardozo L, Chapple C, Kelleher C, et al. (2010) Pelvic organ prolapse and overactive bladder. Neurourol Urodyn 29(1): 30-39.
- Haylen BT, Maher CF, Barber MD, Camargo S, Dandolu V, et al. (2016) An International Urogynecological Association (IUGA)/International Continence Society (ICS) Joint Report on the Terminology for Female Pelvic Organ Prolapse (POP). Neurourol Urodynam 35: 137-68.
- Costantini E, Mearini L, Lazzeri M, Bini V, Nunzi E, et al. (2016) Laparoscopic versus abdominal Sacrocolpopexy: a randomized, controlled trial. J Urol 196(1): 159-165.
- Illiano E, Giannitsas K, Zucchi A, Di Biase M, Del Zingaro M, et al. (2016) Sacro colpopexy for post hysterectomy vaginal vault prolapse: long-term follow-up. Int Urogynecol J 27(10): 1563-1569.
- Rosier PFWM, SchaeferW, Lose G, Goldman HB, Guralnick M et al. (2016) International continence society good urodynamic practices and terms 2016: Urodynamics, uroflowmetry, cystometry, and pressure-flow study. Neurourol Urodynam 1-18.
- Fletcher SG, Haverkorn RM, Yan J, Lee JJ, Zimmern PE, et al. (2010) Demographic and urodynamic factors associated with persistent OAB after anterior compartment prolapse repair. Neurourol Urodyn 29(8): 1414-1448.
- Kummeling MT, Rietbergen JB, Withagen MI, Mannaerts GH, van der Weiden RM (2013) Sequential urodynamic assessment before and after laparoscopic sacro colpopexy. Acta Obstet Gynecol Scand 92(2): 172-177.
- Kanasaki H, Oride A, Mitsuo T, Miyazaki K (2014) Occurrence of pre and postoperative stress urinary incontinence in 105 patients who underwent tension-free vaginal mesh surgery for pelvic organ prolapse: a retrospective study. ISRN Obstet Gynecol: 643495.
- El Hamamsy D, Fayyad AM (2015) New onset stress urinary incontinence following laparoscopic sacrocolpopexy and its relation to anatomical outcomes. Int Urogynecol J 26(7): 1041-1045.
- Abdullah B, Nomura J, Moriyama S, Huang T, Tokiwa S, et al. (2017) Clinical and urodynamic assessment in patients with pelvic organ prolapse before and after laparoscopic sacrocolpopexy. Int Urogynecol J 28(10): 1543- 1549.
- Costantini E, Lazzeri M, Zucchi A, Mearini L, Fragalà E, et al. (2013) Urgency, detrusor overactivity and posterior vault prolapse in women who underwent pelvic organ prolapse repair. Urol Int 90(2): 168-173.
- Gabriel B, Nassif J, Barata S, Wattiez A (2011) Twenty years of laparoscopic sacrocolpopexy: where are we now? Int Urogynecol J Pelvic Floor Dysfunct 22: 1165-1169.
- Kummeling MTM, Rietbergen JBW, Withagen MIJ, Mannaerts GHH, van der Weiden RMF (2013) Sequential urodynamic assessment before and after laparoscopic sacrocolpopexy. Acta Obstet Gynecol Scand 92: 172-177.
- Wu JM, Vaughan CP, Goode PS, Redden DT, Burgio KL, et al. (2014) Prevalence and trends of symptomatic pelvic floor disorders in U.S. women. Obstet Gynecol 123(1): 141-148.
- Maher C, Feiner B, Baessler K, Schmid C (2013) Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev 30(4): CD004014.
- Van der Schans EM, Paulides TJC, Wijffels NA, Consten ECJ (2018) Management of patients with rectal prolapse: the 2017 Dutch guidelines. Tech Coloproctol 22(8): 589-596.
- Van Iersel JJ, de Witte CJ, Verheijen PM, Broeders IA, Lenters E, et al. (2016) Robotassisted sacro colpo rectopexy for multi compartment prolapse of the pelvic floor: a prospective cohort study evaluating functional and sexual outcome. Dis Colon Rectum 59(10): 968-974.
- Reddy J, Ridgeway B, Gurland B (2011) Robotic sacro colpo perineopexy with ventral rectopexy for the combined treatment of rectal and pelvic organ prolapse: initial report and technique. J Robot Surg 5(3): 167-173.
- Choi YS, Kim JC, Lee KS, Seo JT, Kim HJ, et al. (2013) Analysis of female voiding dysfunction: a prospective, multi-center study. Int Urol Nephrol 45(4): 989-994.
- Costantini E, Mearini L, Lazzeri M, Bini V, Nunzi E, et al. (2016) Laparoscopic versus abdominal Sacrocolpopexy: a randomized, Controlled Trial. The Journal of urology 196(1): 159-165.
- Zhu L, Sun Z, Yu M, Li B, Li X, et al. (2013) Modified laparoscopic sacrocolpopexy with mesh for severe pelvic organ prolapse. Int J Gynaecol Obstet 121(2): 170-172.
- Haylen BT, Maher CF, Barber MD, Camargo S, Dandolu V, et al. (2016) An international Urogynecological Association (IUGA) / international continence society (ICS) joint report on the terminology for female pelvic organ prolapse (POP). Int Urogynecol J 27(2): 165-194.
- Casteleijn NF, Panman CM, Wiegersma M, Kollen BJ, Messelink EJ, et al. (2015) Free uroflowmetry for voiding dysfunction measurement in women with pelvic organ prolapse and urinary incontinence in primary care. Int J Urol 22(8): 801-802.
- Lo TS, Shailaja N, Hsieh WC, Uy-Patrimonio MC, Yusoff FM, et al. (2016) Predictors of voiding dysfunction following extensive vaginal pelvic reconstructive surgery. International urogynecology journal 28(4): 575-582.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...