Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Research Article(ISSN: 2637-4544) 
Evaluation of The Efficacy of Pipelle In Diagnosis of Endometrial Lesions in Cases of Perimenopausal Bleeding Volume 4 - Issue 2
Nagy M Metwally Ahmed*
- Faculty of Medicine, Zagazig University, Egypt
Received: December 02, 2020; Published: January 27, 2020
Corresponding author: Nagy M Metwally Ahmed, Lecturer of Obstetrics and Gynecology, Obstetrics and Gynecology Department, Faculty of Medicine; Zagazig University, Zagazig, Egypt
DOI: 10.32474/IGWHC.2020.04.000182
Abstract
One of the most common gynecologic complaint is irregular uterine bleeding It is one of the most common Problem in the perimenopausal and postmenopausal years. It has a direct impact on woman physical, social, emotional and material quality of life. While vaginal bleeding is the sign of endometrial cancer in more than 90% of postmenopausal women which is the sixth most common malignant neoplasm in women worldwide and is the most common gynecologic malignancy in developed countries, therefore, the diagnosis of AUB needs to be undertaken seriously. This study was implemented to evaluate the efficacy of suction pipelle-which is an endometrial sampling technique- in diagnosis of endometrial lesions in cases of abnormal uterine bleeding. It was designed as a cross sectional study and included 184 patients complaining of AUB. 2 samples were taken from all candidate women one by D&C and the other was by pipelle device and the results of histopathological examination of both were compared regarding that D&C was the gold standard. After statistical analysis of the present study by SPSS version 23 software, the 2 methods were 100% matched in diagnosis of secretory endometrium, hormone dependent endometrium, atypical hyperplasia and EEC grade 1. The pipelle succeeded to diagnose some cases of proliferative endometrial and simple hyperplasia which were missed by D&C (18.5% and 17.4% by pipelle versus 16.3% and 13% by D & C respectively). Unfortunately, there were cases the pipelle failed to diagnose, as in some cases of endometrial polyp and disordered endometrial hyperplasia which diagnosed by D&C (8.7% and 17.4% by pipelle versus 16.3% and 19.6% by D& C respectively).
Conclusion: Pipelle is an outpatient procedure which avoids general anesthesia and its related risks, does not need room or personnel in the operating theatre, is less painful, is more cost-effective and obtains an accurate specimen with consistent histopathology results compared to D&C. It would, however, have decreased sensitivity for endometrial polyp diagnosis and hyperplasia.
Introduction
Abnormal uterine bleeding (AUB) is a significant clinical
entity complaint among women in reproductive age attending
to an outpatient clinics [1] it may have a significant impact on
woman physical, social, emotional and material quality of life along
with the direct impact on the woman and her family, there are
significant costs to both economy and health service [2]. AUB is an
abnormal uterine bleeding that occurs in the absence of identifiable
pathology. This represents a disturbance to the endometrial lining
of the normal cyclic of ovulatory hormonal stimulation. In many
cases, the bleeding is unpredictable. It can be too heavy or light and
prolonged, irregular, or random [3].
The working group on menstrual disorders of the International
Federation of Gynecology and Obstetrics, FIGO, has recently
developed a classification system (PALM-COEIN) for AUB
causes in non-gravid women of reproductive age. There are
nine main categories grouped under the acronym PALM-COEIN:
polyp; adenomyosis; leiomyoma; malignancy and hyperplasia;
coagulopathy; ovulatory dysfunction; endometrial; iatrogenic;
and not yet classified [4]. Endometrium assessment methods are
numerous in patients with abnormal uterine bleeding, these are
ultrasonography, D&C, office-based methods as hysteroscopic
biopsy or endometrial samplers such as suction pipeline [5].
In women with abnormal uterine bleeding, the main cause for
performing endometrial biopsy is to confirm the benign nature of
the problem by excluding endometrial carcinoma so appropriate
management can be [6] Throughout decades, the endometrial
curettage is the gold standard endometrial sampling tool. However,
in sixty percent of cases, it can lead to less than 50% curettage
of endometrium and is also accompanied by infection risk and
perforation. It also requires hospital admission and local or general
anesthesia [5].
Aim of the Work
Evaluation of the efficacy of suction pipelle in diagnosis of endometrial lesions in patients with abnormal uterine bleeding
Patients and Methods
Conclusion
The study was Cross sectional study carried out at Gynecology
and Obstetrics Department, Armed Forces Hospitals of South
Region. Gazan, KSA. during the period from April 2017 to May 2019.
184 patients included in this study they had Abnormal vaginal
bleeding although medical therapy.
Exclusion criteria:
a. Lower genital tract infection.
Local gynecological cause.
b. Patients with bleeding disorders (Coagulopathy,
thrombocytopenia (less than 100/000 platelet per mm3).
c. Use of anti-coagulants.
d. Bleeding due to endocrinological disorders (thyroid
diseases and diabetes) or due to liver or renal impairment.
e. An informed verbal and written consent were obtained
from every subject.
All cases who met inclusion criteria were subjected to the
following:
History
Full history was taking including: personal, present, past, family, obstetric, history of drug intake, contraceptive and menstrual history.
Detailed History about duration, amount and pattern of bleeding.
Examination
General examination: Including Blood pressure, pulse, temperature and respiratory rate.
Abdominal examination: Evaluation of fundal level. Presence of any scars of previous operations.
Laboratory investigation: CBC will be conducted, coagulation profile, hormonal assay consisting of thyroid function tests, serum prolactin, liver and kidney function tests. Transvaginal ultrasonography TVS for assessment of myometrium, endometrial thickness and uterine cavity. On the day of operation and after vaginal washing and speculum placement in lithotomy place, patients are moved to the operating room. the sampling was performed preceding to anesthesia, dilatation and using of suction pipelle. The sheath piston was drowned back to make negative gradient after the pipelle was inserted into the uterine cavity and then the pipelle was slowly removed. The procedure was repeated more than one as much if the sample was insufficient. In container A, the samples were collected. Using the curette number 3 or 4 and the samples were assembled in container B. The samples were sent to the same pathologist for histopathological evaluation. Patients and pathologists were blinded about the sampling sequence and the sampling method used for each sample.
Results
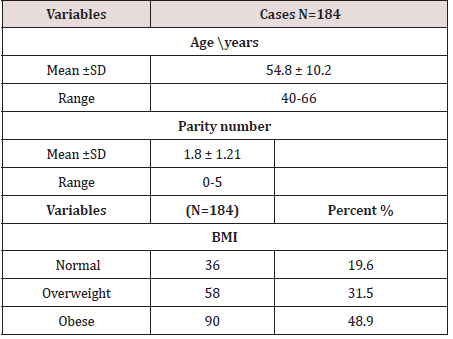
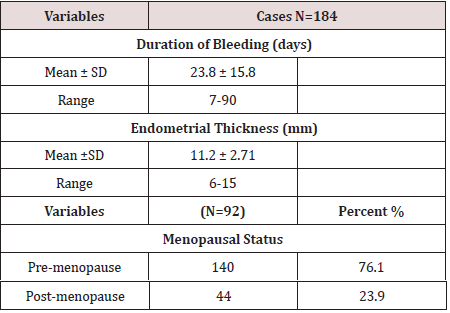
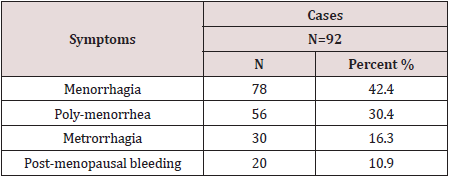
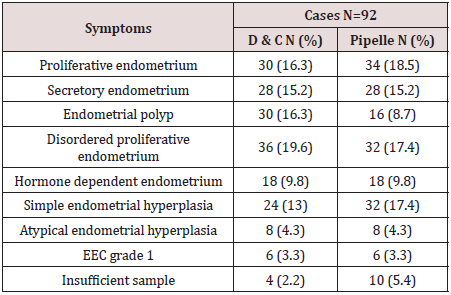
The mean of 54.8 years, parity of the studied group ranged from 0 to 5 times, and 48.9% of them were obese and 31.5% were overweight (Table 1). The mean duration of bleeding ranged from 7 days up to 90 days with mean of 23.8 days, endometrial thickness of the studied group ranged from 6 to 15mm, and 76.1% of them were pre-menopause (Table 2). The most common presented symptoms among the studied group was menorrhagia among 42.4% of them, then 30.4% presented with poly-menorrhagia and 16.3% with metrorrhagia (Table 3). The results of D & C and pipelle device, they were matched in detection of secretory endometrium, hormone dependent endometrium, atypical hyperplasia and EEC grade 1, while there was over estimation of positive proliferative endometrial cases and simple hyperplasia by pipelle device (18.5% and 17.4% versus 16.3% and 13% respectively by D&C), also it miss cases of endometrial polyp and disordered endometrial hyperplasia (8.7% and 17.4% versus 16.3% and 19.6% respectively by D& C) (Table4).
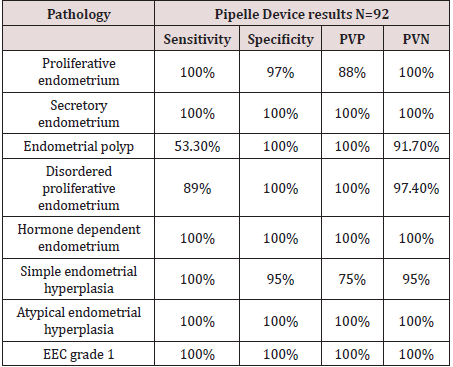
The sensitivity of pipelle sampling was 100% in detecting proliferative, secretory, hormonal dependent endometrium, simple and atypical hyperplasia and EEC grade 1, while it was 89% for the detection of disordered endometrium and 53.3% only for detection of polyp (Table 5).
Discussion
Abnormal bleeding is the presenting sign in more than 90%
of perimenopausal women with cancer of the endometrium [7].
Endometrial cancer is the sixth most common malignant neoplasm
in women worldwide and is the most common gynecologic
malignancy in developed countries [8]. Therefore, the management
of AUB needs to be undertaken seriously. There are many methods of
endometrial assessment in patients with abnormal uterine bleeding,
including ultrasonography, D&C, office-based methods, including
hysteroscopic biopsy or endometrial samplers such as suction
pipelle [6].The D & C is the most conventional method of endometrial
sampling which is in vogue since many decades. Though, it offers a
high degree of sensitivity in diagnosis of endometrial lesions, the
associated surgical risks, postoperative pain, higher costs due to
hospitalization and anesthesia have necessitated the search for
a suitable substitute which is simpler, cheaper, non-invasive, free
of complications and offers good diagnostic accuracy [6]. The
advent of non-invasive office procedures like pipelle endometrial
sampling has posed a challenge to the whole range of conventional
invasive techniques. It is now widely accepted by the clinicians and
patients, since Its safe and economical. It can sample about 5-15%
of the total endometrial surface area. It is especially useful in global
lesions involving in large surface area of the endometrium than in
focal lesions [7]. Hence, our study was proposed to evaluate the
efficacy of Pipelle sampling in diagnosing endometrial pathologies
in comparison with gold standard D and C method. The aim of this
study was to Compare between the histopathological findings of
pipelle endometrial biopsy and D&C biopsy (the gold standard).
Regarding the clinical features of the study population; we work
on 184 cases their age was ranged from 44 years up to 66 years
with mean of 54.8 years, their parity is ranged from 1 to 5 with
mean of 1.8, and according to BMI, 36 cases (19.6%) were normal
(BMI; 18-25), 58 cases (31.5%) are overweight (BMI; 25-30) and
rest of cases (90 case, 48.9%) are obese (BMI: more than 30) from
that it seems that most of patients were obese. In comparison with
a study performed in Iran by Moradan et al., 2015 on 130 patients,
similar data have been observed, as the mean age of the study
group was 46.19 years. The mean parity was 2.9 ranging from 1 to 5
time [9,10]. Our data is also agreed with data obtained from a study
performed in Kuwait by Abdelazim et al. [11] on 143 cases as it
shows that, the mean age of the study group was 46.3 years ranging
from 40 to 49. The mean parity was 4.7 ranging from 1 to 6 time.
Regarding to menopausal state of our studied group, most of cases
were pre-menopause with percentage of 76.1%, the rest of cases
were post-menopause. It was to somehow consistent with that in
another study as the percentage of pre- menopause was 62.3%.
The most common presenting symptoms among our studied
group was menorrhagia 78 cases (42.4%), 56 cases (30.4%)
presented with Polymenorrhea, 30 cases (16.3%) presented
with metrorrhagia and finally 20 cases (10.9%) presented with
Post-menopausal bleeding [9]. There were slight differences
in the percentage of the common presentation among patients
included in the above study as Menorrhagia was the most common
presenting complaint seen in 116 cases (55.24%), but against to
our findings it was followed by metrorrhagia in 48 (22.86%) cases,
then Polymenorrhagia in 28 (13.33%) cases and postmenopausal bleeding in 18 (8.57%) cases. In comparison with the study by
Abdelazim et al. [11]. the presenting symptoms were menorrhagia
37%, poly-menorrhagia 25.8%, metrorrhagia 18.1% and Postmenopausal
bleeding 16.7%, like our results.
In our study tissues obtained for histopathology were mostly
enough in both methods, sample sufficiency was 97.9% for D & C
as there were only 4 insufficient samples while in pipelle sampling
it was 94.6%, 5 samples are in insufficient. In comparison with
the study by Alliratnam AS et al. [12] Sample sufficiency was 96%
for D & C versus 93% for Pipelle. While in Moradan et al., 2015
study 84.6% of the samples obtained by Pipelle and 90% of those
obtained by D& C were enough. Similar results have been observed
in Abdelazim et al. [11]. study, Sample sufficiency was 100% for D
& C versus 97.9% for Pipelle.
Also, similar results were reported in a study by Naderi et al.
[13] the sufficiency rates were 91.6% and 98.3% by Pipelle and
D & C respectively. Regarding pathology of endometrial tissue
obtained by D&C and pipelle; our study showed that, the 2 methods
were matched in detection of secretory endometrium, hormone
dependent endometrium, atypical hyperplasia and EEC grade 1,
while there was over estimation of positive proliferative endometrial
cases and simple hyperplasia by pipelle device (18.5% and 17.4%
versus 16.3% and 13% respectively by D&C), also it miss cases of
endometrial polyp and disordered endometrial hyperplasia (8.7%
and 17.4% versus 16.3% and 19.6% respectively by D&C).
The results of endometrial sampling were also to somehow
similar to Alliratnam et al. (12). study, Histopathological
examination revealed that both methods agreed in all cases of
secretory endometrium and adenocarcinoma, and there was over
estimation of positive in diagnosis of proliferative endometrium
by pipelle device, only 1 missed case by pipelle in diagnosis of
disordered endometrium, but it failed to diagnose any case of
endometrial polyp, thus polyp is rarely to be detected by pipelle in
this study and proliferative endometrium is the commonest cause
of peri-menopausal bleeding in this study.
In Moradan et al., 2015 study, the pipelle missed only few
cases in diagnosis of secretory endometrium and endometrial
hyperplasia without atypia (27.7% and 16.9% versus 28.5% and
18.5% by D&C), but they were agreed in diagnosis of malignant
endometrium, and pipelle positively overestimated the diagnosis
of proliferative endometrium [10]. The results were similar to
Abdelazim et al[11]. study who found that there was positive
correlation between 2 methods in diagnosis of proliferative
endometrium, secretory endometrium, endometrial hyperplasia
with atypia and malignant endometrium, but the pipelle missed the
diagnosis of some cases of endometrial hyperplasia without atypia
and endometrial polyps (34.3% and 2.1% versus 31.4% and 0.7%
by D&C). Our study disagrees with Demirkiran et al. [14]. study on
478 patients. Histopathological examination of D & C biopsy showed
normal endometrium in 330 cases (69%) , hyperplasia in 21 cases
(4.4%), hyperplasia with atypia in 20 cases (4.2%), focal lesions in
89 cases (18.6%) , atrophy in 9 cases (1.9%) and insufficient in 9
cases (1.9%), while Pipelle method showed; normal endometrium
in 356 cases (74.5%) , hyperplasia in 22 cases (4.6%) , hyperplasia
with atypia in 18 cases (3.8%),focal lesions in 59 cases (12.3%),
atrophy in 7 cases (1.5%) and insufficient in 16 cases (3.3%).
Regarding validity; Our study showed good agreement between
Pipelle and D&C in detection of endometrial abnormalities; the
sensitivity of pipelle sampling was 100% in detecting proliferative,
secretory, hormonal dependent endometrium, simple and atypical
hyperplasia and EEC grade 1, while it was 89% for the detection of
endometrium disorders and 53.3% only for detection of polyp.
In support of our finding’s validity of Pipelle in Alliratnam et
al. [12] study was as following; Pipelle has sensitivity of 100%
in proliferative endometrium, secretory endometrium and
Adenocarcinoma, while it had 90% sensitivity in disordered
proliferative endometrium diagnosis and only 16% in endometrial
polyp detection .Similar results have been observed in Moradan et
al., 2015 study as following; pipelle has sensitivity in proliferative
endometrium (94.4%), secretory endometrium (97.4), simple
endometrial hyperplasia without atypia (92.3%), endometrial
cancer (100%) and atrophic endometrium (50%) (10).
Our results are also consistent to somehow with Abdelazim
et al. [11] study results as pipelle showed sensitivity of 100% in
proliferative endometrium, secretory endometrium, endometrial
hyperplasia and endometrial carcinoma and only 60% in
detection of endometrial polyp . On the other hand, the current
study disagrees with Demirkiran et al. [14]. In the detection of
endometrial hyperplasia, which was lower than our study, they
reported a sensitivity level of 67% for Pipelle biopsy. The source of
discrepancies is the recognition of different age groups as criteria
for inclusion in this and another research. The other probable cause
is difference in curette and Pipelle that is used by different studies.
Conclusion
With regard to the facility to perform sampling as an outpatient procedure and without anesthesia and with short duration and less cost, it is recommended that this device be used instead of D & C. lesion like polyps and focal lesions may missed by pipelle. Negative biopsy must therefore be followed in a symptomatic patient by other diagnostic methods such as D&C or hysteroscopy.
References
- (2010) International Journal of Gynecological Pathology 9(2):117-21.
- Matthews ML (2015) Abnormal uterine bleeding in reproductive-aged women. Obstet Gynecol Clin North Am 42 (1): 103-115.
- Khrouf M Terras K (2014) Diagnosis and Management of Formerly Called "Dysfunctional Uterine Bleeding" According to PALM-COEIN FIGO Classification and the New Guidelines. J Obstet Gynaecol India 64(6): 388-393.
- Munro MG, Critchley HOD, Fraser IS (2018) The two FIGO systems for normal and abnormal uterine bleeding symptoms and classification of causes of abnormal uterine bleeding in the reproductive years: 2018 revisions. Int J Gynaecol Obstet 143(3): 393-408.
- Berek JS, Berek DL (2012) Berek & Novak’s Gynecology. Pp: 374-431.
- Barbara L Hoffman MD, John O (2016) Williams GYNECOLOGY.
- (2018) The role of transvaginal ultrasonography in evaluating the endometrium of women with postmenopausal bleeding. Obstet Gynecol 131(5): e124-e129
- Lortet-Tieulent J, Ferlay J, Bray F, Jemal A (2018) International Patterns and Trends in Endometrial Cancer Incidence. J Natl Cancer Inst 110(4): 354-361.
- Chandrashekar N, Jyothi GS, Shetty P (2017): Pipelle endometrial biopsy vs dilatation and curettage to diagnose endometrial diseases in abnormal uterine bleeding. International Journal of Gynecological Pathology 9(2): 117-21.
- Sanam M, Majid MM (2015) Comparison the Diagnostic Value of Dilatation and Curettage versus Endometrial Biopsy by Pipelle - a Clinical Trial. Asian Pac J Cancer Prev 16(12): 4971-4975.
- Ibrahim Anwar Abdelazim, Amro Aboelezz, Amr Fathy (2013) Pipelle endometrial sampling versus conventional dilatation & curettage in patients with abnormal uterine bleeding. J Turk Ger Gynecol Assoc 14(1): 1-5.
- Alliratnam AS, Senthil Priya S, Shankar R (2016) Diagnostic value of pipelle endometrial sampling in comparison with dilatation and curettage among patients with abnormal uterine bleeding The New Indian Journal of OBGYN 3(1): 4-8.
- Naderi T, Asharafganjooie T, Bahrampoor A, (2006) Comparison of the diagnostic accuracy of pipelle biopsy, dilatation and curettage and hysrectomy in detection of endometrial lesions. J Kerman University Med Sci 13:159-63.
- Demirkiran F, Yavuz E, Erenel H, Bese T, Arvas M, et al. (2012) Which is the best technique for endometrial sampling? Aspiration (pipelle) versus dilatation and curettage (D&C). Arch Gynecol Obstet 286(5):1277-1282.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...