
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Research Article(ISSN: 2637-4544) 
Intrapartum Analysis of Lower Segment Cesarean Section Undertaken for Clinically Diagnosed Foetal Distress Volume 1 - Issue 3
Nupur Hooja, Premlata Mital*, Nidhi Sharma, Smriti Bhargava, Bhomraj Kumawat, Manisha Kala, Surabhi Arora and Kritika Tulani
- Department of Obstetrics and Gynaecology, Rajasthan University of Health Sciences, India
Received: February 01, 2018; Published: February 12, 2018
Corresponding author: Premlata Mital, Department of Obstetrics and Gynaecology, Rajasthan University of Health Sciences, A-29, Lal Bahadur Nagar, Girdhar Marg, Malviya Nagar, Jaipur, 302017, India
DOI: 10.32474/IGWHC.2018.01.000115
Abstract
Abstract: Clinically diagnosed foetal distress (non reassuring foetal heart rate, meconium stained liquor, altered foetal movement) is one of the leading cause of cesarean section. This study was done for evaluation and correlation of intraoperative condition and neonatal status associated with clinically diagnosed foetal distress.
Methodology: It was a hospital based observational study done in tertiary care hospital in women with clinically diagnosed foetal distress - non reassuring foetal heart rate, meconium stained liquor, altered foetal movement were included in study a details history was taken and intraoperative factors- Liquor (amount and colour), Placenta, Cord were noted. Detailed record of neonatal status was recorded. All data was collected and analyzed.
Result: Among 139 women with clinically diagnosed foetal distress 51% had not reassuring foetal heart rate, 21.5% had meconium Stained liquor, 27.3% had altered foetal movement. Evaluation showed 9.8% had meconium stained liquor 45% had nuchal cord, 8.4% had abruptio placenta in non reassuring foetal heart rate cases. 31.5% had nuchal cord, 13.1% liquor was absent and in 2.6% liquor was meconium stained in altered foetal movements cases. Nuchal cord was present in 6.6% cases with meconium stained liquor. Apgar score of <7/10 and birth weight <2.5 kg present in 10.7% &23% cases respectively. Average neonatal intensive care unit stay was of 7 days and among them meconium aspiration syndrome were maximum.
Conclusion: Careful evaluation should be done for clinically diagnosed Meconium Stained Liquor, altered foetal movement & nonreassuring foetal heartrate. Over diagnosis of foetal distress & misinterpretation of foetal heartrate increased the hospital burden of cesarean section. This points the need to confirm foetal distress diagnosed clinically with foetal blood acid base study & cardiotocography monitoring if possible or using two parameters for better reliability
Keywords: Altered Foetal Movement; Foetal distress; Meconium Stained Liquor; Non reassuring foetal heart rate; Caesarean section
Abbrevations: FHR: Foetal Heart Rate; NICU: Neonatal Intensive Care Unit
Introduction
Foetal distress is one of the leading cause of cesarean section. Assessment of fetus is by counting of the foetal heart rate (FHR) and checking for the presence of meconium in the liquor and womans daily foetal movement count. Abnormal FHR pattern, especially in the presence of meconium in the liquor, signifies foetal hypoxia and acidosis [1]. The introduction of foetal scalp blood pH estimation and electronic foetal monitoring into labour management has decreased the reliability on clinical methods, however the detection of abnormal FHR or rhythm and meconium staining of liquor still represents the best available indirect evidence of poor foetal oxygenation during labour in resource constrained settings and helps identify significant fetuses with possible early neonatal acidaemia and selecting foetuses that requires expedited delivery and supportive therapy at birth in low resource settings [2].
But, operative delivery for clinical foetal distress show that not all the babies delivered have evidence of antecedent hypoxic insult [3]. False diagnosis results in unnecessary caesarean delivery. In developing countries, caesarean section is still not preferred and is associated with significant maternal morbidity and mortality [4-6]. The compromised neonate is to be weighed against the maternal risk of caesarean delivery
Objective
This study was done for evaluation of the accuracy and correlation of intrapartum factors and neonatal status associated with clinically diagnosed foetal distress indicating caesarean section.
Methodology
It was a hospital based observational study done in tertiary care hospital. Singleton caesarean births indicated by clinically diagnosed foetal distress over a six months period (July to December 2017) were selected for the study. The diagnosis of foetal distress was based on detection of abnormal FHR and/or rhythm (>160 or <110 beat per minute) by intermittent auscultation and/or presence of meconium stained liquor or Altered Foetal Movement. Electronic FHR monitoring, foetal blood gas or pH analysis were not available.
All neonates delivered by caesarean section were attended by a senior resident, paediatrician of the hospital. The Apgar scores were assessed at one and five minutes to assess foetal condition and response to resuscitation measures, respectively. Neonatal compromise was defined as one minute Apgar score < 7.
Detailed history was taken and liquor (amount and colour), placenta, cord were noted. Detailed record of neonatal status was recorded. All data was collected and analyzed.
Results
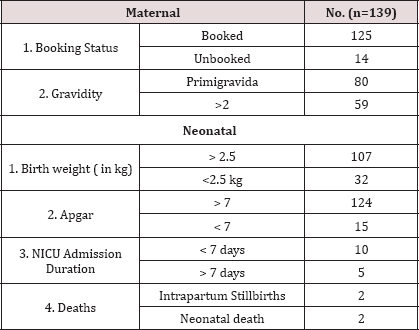
Mean age of the women in our study was 24.6±1.03 years ranging from 20 - 32 years. This may be because of early marriage which is still practiced in our state. (1). 57.7% women in our study were primigravida Table 1.
Table 1: Maternal and Neonatal Characteristics.
Out of 139 women diagnosed clinically as foetal distress, 51.1% had non reassuring FHS, 27.4% had altered foetal movement and 21.5% had meconium stained liquor with normal foetal heart pattern. 71 of 139 women who had non assuring foetal heart pattern, intraoperatively it was observed that 45.1% had nuchal cord, 8.4% had absent or oligohydramnios, 9.9% had meconium stained liquor and in 8.4% cases placenta was small/calcified or separated. 76.9% had birth weight of more than 2.5 kg. 1.4% had intrapartum stillbirth Table 2.
Table 2: Intraoperative Findings Of Clinically Diagnosed Foetal Distress.

Table 3: Correlation of Clinical Foetal distress,Intraoperative Findings with stillbirths / NICU Admissions.
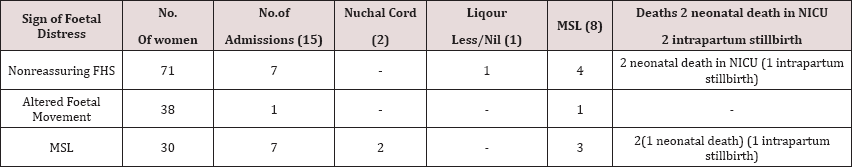
Apgar score was <7 in 10.8% babies in our study. Only 10.7% (15/139) babies required neonatal intensive care unit (NICU) admission. In more than 50%, NICU admission was due to birth asphyxia in neonates associated with meconium passage in utero of all babies requiring NICU admission, 66.7% babies were admitted for a period of 1 to 7 days while 33.3% were admitted for more than 7days in NICU. and 1.4% had early neonatal death. These had either nonreassuring FHR or meconium stained liquor Table 3.
Discussion
This study was done due to the dilemma faced by obstetricians practising in developing countries when faced with clinical evidence of foetal distress that cannot be confirmed by other methods. The results show that 10% ofthe neonates delivered by caesarean section due to clinically diagnosed foetal distress did have suboptimal (< 7) Apgar scores. The relative risk of poor perinatal outcome in terms of foetal acidaemia, low Apgar score, early perinatal morbidity and or mortality in newborns with clinical foetal distress was at least twice that of newborns without foetal distress [7]. Priyadharshini. VM et al 2013 [8] Patil KP et al 2006 [9] and Vijayasree M et al 2014 [10] reported APGAR score <7 in 18.8%, 33% and 30% respectively Vaghela HP et al 2014 [11] had only 5% neonates with APGAR score < 7. This puts some value on clinical diagnosis of foetal distress in low resource setting. However, the number of neonates with mildly decreased or normal Apgar scores at birth also suggests a review of the mode of delivery where the likely risk of caesarean birth to both mother and baby may outweigh its benefits.
Only 10.7% neonates in our study required NICU admission, however in the study done by Kumar BV et al 2015 [12], 35.8% required NICU admission and by Vaghela et al (30%) [11], Vijayasree M et al 2014 [10] (20%) and16% by Uday Rajput, Anu Jain 2013 [13] .Similar to our findings, Our study emphasizes the benefits of combining abnormal FHR with meconium staining of liquor as against singly employing either of the two for intrapartum diagnosis of foetal distress. Reduced amount of liquor along with abnormal foetal heart pattern was also an important marker of distress [12]. In our study, there was poor relation between abnormal FHR alone and immediate neonatal outcome. Use of auscultation of FHR with the stethoscope has many limitations. It cannot assess baseline variability nor can help in diagnosing decelerations with uterine contractions. Foetal tachycardia may be due to maternal fever and anxiety and not foetal acidaemia.
Passage of meconium does not have any hypoxic consequences on the foetus if the FHR is greater than 110 beats per minute. However, meconium staining of liquor together with abnormal FHR and rhythm are still good indicators of foetal jeopardy, which require expedient delivery.7There was reversal of the relationship between meconium liquor alone and severe neonatal compromise only when the consistency of meconium was separately considered [14].
A limitation of the study was the use of Apgar score to assess the neonate as it may not correlate with neonatal acidaemia. Apgar score is not universally accepted as evidence of or consequence of asphyxia. Although a low score may be evidence of hypoxia, the scores may be influenced by factors that affect infant's responsiveness, tone and respiration. Low Apgar score at one minute nevertheless suffices as an excellent indicator of infants in need of resuscitation in a setting where no other method of assessment is available [13].
Conclusion
Since many neonates delivered by caesarean section following clinical diagnosis of foetal distress were severely compromised, careful evaluation should be done for clinically diagnosed meconium stained liquor, altered foetal movement & nonreassuring FHR. These still are of value in identifying foetuses needing expedited delivery in such setting. However, over diagnosis of foetal distress & misinterpretation of foetal heart rate increases the hospital burden of cesarean section besides causing increased maternal morbidity. This points the need either to confirm foetal distress diagnosed clinically with foetal blood acid base study & cardiotocography monitoring. Where not available, combining abnormal FHR with meconium staining of liquor as against either of the two for foetal distress is more reliable.
References
- Van Bogaert LJ, Misra A (2008) Neonatal outcome after caesarean birth for foetal distress and/or meconium staining in a South African rural setting. J Obstet Gynaecol 28(1): 56-59.
- Rotich SK, Ndavi MP, Rukaria Kaumbutho R, Kigondu CS (2006) Early perinatal outcome in cases delivered through Caesarean section following clinical diagnosis of severe foetal distress at Kenyatta National Hospital. East Afr Med J 83(5): 250-258.
- Ikechebelu JI (2004) Accuracy of clinical diagnosis of foetal distress. J Coll Med 9(1): 12-13.
- Ezechi OC, Fasubaa OB, Kalu BE, Nwokoro CA, Obiesie LO (2004) Caesarean delivery: Why the aversion? Trop J Obstet Gynaecol 21(2): 164-167.
- Oladapo OT, Lamina MA, Sule Odu AO (2007) Maternal morbidity and mortality associated with elective caesarean delivery at a university hospital in Nigeria. Aust N Z J Obstet Gynaecol 47: 110-114.
- Ozumba BC, Anya SE (2002) Maternal deaths associated with caesarean section in Enugu, Nigeria. Int J Gynecol Obstet 76(3): 307-309.
- Rotich SK, Ndavi MP, Rukaria Kaumbuthor, Kigondu CS (2006) Early perinatal outcome in cases delivered through Caesarian section following clinical diagnosis of Severe foetal distress at Kenyatta National Hospital East African Medical Journal 83(5).
- Priyadharshini V Meena, Panicker Seetha (2013) Meconium Stained Liquor and Its Foetal Outcome Retrospective Study. IOSR Journal of Dental and Medical Sciences 6(2): 27-31.
- Patil KP, Swamy MK, Samatha K (2006) A one year cross sectional study of management practices of meconium stained amniotic fluid and perinatal outcome. Obstet Gynaecol India 56(2): 128-130.
- M Vijayasree, L Geetha, DVC Shoban Kumar, SGK Murthy, SS Guru Prasad (2014) Study of Maternal and Foetal Outcome in Parturients with Meconium Stained Amniotic Fluid at Term Gestation Role of Intrapartum Amnio Infusion Sch. J App Med Sci 2(2C): 752-756.
- Vaghela HP, Deliwala K, Shah P (2014) Foetal outcome in deliveries with meconium stained liquor. Int J Reprod Contracept Obstet Gynecol 3(4): 909-912.
- Kumar BV, Raj SV, Devi S (2015) Abnormal foetal heart tracing patterns in patients with meconium staining of amniotic fluid and its association with perinatal outcomes. Int J Reprod Contracept Obstet Gynecol 4: 629633.
- Uday Rajput, Anu Jain (2013) Impact of meconium stained amniotic fluid on early neonatal outcome. Journal of Evolution of Medical and Dental Sciences 2(45): 8788-8794.
- Oladapo OT, Sotimehin SA, Ayoola-Sotubo O (2009) Predictors of Severe Neonatal Compromise Following Caesarean Section for Clinically Diagnosed Foetal Distress West African Journal of Medicine 28(5).

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...















