Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Research Article(ISSN: 2637-4544) 
Females’ Menstrual Cycle Following Severe Acute Respiratory Syndrome Coronavirus 2 Infection Volume 5 - Issue 3
Kariman Ghazal1,2,3,4*, Eva Koulaymi1, Mayssaloun Khairallah1, Ahmad Beyrouti1, Loubna Sinno5, Jihad El Hassan1,2,4,6 and Georges Yared7,8
- 1Lebanese University, Obstetrics and Gynecology Department, Beirut, Lebanon
- 2Al Zahraa Hospital University Medical Center, Obstetrics and Gynecology Department, Beirut, Lebanon
- 3Makassed General Hospital, Obstetrics and Gynecology Department, Beirut, Lebanon
- 4Rafik Hariri Hospital University Medical Center, Obstetrics and Gynecology Department, Beirut, Lebanon
- 5Makassed General Hospital, Research Unit, Beirut, Lebanon
- 6Head of Obstetrics and Gynecology, Obstetrics and Gynecology Department, Al Zahraa Hospital University Medical Center
- 7Head of Obstetrics and Gynecology Department Rafik Hariri Hospital University Medical Center, Beirut, Lebanon
- 8Assistant Professor Obstetrics and Gynecology Department Lebanese American University,Beirut, Lebanon
Received:April 18, 2022; Published: April 26, 2022
Corresponding author: Kariman Ghazal, Obstetrics and Gynaecology Department, Lebanese University, Lebanon
DOI: 10.32474/IGWHC.2022.05.000212
Abstract
Objectives: The objective was to describe and compare self-reported changes in the menstrual cycle in females who had COVID-19.
Methods: This was a cross sectional study conducted through an online questionnaire between January 1, 2021, and September 30, 2021. Included were females aged between 13 and 52 years who previously acquired COVID-19. Participants were divided into two groups; one group were females who experienced change in their menstrual cycle following COVID-19 infection and the other group were those who did not have any change.
Results: A total of 341 participants were included, 183 (53.7%) experienced change in their menstrual cycle. The mean age was 31.01±8.97 years in those without change and 32.21±9.09 years in those who had changes. Ninety (57.0%) in the unchanged cycle group had comorbidity compared to 88 (48.1%) in the other group, with anemia being the most frequent. Around 55% had irregular length while 56% had moderate and 19.6% had severe dysmenorrhea. The quantity of menses was moderate and heavy in 51.3% and 12.6% respectively. The length of menses changed in 46.6%, and 74.2% had experienced at least one menorrhagia episode.
Conclusion: COVID-19 could be associated with changes in the menstrual cycle in females of child-bearing age.
Keywords: Coronavirus disease, menstrual cycle, menorrhagia, irregular menses
Introduction
Coronavirus disease (COVID-19) has spread rapidly throughout the world to become a major disaster affecting public health [1]. Till the moment, COVID-19 is a global health crisis. COVID-19 pandemic acts as a major stressor because it could be associated with feeling grief due to fear of family loss, decrease in incomes, and loss of routine social relationships, that might all affect women’s health [2,3]. Women in particular have higher prevalence of anxiety disorders due to biological and social factors [4,5]. Women with stress-related disorders often report menstrual cycle irregularities [6 7]. The female reproductive system is prone to the effects of stress through the interconnected nature of the hypothalamicadrenal and hypothalamic-pituitary-gonadal axes [8]. Several studies reported that stress experienced during the COVID-19 pandemic could influence menstrual cycle patterns and symptoms [9-11]. Moreover, numerous studies have predicted that age and female sex are good prognosis for COVID-19 progression [1,12,13]. An epidemiological study of the COVID-19 outbreak showed that it might have a longer incubation period and less pronounced symptoms in women than in men. The mechanism underlying this difference is unclear [14,15]. COVID-19 has been reported to have multisystem complications [1]. Currently, there are no definitive clinical data on the impact of COVID-19 on the female reproductive endocrine function. Due to the paucity of data, the objective of this study was to describe and compare self-reported changes in the menstrual cycle in females who had COVID-19 infection.
Materials and methods
This was a cross sectional study conducted through an anonymous online questionnaire in Lebanon between January 1, 2021, and September 30, 2021. Included in the study were females aged between 13 and 52 years who had previously acquired COVID-19 detected through real-time reverse-transcriptasepolymerase- chain-reaction (RT-PCR). Exclusion criteria were females with history of gynecological surgery such as hysterectomy, tubal ligation, or oophorectomy; females who had menopause, were pregnant or breastfeeding during the past year; those being treated with psychotropic medications; and those who refused to participate in the study. Institutional Review Board approval was obtained. The questionnaire included data regarding sociodemographic characteristics, medical history, menstrual patterns, COVID-19 symptoms; as well as medications used. Participants were divided into two groups; one group included participants who experienced change in their menstrual cycle following COVID-19 and the other group were those who did not have any change. Change in the menstrual cycle was defined as change in the length of the cycle and/or change in the length of menses before and after the COVID-19 infection.
Statistical analysis
The Statistical Package for Social Sciences (SPSS, version 24) was used for analysis. Bivariate analysis was performed by using the Chi square test or Fisher’s exact test (as appropriate) for comparing categorical variables. Continuous variables were compared using the student’s t-test. Categorical variables were presented as number and percent while continuous variables were presented as mean and standard deviation. A p-value <0.05 indicated statistical significance.
Results
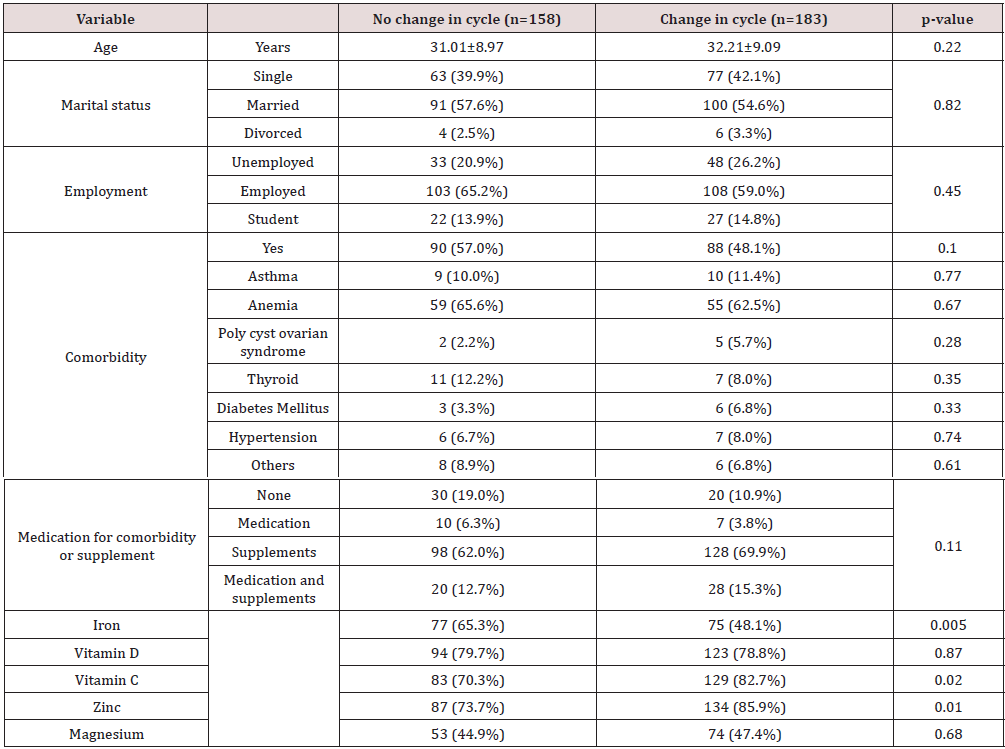
A total of 356 females participated in the study of which 15 were excluded because they have been pregnant or breastfeeding within the past year. Hence, 341 participants were included in the study. Of these, 183 (53.7%) had experienced change in their menstrual cycle. Regarding participants’ demographic characteristics, the mean age was 31.01±8.97 years in those without change and 32.21±9.09 years in those who had changes. More than 50% of the females in both groups were married and employed. Ninety (57.0%) in the unchanged cycle group had comorbidity compared to 88 (48.1%) in the other group, with anemia being the most frequent comorbidity. The majority were taking supplements before their COVID-19 infection. Approximately 65% in the no changes group consumed iron compared to 48.1% in those who had changes (p-value=0.005) while 73.7% took zinc in the no changes group versus 85.9% in the other group (p-value=0.01) (Table 1).
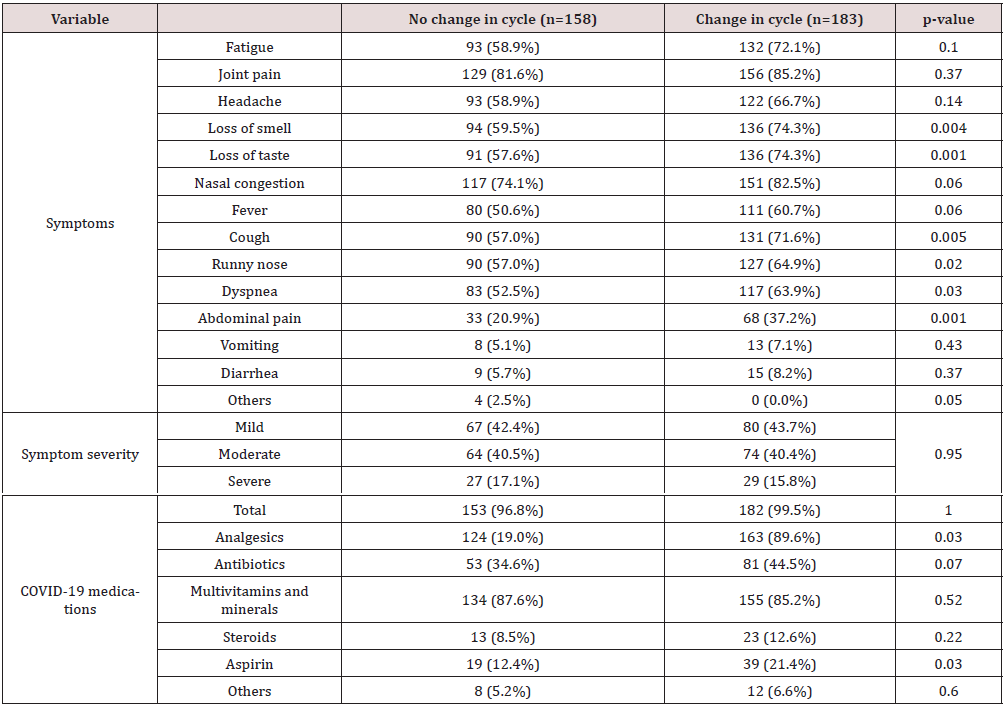
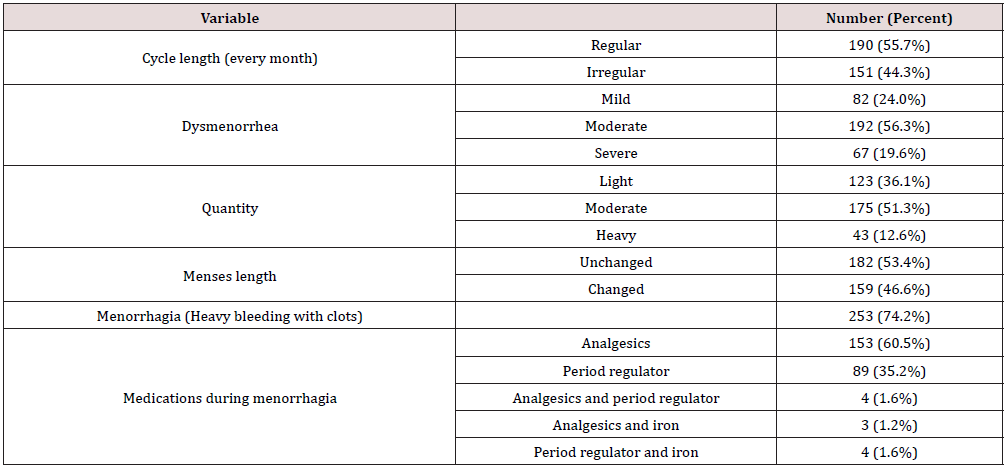
As for COVID-19 symptoms, 59.5% and 57.6% had loss of smell and taste respectively in the no changes group compared to 74.3% in those with changes (p-value=0.004 and 0.001 respectively). Moreover, 90 (57%) females had cough and runny nose in the no changes group versus 131 (71.6%) and 127 (64.9%) in the other group (p-value=0.005 and 0.02 respectively). Around 52% had dyspnea in those with no changes versus 64% in those who had changes (p-value=0.03). Some females (20.9%) in the no changes group had abdominal pain in comparison to 37.2% in the second group (p-value=0.001). Approximately 43% had mild symptoms whereas 40% had moderate symptoms in the two groups. With respect to COVID-19 medications, 19% took analgesics in those without changes compared to 89.6% in those with changes p-value=0.03). More than 80% of participants in both groups took multivitamins and minerals (Table 2). Regarding menstrual cycle characteristics after COVID-19 infection, 55.7% had regular cycle length while 55.7% had irregular cycle length. Around 24% had mild dysmenorrhea, 56.3% had moderate, and 19.6% had severe dysmenorrhea. As for quantity of menses, it was light in 36.1% of the females while it was moderate and heavy in 51.3% and 12.6% respectively. The length of menses was unchanged in 53.4% while it changed in 46.6% and 74.2% had experienced at least one episode of menorrhagia (heavy bleeding with clots). Around 60% of those who had menorrhagia took analgesics and 35.2% consumed period regulator (estrogen-progesterone oral contraceptives) (Table 3).
Discussion
Nowadays, female reproductive health has become increasingly important, and attention to the effect of COVID-19 on the reproductive system has been called for globally. Currently, there are paucity in clinical data regarding the impact of COVID-19 on the ovarian function of women of child-bearing age. Therefore, clinical evidence to confirm whether COVID-19 viral infection causes endocrine disorders and affects the menstrual cycle is urgently needed. Our study aimed to report and analyze the epidemiological and clinical characteristics of females in childbearing age who had acquired COVID-19 compare self-reported changes in the menstrual cycle. Many viruses that affect the female reproductive system and more specifically the menstrual cycle were described in the literature. These viruses are Hepatitis B, Hepatitis C and Human Immunodeficiency Virus [1,16]. They affect ovarian function through cellular immune response. In addition, an earlier age of onset of menopause was found in women with human immunodeficiency virus [1,13,17]. In addition to respiratory tract, cardiovascular and digestive systems, COVID-19 patients have been reported to have reproductive system involvement in both men and women [13,16]. A possible theory is that the pathogen of COVID-19, enters cells through its receptor, angiotensin converting enzyme-2 (ACE2) [18]. Hence, organs with high expression of ACE2 might therefore be attacked. Honorato-Sampaio et al demonstrated ACE2 expression in ovarian granulosa cells [19]. which means the ovary might also become the target of COVID-19, resulting in hormonal instability and menstrual cycle disorders.
In China as in the rest of the world, increased stress and exacerbation of depression and anxiety symptomology was reported during the COVID-19 pandemic [20]. For Altena et al, sleep has been proposed as one of the primary targets to be impacted, as well as a crucial mediator of mental health outcomes [21]. Increased stress, changes in weight and exercise, and other major lifestyle changes can affect menstrual cycle. All those changes are common during the COVID-19 pandemic. Additionally, studies have shown that some women who had COVID-19 experienced changes in their menstrual cycle including the duration, flow and accompanying symptoms such as pain [3,22,23]. Indeed, in our study, 53.7% had experienced change in their menstrual cycle. Around 56% of the participants had moderate dysmenorrhea, while 19% had severe dysmenorrhea. Li et al, reported that patients infected with COVID-19 manifested transient menstrual changes mainly prolonged cycles and decreased blood volume. Fewer patients had shortened cycle with increased volume [1]. This was consistent with our results where 44% of the female’s encountered variation in their cycle after they had recovered from COVID-19. Along with this variation, 46% mentioned having changes in the length of menses. Phelam et al reported that stress and psychosocial distress as a result of COVID-19 pandemic affects women’s menstrual health by altering the neuro modulatory cascade that drives gonadotropin releasing hormone (GnRH) regulation. Hence, chronic anovulation and hypothalamic amenorrhea ensure [3]. Moreover, Abu Helwa et al and Ibrahim NK et al stated that dysmenorrhea and menorrhagia have been related to depression, emotional instability, anxiety and psychosocial distress, all of which were linked to COVID-19 pandemic era [3,22,23]. In fact, 74% of our participants mentioned having at least on episode of menorrhagia (heavy bleeding with clots) after COVID-19 of which 35% took period regulator.
Demir et al stated that COVID-19 pandemic has increased anxiety scores which resulted in increased women’s menstrual symptoms while the length of periods and numbers of pads used decreased [11]. This was not consistent with our sample where only 36% had mild periods while the rest (64%) experienced moderate to heavy menses. They also deduced that COVID-19 is at the origin of the development of posttraumatic stress disorder due to the enormous psychological distress which, in turn, will affect the menstrual cycle process [11].
The pathophysiology of the virus and the target tissues at a molecular level must be well understood in order to clarify its impact on the endometrium and menstrual cycle [24]. Two studies endorsed the theory that the menstrual cycle might be affected by immune activation in response to various stimuli, including viral infection. Karagiannis. A et al linked immune stimulation with menstrual changes through biologically plausible mechanisms via immunological influences on the hormones driving the menstrual cycle [25]. While Monin L et al linked these effects to be mediated by immune cells in the lining of the uterus, which are involved in the cyclical build-up and breakdown of this tissue [26]. The present study had some limitations. First, we did not measure Antimullerian hormone (AMH) level, a hormone secreted by small antral follicles and is an important indicator for evaluating ovarian reserve. It is not affected by the menstrual cycle, exogenous sex hormones or pregnancy level. Hence, we would have been able to evaluate the consequence of COVID-19 on ovarian reserve and fertility, which might give an additional reason behind these menstrual changes. Second, data were collected through an online questionnaire, thus information concerning menstrual cycle heaviness were prone to subjective bias. Third, we did not follow up participants for a longer period of time to determine any deterioration or amelioration in their menstrual cycle. Fourth, pregnant women were excluded from the study, hence menstrual changes, if any, will not be recorded after they resume menses in the postpartum period.
Conclusion
COVID-19 could be associated with changes in the menstrual cycle in females of child-bearing age. Stress, anxiety, immune system alteration, GnRH pulsatility dysregulation are all accepted but not well demonstrated theories behind the exact mechanism by which the causative agent of COVID-19 alters female reproductive system, notably the menstrual cycle. Future studies are needed to further understand the underlying influence of COVID-19 on women’s reproductive health.
Author Contributions
Study conception and design was by KG. Material preparation, data collection and analysis were performed by MK, AB, HH and LS. The first draft of the manuscript was written by KG and EK. All authors commented on previous drafts of the manuscript. All authors read and approved the final manuscript.
Conflicts of Interest
The authors have no conflicts of interest.
References
- Li K, Chen G, Hou H (2021) Analysis of sex hormones and menstruation in Covid-19 women of child-bearing age. Reprod Biomed Online 42(1): 260-267.
- Naz MSG, Ramezani F (2021) SARS- COV-2: Future potential impact on timing of menarche and onset of the regular menstrual cycle in adolescence. J Pediatr Nurs 57: 90-91.
- Phelan N, Bechan LA, Owens L (2021)) The impact of the Covid-19 pandemic on women’s reproductive health. Front Endocrinol 12: 642755.
- McLean CP, Asnaani A, Litz BT, Hofmann SG (2011) Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. J Psychiatr Res 45(8): 1027-1035.
- Verma R, Balhara YP, Gupta CS (2011) Gender differences in stress response: Role of developmental and biological determinants. Ind Psychiatry J 20(1): 4-10.
- Nillni YI, Wesselink AK, Hatch EE (2018) Mental health, psychotropic medication use, and menstrual cycle characteristics. Clin Epidemiol 10: 1073-1082.
- Kim T, Nam GE, Han B (2018) Associations of mental health and sleep duration with menstrual cycle irregularity: a population-based study. Arch Womens Ment Health 21(6): 619-626.
- Valsamakis G, Chrousos G, Mastorakos G (2019) Stress, female reproduction and pregnancy. Psychneuroendocrinology 100: 48-57.
- Ozimek N, Velez K, Anvari H, Butler L, Goldman KN, Woitowich NC (2021) Impact of Stress on Menstrual Cyclicity During the Covid-19 Pandemic: A Survey Study. J Womens Health 31(1): 84-90.
- Takmaz T, Gundogmus I, Okten SB, Gunduz A (2021) The impact of COVID‐19‐related mental health issues on menstrual cycle characteristics of female healthcare providers. J Obstet Gynaecol Res 47(9): 3241-3249.
- Demir O, Sal H, Comba C (2021) Triangle of COVID, anxiety and menstrual cycle. J Obstet Gynecol 41(8): 1257-1261.
- Guan WJ, Zheng Yi N, Yu H (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382: 1708-1720.
- Chen N, Zhou M, Dong X (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395(10223): 507-513.
- Zheng H, Tan J, Ma K, Meng W (2021) Changes in Rt-PCR test results and symptoms during the menstrual cycle of female individuals infected with SARS-COV-2: Report of two cases. J Med Virol 93(1): 541-545.
- Xiong Q, Xu M, Zhang J (2020) Women may play a more important role in the transmission of the coronavirus disease (Covid-19) than men.
- Kurmanova AM, Kurmanova GM, Lokshin VN (2016) Reproductive dysfunction in viral hepatitis. Gynecol Endocrinol 32: 37-40.
- Schoenbaum EE, Hartel D, Lo Y (2005) HIV infection, drug use, and onset of natural menopause. Clin Infect Dis 41(10): 1517-1524.
- Hoffmann M, KleineWeber H, Schroeder S (2020) SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 181(1): 271-80. e278.
- Honorato-Sampaio K, Pereira VM, Santos RA, Reis AM (2021) Evidence that angiotensin-(1-7) is an intermediate of gonadotrophin-induced oocyte maturation in the rat preovulatory follicle. Exp Physiol 97(5): 642-650.
- Rajkumar RP (2020) COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr 52: 102066.
- Altena E, Baglioni C, Espie CA (2020) Dealing with sleep problems during home confinement due to the COVID‐19 outbreak: practical recommendations from a task force of the European CBT‐I Academy. J Sleep Res 29(4): e130552.
- Abu Helwa HA, Mitaeb AA, Al Hamshri S, Sweileh WM (2018) Prevalence of dysmenorrhea and predictors of its pain intensity among Palestinian female university students. BMC Womens Health 18(1): 18.
- Ibrahim NK, Al Ghamdi MS, Al Shaibani AN (2015) Dysmenorrhea among female medical students in King Abdul Aziz University: Prevalence, predictors and outcome. Pak J Med Sci 31(6): 1312-1317.
- Abhari S, Kawwas J (2020) Endometrial susceptibility to SARS COV-2 explained by gene expression across menstrual cycle. Fertil Steril 114(2): 255-256.
- Karagiannis A, Harsoulis F (2005) Gonadal dysfunction in systemic diseases. Eur J Endocrinol. 152(4): 501-513.
- Monin L, Whettlock EM, Male V (2020) Immune responses in the human female reproductive tract. Immunology 160(2): 106-115.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...