Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Editorial(ISSN: 2637-4544) 
Features of Rheumatic Disease Management while Pregnancy Volume 1 - Issue 2
Afa Bayramova*
- Department of Gynaecology & Obstetrics, Yaroslavl State Medical University, Russia
Received: December 20, 2017; Published: January 18, 2018
*Corresponding author: Afa Bayramova, Department of Gynaecology & Obstetrics, Yaroslavl State Medical University, Russia
DOI: 10.32474/IGWHC.2018.01.000109
Abstract
Rheumatism is a systemic inflammatory disease of connective tissue and joints with a predominantly affected heart. Children and young people are ill mostly: women are 3 times more likely than men. Therefore, the problem of rheumatism in pregnant women is quite common.
Keywords: Rheumatism; Pregnancy; Orthopedist
Etiology & Pathogenesis
The main etiological factor in acute forms of the disease is betahemolytic streptococcus of group A [1]. In patients with prolonged and continuously recurrent forms of rheumatic heart disease, the association of the disease with streptococcus often fails to be established. In such cases, the defeat of the heart, which fully meets all the main criteria for rheumatism, apparently has a different nature - allergic (not related to streptococcus or, in general, infectious antigens), infectious-toxic, viral. Speaking of rheumatism, it is implied that the process involves the musculoskeletal system and the cardiovascular system [2]. Given this fact, it becomes extremely clear that pregnancy with such extra genital pathology should proceed under the compulsory supervision of not only the obstetrician-gynecologist, but also the rheumatologist. According to statistical data, pregnancy itself rarely leads to the development of an unpleasant phenomenon of the future mother, such as rheumatism.
Usually, women already suffer from this ailment, only during pregnancy the disease worsens in 20% of women and causes many pregnant women to seek medical help [3]. The development of rheumatism is observed in the first months of pregnancy, when there is a weakening of immunity and the body as a whole. This indicates that the body is not able to withstand various diseases, which are mostly infectious. Births also play a significant role in the development of extra genital pathology. After all, it is well known that after giving birth, the body is significantly weakened and loses ability to fight against many diseases, including rheumatism. It takes sufficient time for the body to recover and the woman to return to her former strength. The most unpleasant thing is that if rheumatism worsens at the initial stage of pregnancy, it can lead to an interruption of the process, because any acute inflammation occurring in the body requires mandatory medical intervention and the admission of certain groups of drugs [4]. How rheumatism is manifested and how can it happen in pregnant women? Most often it is caused by beta-hemolytic streptococcus group A.
The development of the rheumatic pathological process consists of several stages:
a) a disease with sore throat, pharyngitis, scarlet fever, or other ENT infection of streptococcal nature;
b) In response to the penetration of β-hemolytic streptococcus, the immune system produces specific antibodies - the so-called “antibodies”. C-reactive proteins;
c) In the presence of a genetic predisposition to rheumatism, C-reactive proteins begin to attack their connective tissue cells (similar antigens exist on their surface, as in hemolytic streptococcus);
d) An autoimmune inflammatory process develops in the affected area - most often in the joints, myocardium, endocardium, vessels, etc. [5,6].
The provoking factors of exacerbation of rheumatism during pregnancy are [7]:
a) Hypothermia;
b) Physiological Reduction of Immunity in early Pregnancy;
c) Bacterial and Viral Infections;
d) Stress;
e) Malnutrition;
f) Exacerbation of Existing Chronic Diseases;
g) Excessive Exposure to the sun.
Speaking about the symptoms of the disease, it should be borne in mind that they are in some ways similar to those with streptococcal angina and are characterized by [8,9]:
a) general weakness;
b) the appearance of pain in the heart;
c) often minor physical exertion can provoke shortness of breath, rapid heart rate;
d) loss of appetite;
e) Joint pain, especially on days when the weather is changing noticeably; increase in temperature.
Due to the fact that during pregnancy many corticosteroid hormones are produced that have anti-inflammatory effect, the signs of exacerbation of rheumatism are blurred and not pronounced. With a heart form of rheumatism, pain in the heart is more pronounced. As a rule, the joint form is combined with the heart. It all starts with pain in the large joints. In this case, the pain passes from one group of joints to another. The cutaneous form is manifested in the appearance of characteristic pink rings on the skin, which eventually pass Rheumatism of pregnant women can lead to a condition like late toxicosis. With the exacerbation of rheumatism, there is often an acute shortage of oxygen, which can lead to placental vasculitis, changes in the placenta, intrauterine hypoxia and hypotrophy. Given the possible complications, those pregnant women who are at risk are kept under close supervision throughout the process, right up to the birth itself. If a woman has suffered several exacerbations of rheumatism, she should definitely mention this at the first visit to the doctor of a woman’s consultation. As a preventive measure, you must take care of acute infectious diseases, and if they arise, immediately go to a doctor who will prescribe an effective treatment. In addition, antirheumatic therapy is performed in pregnant women who have undergone angina or catarrh of the upper respiratory tract.
Diagnosis of rheumatism in pregnancy
Recognize and determine rheumatism in a pregnant woman can only a doctor after the examination and analysis. Diagnosing rheumatism is important in the first trimester. Because of the dangers that rheumatism causes (especially if there is heart failure and heart defects), it may be asked about the need for abortion. The diagnosis of rheumatic carditis is based on ECG (electrocardiogram), ultrasound of the heart [10]. It is necessary to consider those cases when a number of pregnant women do not suspect about the presence of rheumatism. To identify extra genital pathology, laboratory (diagnostic) studies are mandatory. Speaking about the complex of diagnostic examination, we mean the delivery of a blood test, as well as ultrasound, an echocardiogram of the heart. These indicators can give accurate information about whether a pregnant woman suffers from rheumatism or not.
Particular attention is paid to increasing the heart rate. In pregnant women suffering from a disease such as rheumatism, the heart rate has a more pronounced picture than the usual (healthy). Nevertheless, it should not be forgotten that in most cases this picture may indicate more about the development of insufficiency in pregnant blood circulation, rather than the development of rheumatism. Therefore, several methods are used to obtain more accurate and reliable information about the work of the heart. In this case, an important role in the diagnosis is played by ECG (electrocardiogram) indicators, such as: increase / flattening / broadening of the P-Q interval; serration of the tooth P; QRS complex changes; slight or, conversely, a significant decrease in the ST segment and T wave. In addition to the results of ECG and ultrasound of the heart, blood tests are used to diagnose rheumatism. Practice shows that rheumatism, especially if there is a tendency to exacerbate it, leads to an increase in ESR (sedimentation rate erythrocytes) to 35-50 mm / h. When conducting a biochemical blood test in pregnancy, the main indicators are [11]:
a) C-reactive protein;
b) Hexose;
c) Ceruloplasmin;
d) Seromucoid;
e) Hydroxyproline;
f) A2-globulin.
As for the indicator, such as fibrinogen, which is determined by the blood test, it is not given special attention, since it is always elevated in pregnant women and does not indicate an increase in rheumatism. Another issue is the identification of those pregnancy periods in which one can expect activation of the rheumatic process. Almost all authors agree that the most frequent exacerbation of rheumatism occurs in the first trimester of pregnancy. The second vulnerable period is postpartum; sometimes an exacerbation occurs at a gestational age of 28-32 weeks, so it is reasonable to conduct an anti-relapse treatment in these periods and especially in the first 3 months of pregnancy and immediately after delivery. It should be noted that the risk of exacerbation is not limited only to the postpartum period. These people may come several months after the birth, demanding special monitoring of this contingent of women for a longer time (at least, up to 6-12 months).
Many pregnant women are wondering: why should the survey be conducted at an early stage, that is, in the first months and even weeks of pregnancy? The fact is that pregnant women with rheumatism require serious treatment, especially if it is a question of exacerbating it. If the treatment is serious enough, that is, the expectant mother should take strong drugs, then the process should be suspended. That is, in this case, it will be about the termination of pregnancy. There is nothing comforting in this, of course, not, as most of the pregnant women fall into depression and understand that they do not promise birth in the near future. However, such an approach to solving the problem is most appropriate, since rheumatism has the ability to negatively affect the development and formation of the baby’s future. To avoid any consequences, doctors are advised to terminate the pregnancy, undergo a full course of treatment and only then think about re-conception of the child. Exacerbation of the rheumatic process during pregnancy, and even more so if a woman becomes pregnant with an active rheumatic process, is fraught with the possibility of a number of complications of pregnancy. Thus, according to the materials of the authors [12], with an active rheumatic process, deviations from the normal course of pregnancy are observed one and a half times more often than with the inactive and pathological births - more than twofold.
Our observations confirm these data: premature termination of pregnancy, late toxicosis, threatening fetal asphyxia, premature discharge of amniotic fluid was more frequent. Of particular note is the late toxicosis, which in patients with rheumatism often occurs atypically, at a “normal” level of arterial pressure against the background of impaired blood circulation, caused by activation of the rheumatic process. If you recognize the allergic nature of late toxicosis, you can understand why it often occurs with rheumatism. In the case if rheumatism in pregnant women is mild, that is, there is no exacerbation, and the issue of termination of pregnancy is closed. However, the future mother in any case is under the supervision of her attending physician before the birth begins. This is necessary to ensure the safety of both the pregnant woman herself and her future baby. She is recommended to undergo at least two procedures in the hospital mode for the entire period of pregnancy.
Complications
What is the risk of rheumatism in pregnancy?
In the early stages of aggravation of rheumatism can cause miscarriage or defects in the formation of the fetus. In the second and third trimester, exacerbation of rheumatism can lead to the following complications and consequences [13]: damage to the blood vessels of the placenta causes hypoxia, hypotrophy and intrauterine fetal death;.
a) Edema and pulmonary infarction; Thrombophlebitis;
b) Rheumatic carditis of the future mother becomes the cause of fetal hypoxia, which entails various violations of its intrauterine development
c) Severe fetal malformations;
d) Premature separation of amniotic fluid;
e) Threat of premature termination of pregnancy; late toxicosis (gestosis);
f) Threat of fetal asphyxia;
g) Decomposition, threatening the life of a pregnant woman.
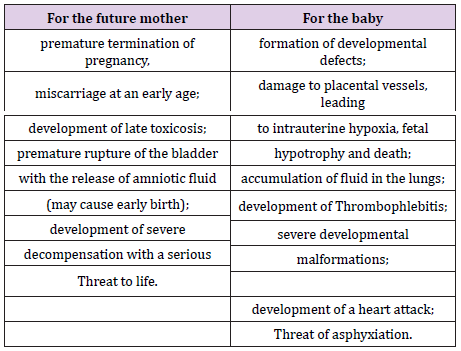
Due to active rheumatic endocarditic, in some cases sudden death may occur during childbirth or soon after (Table 1).
Treatment
What to do in case of an exacerbation of rheumatism and how to cure it during pregnancy?
A. Treatment of pregnant women will depend on the following factors:
a) The degree of the disease;
b) Clinical form of rheumatism;
c) Individual characteristics;
d) Condition of the heart muscle, valvular heart apparatus
e) Results of the survey;
f) Presence of other diseases;
g) The course of the pregnancy process.
To treat rheumatism during pregnancy is necessary, as dangerous complications threatening the life of the future mother and her child can develop.
B. There are several important rules in treatment [14]
a) At detection of foci of infection or expressed activity of pathological processes (2nd or 3rd degree of rheumatism) antibacterial therapy is shown, including the use of drugs from the penicillin group and its synthetic derivatives.
b) In the first 10 weeks of gestation, the use of aspirin is contraindicated because of teratogenic effects. Do not take it before birth, because it has hypo coagulant properties and increases the risk of bleeding.
c) In severe toxicosis, analgin cannot be used because it can cause difficulties in removing the fluid from the body. NSAIDs are also contraindicated, and corticosteroids are resolved only after the end of the first trimester, when antirheumatic therapy does not help.
Timely begun therapy in most cases saves the life of the mother and the future baby. In the therapy of any disease, the spirit mood is important. Often, pregnant women become depressed after learning about rheumatism and its consequences. This is extremely untrue. It is necessary to assess together with the doctor all possible outcomes of the pathology and make the right choice. When there is a real threat to the baby and his mother, it makes sense to interrupt the pregnancy in order to undergo a full course of treatment and start planning a re-conception. In the absence of a significant threat, you should follow all the doctor’s recommendations and adjust to the best. This will help the body to regain strength and coupled with competent therapy to stop the progression of the disease.
C. What can the patient do?: The occurrence of the above symptoms should be alerted, you should immediately contact a therapist or rheumatologist. It is better to carry out the treatment even before the onset of pregnancy, since medications negatively affect the intrauterine development of the baby. In case of rheumatism it is advisable to be treated at least twice during the pregnancy period in a hospital. It is necessary to comply with bed rest during the exacerbation stage, to fully eat and fulfill all the prescriptions of the doctor.
D. What does the doctor do?: After examination, the doctor prescribes antibiotics, drugs with hyposensitizing and antiinflammatory action, sedatives, vitamin remedies, etc. It is also important to monitor the condition of the baby. If future mothers are late, you should visit your gynecologist regularly and listen to the fetal heartbeat.
Prevention
A. Is it possible to prevent the onset of rheumatism or its aggravation during pregnancy?
a) the risk can be minimized if one adheres to the following principles: beware of acute infectious catarrhal diseases - avoid public places during epidemics;
b) timely treatment of tonsillitis, pharyngitis, otitis, sinusitis - foci of streptococcal infection;
c) conduct hygiene of the oral cavity - treat tooth decay, periodontal disease, gingivitis, candidiasis of the oral mucosa;
d) do not overcool and do not undergo excessive sun exposure; maintain immunity;
e) Ensure that the diet contains all the necessary vitamins and microelements, the need for which is increased during pregnancy.
B. The likelihood of developing rheumatism or exacerbations during childbearing can be minimized by performing the following preventive measures [15]
a) it is necessary to beware of catarrhal diseases: avoid crowded public places during epidemics, take a complex of vitamins and minerals for pregnant women;
b) timely treatment of foci of streptococcal infection - pharyngitis, tonsillitis, sinusitis and otitis;
c) maintain oral hygiene: brush your teeth daily and treat dental diseases - dental caries, periodontal disease, candidiasis and gingivitis;
d) Do not overcool and avoid long exposure to direct sunlight.
It is necessary to eat fully, walk more, avoid overstrain of muscles, agitation and stress. It is useful to do morning exercises and go swimming. Rheumatism in most pregnant women often occurs before the onset of conception. The period of bearing of the baby aggravates its course, causing a vivid clinic of the disease. This refers to the first months when the body adapts to a new status, and the immune system weakens [16]. As a result, control of the disease is lost, and its symptoms are aggravated, which is a significant threat to the baby and his mother. To reduce the likelihood of all risks to a minimum, it is strongly recommended that you plan your pregnancy and take timely therapy for rheumatism. In this case, you can successfully take a future child and become a mother.
References
- Katz PP (2006) Childbearing decisions and family size among women with rheumatoid arthritis. Arthritis Rheum 55(2): 217-223.
- Sanchez Guerrero J, Uribe AG, Jimenez Santana L, Mestanza Peralta M, Lara Reyes P, et al. (2005) A trial of contraceptive methods in women with systemic lupus erythematosus. N Engl J Med 353(24): 2539-2549.
- Chambers CD, Johnson DL, Jones KL (2006) The OTIS Collaborative Research Group. Pregnancy outcome in women exposed to leflunomide: The OTIS Autoimmune Diseases in Pregnancy Project. Arthritis Rheum.
- De Man YA, Dolhain RJEM, Van de Geijn FE, Stijnen T, Hazes JM (2006) Does rheumatoid arthritis ameliorate during pregnancy? Results from a Prospective Nationwide Cohort Study (the PARA-study) Arthritis Rheum.
- Ostensen M, Villiger PM (2007) The remission of rheumatoid arthritis during pregnancy. Semin Immunopathol 29(2): 185-191.
- De Man YA, Dolhain RJ, Van de Geijn FE, Willemsen SP, Hazes JM (2008) Disease activity of rheumatoid arthritis during pregnancy: results from a nationwide prospective study. Arthritis Rheum 59(9): 1241-1248.
- Vignali DA, Collison LW, Workman CJ (2008) how regulatory T cells work. Nat Rev Immunol 8(7): 523-532.
- Forger F, Marcoli N, Gadola S, Moller B, Villiger PM, et al. (2008) Pregnancy induces numerical and functional changes of CD4+CD25 high regulatory T cells in patients with rheumatoid arthritis. Ann Rheum Dis 67(7): 984-990.
- Forger F, Villiger PM, Ostensen M (2009) Pregnancy in patients with ankylosing spondylitis: do regulatory T cells play a role? Arthritis Rheum 61(2): 279-283.
- Romero Diaz J, Garcia Sosa I, Sanchez Guerrero J (2009) Thrombosis in systemic lupus erythematosus and other autoimmune diseases of recent onset. J Rheumatol 36(1): 68-75.
- Clowse ME, Jamison MG, Myers E, James A (2008) A national study of the complications of lupus in pregnancy. Am J Obstet Gynecol 199(2): 127.
- Cavallasca JA, Laborde HA, Ruda Vega H, Nasswetter GG (2008) Maternal and fetal outcomes of 72 pregnancies in Argentine patients with systemic lupus erythematosus (SLE). Clin Rheumatol 27(1): 41-46.
- Laube GF, Kemper MJ, Schubiger G, Neuhaus TJ (2007) Angiotensinconverting enzyme inhibitor fetopathy: long-term outcome. Arch Dis Child Fetal Neonatal Ed 92(5): F402-403.
- Bick RL (2008) Antiphospholipid syndrome in pregnancy. Hematol Oncol Clin North Am 22(1): 107-120.
- Salmon JE, Girardi G (2008) Antiphospholipid antibodies and pregnancy loss: a disorder of inflammation. J Reprod Immunol 77(1): 51-56.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...