
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Research Article(ISSN: 2637-4544) 
Fertility Predictability Tools for Clinical Outcomes After Myomectomy Procedure for Intramural Fibroids in Cases of Unexplained Infertility Volume 3 - Issue 4
Mohamed Anwar Elnory and Mahmoud Abosrea*
- Department of Obstetrics & Gynaecology, Benha University, Egypt
Received:August 14, 2019; Published: August 21, 2019
Corresponding author: Mahmoud Abosrea, Department of Obstetrics & Gynaecology, Benha University, Egypt
DOI: 10.32474/IGWHC.2019.03.000170
Abstract
Background: The submucous and intramural categories of uterine fibroids are considered by most reproductive practitioners are factors that could hinder embryonic implantation.
Aim: Elucidation and investigation of factors correlated to reproductive outcomes in infertility cases having myomectomy procedure for Intramural situated fibroids.
Methodology: A clinical research trial in which 150 cases having unexplained infertility in the presence of intramural fibroid category were recruited for the research study data was gathered in a retrospective fashion to elucidate the full clinical data and operative details.
Results: There was statistical significance as regards Age > 40 yrs. and Cavity entry (p values=0.0007,0.0017 consecutively), whereas there was no statistical significance for Fibroid measure on imaging and diameter of largest fibroid in correlation to successful conception occurrence.
Conclusion: Intramural fibroids removal have a positive impact in enhancing fertility potential, however in occurrence of uterine wall disruption fertility potential from myomectomy is reduced. Furthermore, age is a chief factor in maximizing the operative clinical reproductive benefit.
Keywords: Unexplained infertility; Fibroids; Myomectomy; Fertility predictability
Introduction
Fibroids are the most common benign tumor affecting the female genital tract and, in many cases, asymptomatic although having a range of prevalence of around 30 percent among reproductive female age group there is great variability in the site and size of uterine fibroids [1-3]. The submucous and intramural categories of uterine fibroids are considered by most reproductive practitioners are factors that could hinder embryonic implantation particularly in cases requiring ART management protocols [4-6].
Fibroids in general not only could affect implementation but could reduce reproductive capacity by impairment of blood supply or harmonic hormonal balance. The decision to remove uterine fibroids to increase the female reproductive potential should be balanced against the risks of permanent uterine affection, however sometimes it is an issue of high debate among fertility physicians that requires adequate justification before implementation [7-9].
Cases symptomatizing from uterine fibroids are definitely improved as regards menstrual symptoms and pressure symptoms profile by performing the myomectomy procedure but still the reproductive outcomes and conception rates among those categories of cases is an issue of research debate and requires further research efforts to elucidate possible reproductive benefits of the myomectomy procedure in patients seeking fertility management. a more research effort demanding question is whether cases with normal uterine cavity would benefit from intramural fibroid resection is an interesting concern to raise and is a common clinical case scenario [10-13].
Aim of the Work
Elucidation and investigation of factors correlated to reproductive outcomes in infertility cases having myomectomy procedure for Intramural situated fibroids.
Methodology
This clinical research trial was carried at 2 surgical places including Benha University Hospital Obstetrics and Gynecology Department, and Cleopatra Obstetrics& Gynecology Specialized center in Benha City,Qalubia Governorate, Egypt from March 2015 to January 2019. We had ethical approval for this study protocol from Benha Faculty of Medicine ethical committee; also, all included participants signed full informed written consents.
A clinical research trial in which 150 cases having unexplained infertility in the presence of intramural fibroid category were recruited for the research study data was gathered in a retrospective fashion to elucidate the full clinical data and operative details Inclusive research criteria have been as follows cases aged ≤43 years, with clinical diagnosis of unexplained infertility besides the existence of minimally one intramural leiomyoma observed by an imaging investigative tool (sonography or MRI), cases have been consecutively undergone myomectomy surgical procedure (abdominal or laparoscopic). intramural leiomyoma have been defined as a fibroid with above 50% of its volume situated within the myometrial uterine layer, research study subjects were excluded if they had ,only submucous or subserous leiomyomas or submucous and/or subserous leiomyomas coexisting with intramural leiomyomas, no desire for conception after myomectomy ,other infertility issues diagnosed (e.g. male factor, anovulation, There have been no exclusions by size or number of fibroids. Research study subjects were categorized later in to two research groups according to occurrence of conception with analysis of clinical and operative data according to reproductive outcomes to elucidate factors associated with increased conception rates in those categories of cases.
Statistical Analysis
Data were collected, revised, coded and entered to the Statistical Package for Social Science (IBM SPSS) version 23. Data were checked for normality using Kolmogorov-Smirnov test and the quantitative data with parametric distribution were presented as mean, standard deviations and ranges and compared using Independent t-test while non parametric distribution were presented as median with inter-quartile range (IQR) and compared using Mann-Whitney test. Also, the comparison between groups regarding to qualitative parameters were done by using Chi-square test and/or Fisher exact test when the expected count in any cell found less than 5. Multivariate logistic regression analysis was used to assess the parameters related to successful conception. The confidence interval was set to 95% and the margin of error accepted was set to 5%. So, the p-value was considered significant at the level of < 0.05.
Results
Table 1 reveals and displays the comparative statistical analysis between patients who conceived and patients who did not conceive as regards demographic ,baseline and preoperative characteristics in which there was a highly statistical significant difference as regards mean age +/-SD between both research categories (p value<0.001),whereas cases aged below 35 years and ranging between 35-37 years ,and cases from 38 till 39 years there was no statistically significant difference observed (p values=0.522,0.079,0.120 consecutively )whereas cases ≥ 40 years there was a highly statistical significant difference (p value<0.001),besides as regards BMI, gravidity ,parity ,duration of infertility, HCT, uterine size, uterine volume on imaging (cc),cavity impringement on imaging (p values=0.231, 0.123, 0.098, 0.205, 0.426, 0.243, 0.198, 0.216 consecutively), on the other hand fibroid volume on imaging was statistically significantly higher among the research group that conceived (p value=0.007).
Table 1: Demographic, baseline and preoperative characteristics in relation to conception.
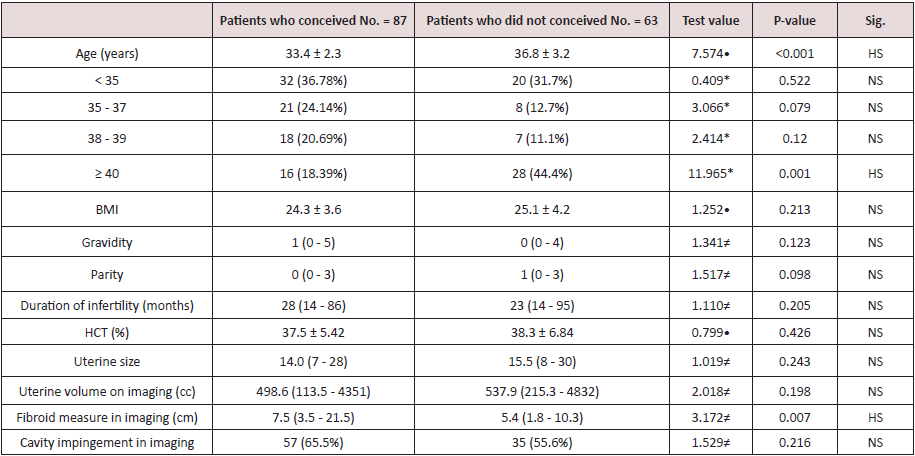
*: Chi-square test; •: Independent t-test; ≠: Mann-Whitney test
Table 2 reveals and displays comparative statistical analysis as regards operative and preoperative phase characteristics between patients who conceived and patients who did not conceive research groups in which there was no statistical significant difference as regards surgical modality ,operative time (min), blood loss(cc), uterine size (weeks) total fibroids removed, total fibroids removed, total fibroids left in situ, specimen weight (gm), cavity impingement, intraoperative complications, postoperative complications ,total complications, hospital length of stay (days) (p values=0.566, 0.262, 0.811, 0.497, 0.887, 0.384, 0.402, 0.227, 0.809, 0.750, 0.436, 0.302 consecutively), on the other hand the Diameter of largest fibroid (cm) was statistically significantly higher among the patients who conceived in comparison to cases that have conceived (p value=0.019),besides cavity entery was statistically significantly higher among cases that didn’t conceive in comparison to cases that conceived (p value=0.001).
Table 2: Operative and Postoperative phase characteristics in relation to conception.
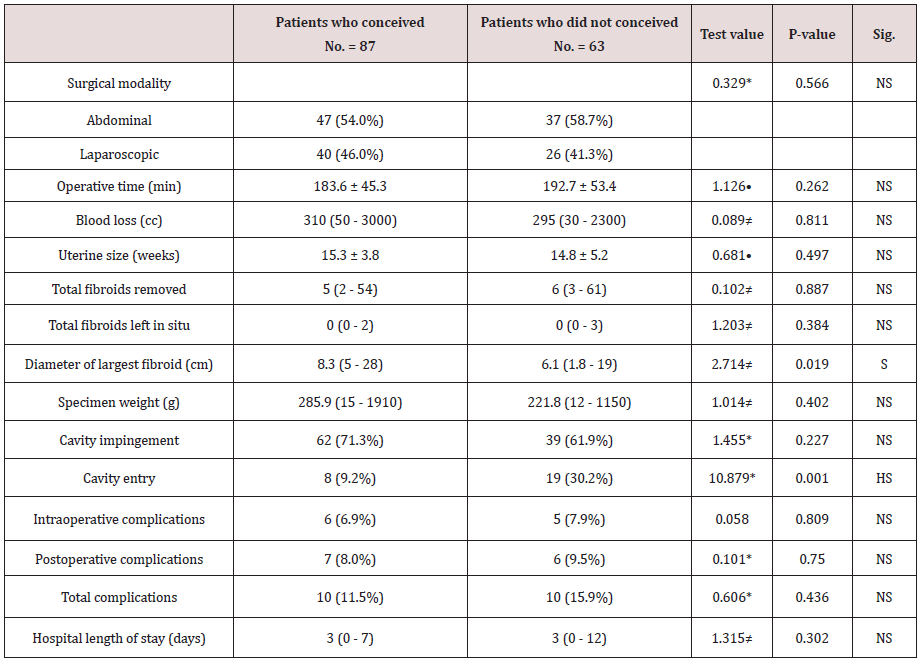
*: Chi-square test; •: Independent t-test; ≠: Mann-Whitney test
Table 3 reveals and displays that there was statistical significance as regards Age > 40 yrs. and Cavity entry (p values=0.0007, 0.0017 consecutively), whereas there was no statistical significance for Fibroid measure on imaging and diameter of largest fibroid in correlation to successful conception occurrence.
Table 3: Multivariable logistic regression analysis for factors correlated to successful conception.
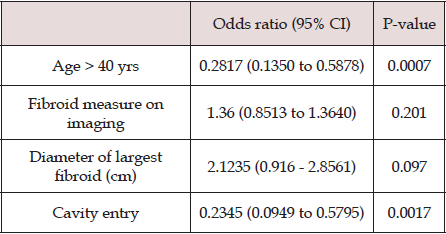
•: Independent t-test; *: Chi-square test
Discussion
Counselling cases with uterine fibroids for myomectomy to enhance chances of conception is considered one of the cornerstone practice issues in every day fertility practice this practice however should be based on research-based evidence to enhance and elucidate the possible success rates expected from infertility management protocols. Restricted research-based evidence exists as regards reproductive clinical outcomes after that indicated intervention [14,15].
A prior research study similar to the current study in approach and methodology was conducted on females having unexplained infertility issues , apart from the existence of uterine leiomyoma , interestingly it was revealed and displayed by the research group of investigators that 58.3% have accomplished conception successfully after myomectomy and 44.9% have successfully delivered a live Neonate , with a mean conception time of around fourteen months. Those indices and statistical analysis results have shown great harmony and similarity to the current research study findings, furthermore prior research groups of investigators have shown in similar indicated interventions in infertility cases a rate of pregnancy around 57%, however the conception time differed having a range of around 8 till 20 months after performing the myomectomy procedure [16,17].
Another research study previously conducted have shown among their study findings it was shown that conception was accomplished in a spontaneous manner spontaneously in about 54% of recruited cases whereas about 39% of cases had IVF management protocols required to accomplish conception successfully [18,19]. The current and prior research study findings could be justified by the fact that cases with unexplained infertility could be multifactorial in nature however when performing the myomectomy that reduces the obstacles at molecular and cellular levels for successful implantation to occur [1,4,9].
Another research study priorly performed designed in a manner to identify factors correlated and linked associated to fertility management clinical outcomes after performing myomectomy for intramural fibroids in cases having unexplained infertility issues have shown that the patient’s age at time of myomectomy procedure performance, was correlated to conception rates .furthermore another research study interestingly have shown that smaller fibroids removal, and the observation of uterine wall disruption during myomectomy, were both correlated and linked to decreased likelihood of achieving conception after finishing the myomectomy procedure [2,7,11,13].
Conclusion and Future Research Recommendations
Intramural fibroids removal has a positive impact in enhancing fertility potential, however in occurrence of uterine wall disruption fertility potential from myomectomy is reduced. Furthermore, age is a chief factor in maximizing the operative clinical reproductive benefit. future research studies are recommended to be multicentric in manner with consideration of other factors such as tubal and ovarian factors in an effort to innovate a clinical algorithm in management of those category of cases.
References
- Lu N, Wang Y, Su YC, Sun YP, Guo YH (2015) Effects of the distance between small intramural uterine fibroids and the endometrium on the pregnancy outcomes of in vitro fertilization-embryo transfer. Gynecol Obstet Invest 79: 62-68.
- Yan L, Ding L, Li C, Wang Y, Tang R, et al. (2014) Effect of fibroids not distorting the endometrial cavity on the outcome of in vitro fertilization treatment: a retrospective cohort study. Fertil Steril 101: 716-721.
- Guven S, Kart C, Unsal MA, Odaci E (2013) Intramural leoimyoma without endometrial cavity distortion may negatively affect the ICSI - ET outcome. Reprod Biol Endocrinol 11: 102.
- Christopoulos G, Vlismas A, Salim R, Islam R, Trew G, et al. (2017) Fibroids that do not distort the uterine cavity and IVF success rates: an observational study using extensive matching criteria. BJOG 124: 615-621.
- Carranza Mamane B, Havelock J, Hemmings R, Reproductive endocrinology and infertility committee; special contributor (2015) The management of uterine fibroids in women with otherwise unexplained infertility. J Obstet Gynaecol Can 37: 277-285.
- Hartmann KE, Velez Edwards DR, Savitz DA, Jonsson Funk ML, Wu P, et al. (2017) Prospective cohort study of uterine fibroids and miscarriage risk. Am J Epidemiol 7: 1-9.
- Fanchin R, Ayoubi JM (2009) Uterine dynamics: impact on the human reproduction process. Reprod Biomed Online 18(2): 57-62.
- Guven S, Kart C, Unsal MA, Odaci E (2013) Intramural leoimyoma without endometrial cavity distortion may negatively affect the ICSI - ET outcome. Reprod Biol Endocrinol 11: 102.
- Makker A, Goel MM (2013) Uterine leiomyomas: effects on architectural, cellular, and molecular determinants of endometrial receptivity. Reprod Sci 20: 631-638.
- Moawad GN, Samuel D, Abi Khalil ED (2016) Abdominal Approaches to Tissue Containment and Extraction in Minimally Invasive Gynecologic Surgery. J Minim Invasive Gynecol 23: 1032.
- Munro MG, Critchley HO, Broder MS, Fraser IS, Disorders FWGoM (2011) FIGO classification system (PALM-COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age. Int J Gynaecol Obstet 113: 3-13.
- Pitter MC, Srouji SS, Gargiulo AR, Kardos L, Seshadri Kreaden U, et al. (2015) Fertility and Symptom Relief following Robot-Assisted Laparoscopic Myomectomy. Obstet Gynecol Int.
- Sangha R, Strickler R, Dahlman M, Havstad S, Wegienka G (2015) Myomectomy to conserve fertility: seven-year follow-up. J Obstet Gynaecol Can 37: 46-51.
- Yan L, Yu Q, Zhang YN, Guo Z, Li Z, et al. (2018) Effect of type 3 intramural fibroids on in vitro fertilization-intracytoplasmic sperm injection outcomes: a retrospective cohort study. Fertil Steril 109(5): 817-822.
- Yoshino O, Nishii O, Osuga Y, Asada H, Okuda S, et al. (2012) Myomectomy decreases abnormal uterine peristalsis and increases pregnancy rate. J Minim Invasive Gynecol 19: 63-67.
- Galliano D, Bellver J, Diaz Garcia C, Simon C, Pellicer A (2015) ART and uterine pathology: how relevant is the maternal side for implantation? Hum Reprod Update 21: 13-38.
- Metwally M, Cheong YC, Horne AW (2012) Surgical treatment of fibroids for subfertility. Cochrane Database Syst Rev 11: CD003857.
- Kim MS, Uhm YK, Kim JY, Jee BC, Kim YB (2013) Obstetric outcomes after uterine myomectomy: Laparoscopic versus laparotomic approach. Obstet Gynecol Sci 56: 375-381.
- Bosteels J, Kasius J, Weyers S, Broekmans FJ, Mol BW, et al. (2015) Hysteroscopy for treating subfertility associated with suspected major uterine cavity abnormalities. Cochrane Database Syst Rev 31(1): CD009461.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...





