
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Research Article(ISSN: 2637-4544) 
Factors Associated with Success Rate of Vaginal Birth After Single Caesarean Section in Khartoum Maternity Hospital Volume 2 - Issue 3
Amir Elnahas1* and Maysoun Izzeldien Ahmed2
- 1Assistant professor at Weill Cornell Medical College- Qatar, Sidra Senior consultant at Sidra medical centre, Department of Obstetrical & Gynecology
- 2Department of Obstetrical & Gynecology, hospital Muscat Oman
Received: August 16, 2018; Published: August 23, 2018
Corresponding author: Amir Elnahas, Assistant professor at Weill Cornell Medical College- Qatar, Sidra Senior consultant at Sidra medical centre, Department of Obstetrical & Gynecology
DOI: 10.32474/IGWHC.2018.02.000140
Abstract
Objectives: To determine success rate of VBAC (Vaginal birth after cesarean section) with reference to prognostic factors to predict successful VBAC in Khartoum Maternity Hospital- Sudan
Methodology: It was descriptive, cross sectional and hospital based study conducted in a period of one year, involving 342 pregnant women with one previous C/S who were admitted in the labor room as emergency cases, were evaluated thoroughly, data collected through designed questionnaire include:- Socio-demographic characters, antenatal clinic follow up, previous C/S, variables affect success of VBAC and outcome of current pregnancy.
Results: A total of 342 pregnant women involved in this study, the majority of them (78.36%) were counseled for VBAC. Fetal distress was the most common cause for previous C/S (39.77%) and failure to progress account for 24.56%. Factors affecting success of the VBAC in this study were; BMI between 25-30 was 58.77%, previous successful VBAC was 44.15% and birth weight between 3-3.5kg was 47.37%. The outcome of this pregnancy were; 67.3% had successful VBAC, while 23.7% had emergency caesarean section
Conclusions: This study reported 67.3% success rate of VBAC and concludes a significant increase in the successful rate of VBAC associated with accurate prior ante natal care, meticulous counseling, prior vaginal delivery, previous success VBAC, BMI between 25-30 and maternal age <35 years.
Keywords: VBAC; Success rate; Prognostic factors; Sudan
Introduction
From the late 1980s to mid-1990s vaginal birth after caesarean (VBAC) rates increased in North America. This was a response to public and professional concerns about rising caesarean section rates and increasing evidence indicating that in the absence of contraindications, VBAC is a safe choice [1]. however, since the mid-1990’s, the rate of VBAC has declined dramatically in Canada, with the repeat caesarean section (C/S) rate having increased from 64.7% in 1995 to 82.4% in 2008 [2,3]. this increase has occurred despite a consensus, reflected in professional guidelines, that VBAC is a safe and appropriate option for most women who have had a previous cs [4-7]. Although attempts at a trial of labor after a cesarean birth (TOLAC) have become accepted practice, the rate of successful vaginal birth after cesarean delivery (VBAC), as well as the rate of attempted VBACs, has decreased during the past 10 years. Whereas, 40-50% of women attempted VBAC in 1996, as few as 20% of patients with a prior cesarean delivery attempted a trial of labor in 2002. This number is drifting down toward the 10% mark with fewer than 10% of women achieving successful VBAC in 2005[1]. This study attempts to highlight the various factors which have a prognostic significance for success of VBAC.
Material and Methods
It was cross sectional, prospective and hospital-based study conducted during one year (January\2011- December\2011), involving 342 patients with one previous C/S. All the patients with one previous caesarean section who were admitted in the labor room as emergency cases, were evaluated thoroughly. A detailed history regarding the type of operation, indication, birth weight of infant, prior vaginal births, puerperal complications in previous deliveries etc., were obtained. The presentation, estimated birth weight of present infant, condition of scar and adequacy of pelvis was ascertained. Routine investigations like CBC, Rh group etc. was carried out. Ultrasonography was carried out in all the booked patients to know the maturity of fetus, placenta localization and to rule out anomalies. The patients were carefully selected for vaginal trial of labor based on the ACOG recommendations and were taught to recognize the basic signs and symptoms of labor as well as scar dehiscence. Statistical analysis was performed via SPSS software (SPSS, Chicago, IL, USA). Continuous variables were compared using student’s t test (for paired data) or Mann-Whitney U test for non-parametric data. For categorical data, comparison was done using Chi-square test (X2) or Fisher’s Exact test when appropriate. A P value of <0.05 was considered statistically significant.
Ethical clearance and approval for conducting this research was obtained from the general manager of the hospital and informed written consent was obtained from every respondent who agreed to participate in the study. Of course, the respondents informed that the study is not associated with experimental or therapeutic intervention while information was collected from her.
Results
Table 1: VBAC and demographic data with significance table and the p value among respondents.
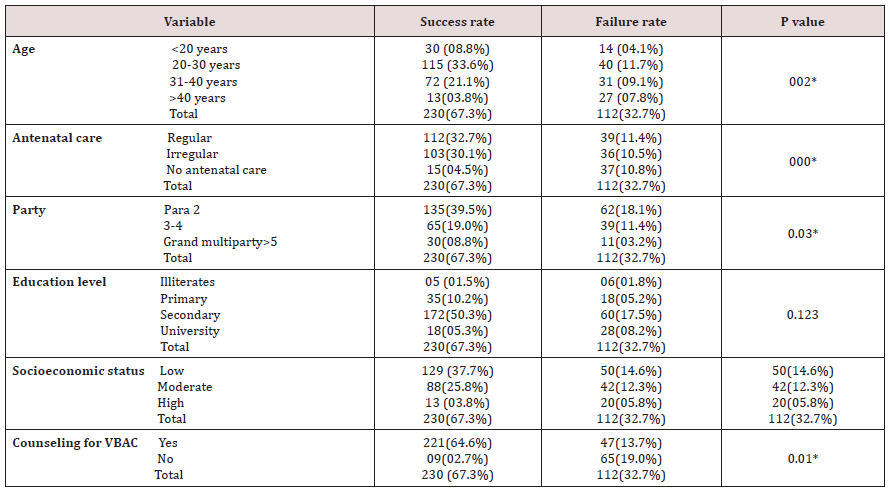
*Statistically significant at 0.05 level
Table 1 The mean ± SD of age was 25.7 + 3.1 years, 67.8% of women were secondary educated, almost half of them were in low socioeconomic status and majority of patients (88.0%) were paras between 2-4. Antenatal clinic follows up to 5 visits 151(44.15%), more than 5 visits were 139(40.65%) and no follow were 52(15.2%). Counseled for VBAC in antenatal clinic were 268(78.36%) and not counseled were 74(21.64%) (Table 2).
Table 2: VBAC and prognostic factors with significance table and the p value among respondents.
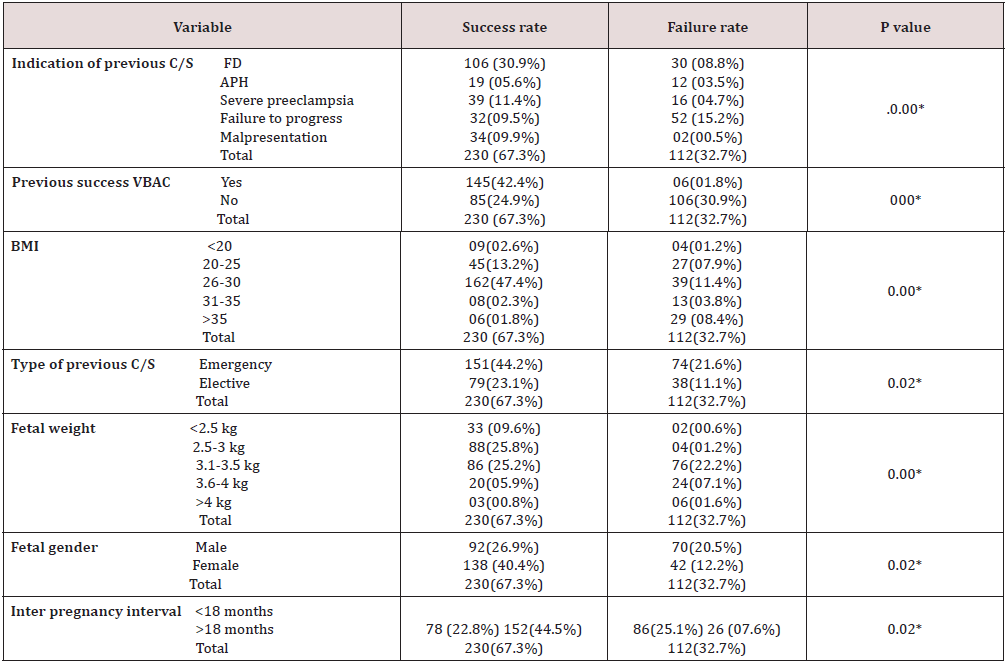
*Statistically significant at 0.05 level
Indication of the previous caesarean section were fetal distress 136(39.77%), APH 31(9.06%), severe preeclampsia 55(16.08%), failure to progress 84(24.56%) and mal presentation 36(10.53%). Caesarean section done emergency in 225(65.79%) and elective in 117(34.21%). The body mass index less than 20 was 13(3.81%) of women, between (20 - 25) 72(21.05%), between (25 - 30) 201(58.77%), between (30 - 35) 21(6.14%) and more than 35 35(10.23%). Previous successful VBAC in 151(44.15%) of women and no previous successful VBAC 191(55.85%). The study showed a significant correlation between successful rate of VBAC and following factors, accurate prior ante natal care, meticulous counseling, prior vaginal delivery, previous success VBAC, maternal age <35 years, increased parity, body mass index (25-30), birth weight less than 4kg, inter pregnancy interval >2 years, female fetus and non-recurrent indications, such as breech birth and APH.
Discussion
Vaginal birth after cesarean section (VBAC) has been strongly advocated, resulting in a significant increase in attempted and successful vaginal births and a decreasing overall cesarean section rate. However, recently, some cautions have been raised surrounding complications such as uterine rupture or uterine dehiscence that may occur with VBAC and, as such, VBAC rates have declined. VBAC is becoming a standard of practice in all obstetrical institution around the globe, the success rate of trial of vaginal birth after one previous cesarean section have been reported to be 60-80%. In this study success rate of VBAC 67.3% which is comparable with previous studies and the globe standard [8,9]. The current study demonstrated that, there is significant decline in the success rate of VBAC with increase maternal age and revealed only 3.8% of women >40 years had success VBAC compared with 33.6% success rate among women age between 20-30 years. This finding is similar with studies done by Wing DA which was reported that after adjusting for confounding factors, women older than 40 years who have had a prior cesarean delivery have an almost 3-fold higher risk for a failed trial of labor compared with women younger than 40 years. In one scoring system, women younger than 40 years were given an extra point as a predictor for successful VBAC [10]. Bujoldeta l4 also reported from their14year study covering 2493 women that maternal age at the time of TOL equal or greater than 35years old was associated with a lower rate of successful vaginal delivery (OR :0.73,95%CI: 0.56-0.94). While previous studies have evaluated pre-pregnancy weight and height to examine the effect on mode of delivery, all of which show that women in the morbidly obese range have a higher risk of failing a trial of labor [11]. Our study found low rates of success VBAC with increase maternal BMI the result of the present study found that only 1.8% success rate of VBAC for women more >35 BMI.
In one study of 510 women with a single C/S, women with prepregnancy BMI ≥ 30 were less likely to experience VBAC compared to women with a BMI of 20-25 (546/1000 vs. 705/1000). Women with BMI < 19.8 were most likely to experience a planned VBAC (850/1000). After controlling for other factors, including recurring indications for C/S, increasing BMI was significantly associated with a lower rate of vaginal birth [12]. The present study revealed higher likelihood of success VBAC among women who have had at least one success VBAC and prior vaginal delivery. Again, Our study match meta- analysis performed by Guise et al who concluded that women with prior VBAC were three to seven times more likely to have a VBAC for their current delivery, compared to women choosing VBAC who had not had a prior vaginal delivery [13].
Women with neonatal weights exceeding 3kg in our study had less chances of successful VBAC compared to those having neonatal weights<=3kg.Asimilar result was obtained by another study in which it was concluded that the chances of vaginal delivery decreased as the fetal weight exceeded 3.5kg(P<0.05)2. The indication of prior cesarean section was significantly associated with the success of current VBAC in our study. VBAC was maximally successful in patients who were operated previously for non-recurrent indications such as mal presentations. Again, our study comparable with several studies which have examined indications for prior cesarean delivery as a predictor of outcome in a subsequent trial of labor. In all studies, Failure to progress, CPD, or dystocia as indications for prior cesarean delivery are also associated with a higher proportion of patients not attempting a trial of labor after cesarean birth [9]. In a meta-analysis of the existing literature prior to 1990, Rosen et al demonstrated that women whose prior cesarean delivery was performed for CPD were twice as likely to have an unsuccessful trial of labor [14]. The timing between pregnancies has recently become an interesting predictor for a number of obstetric outcomes, VBAC success among them. In the present study, women who had an inter pregnancy interval of more than 18 months had an 44.5% chance of VBAC success, while women whose inter pregnancy interval was less than 18 months had a VBAC success rate of 22.8%. Chhabra [15], concluded that an inter conception period of <19months was associated with adverse outcome of VBAC.
Conclusion
The study concludes that a significant increase in the successful rate of VBAC associated with accurate prior ante natal care, meticulous counseling, prior vaginal delivery, previous success VBAC, maternal age <35 years, increased parity, body mass index (25-30), birth weight less than 4kg, inter pregnancy interval >2 years, female fetus and non-recurrent indications, such as breech birth and APH.
References
- Millar wJ, nair c, wadhera s (1996) Declining cesarean section rates: a continuing trend? health rep summer 8(1):17-24 (Eng); 17-24 (Fre).
- (2008) Public health agency of canada (phac). canadian perinatal health report: 20008 Edition.
- Canadian institute of health information (cihi). childbirth Quickstats 2006-2007 to 2008-2009. 2010.
- (2005) Society of obstetricians and gynaecologists, of canada. sogc clinical practice guidelines. guidelines for vaginal birth after previous caesarean birth. number 155 (replaces guideline number 147), February 2005. International Journal of gynaecology & obstetrics 89(3): 319-331.
- Bangdiwala si, brown ss, cunningham Fg, Dean tm, Frederiksen m, et al. (2010) nih consensus Development conference Draft statement on Vaginal birth after cesarean: new insights. NIH consens state sci statements 27(3): 1-42.
- (2010) American college of obstetricians and gynecologists. acog practice bulletin no. 115: Vaginal birth after previous cesarean delivery. obstet gynecol 116(2 pt 1): 450-463.
- (1998) National collaborating centre for women’s and children’s health. caesarean section. Fylstra DL. Tubal pregnancy: a review of current diagnosis and treatment. Obstet Gynecol Surv 53: 320-328.
- Bujold E, Hammoud AO, Hendler I, Berman S, Blackwell SC, et al. (2004) Trial of labor in patients with previous cesarean section: does maternal age influence outcome? Am J Obstet Gynecol 190: 1113-1118.
- Shakti V, Behera RC, Sandhu GS, Singh Anita, Bandhu HC (2006) Vaginal birth after cesarean delivery. J Obstet Gynecol India 56: 320-323.
- Wing DA, Lovett K, Paul RH (1998) Disruption of prior uterine incision following misoprostol for labor induction in women with previous cesarean delivery. Obstet Gynecol 91(5 Pt 2): 828-830.
- Lydon-Rochelle M, Holt VL, Easterling TR, Martin DP (2001) Risk of uterine rupture during labor among women with a prior cesarean delivery. N Engl J Med 345(1): 3-8.
- Durnwald CP, Ehrenberg HM, mercer BM (2004) The impact of maternal obesity and weight gain on vaginal birth after cesarean section success. american Journal of obstetrics & gynecology 191(3): 954-957.
- Guise JM, Eden K, Emeis C, Denman MA, marshall N, et al. (2010) Vaginal birth after cesarean: new insights. Evid rep technol as- sess (Full rep) (191):1-397.
- Rosen MG, Dickinson JC, Westhoff CL (1991) Vaginal birth after cesarean: a meta-analysis of morbidity and mortality. Obstet Gynecol 77(3): 465- 70.
- Chhabra S, Arora G (2006) Delivery in women with previous cesarean section. J Obstet Gynecol India 56: 304-347.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...















