Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Research Article(ISSN: 2637-4544) 
Effectiveness of Hayman’s Compressive Suture in the Management of Postpartum Hemorrhage Volume 3 - Issue 4
Franklin José Espitia De La Hoz*1, Diana Marcela Echeverri Muñoz2, Johny Alexander Enríquez Mogollón3 and Gloria Stefany Fernández Cabrera2
- 1 Especialista Ginecología y Obstetricia, Universidad Militar Nueva Granada, Colombia
- 2 Médica General, Universidad del Quindío, Colombia
- 3 Médico General, Universidad Tecnológica de Pereira, Colombia
Received:July 11, 2019; Published: July 22, 2019
Corresponding author:Franklin José Espitia De La Hoz, Especialista Ginecología y Obstetricia, Universidad Militar Nueva Granada, Colombia
DOI: 10.32474/IGWHC.2019.03.000166
Abstract
Objective: To evaluate the effectiveness of Hayman’s compressive sutures, as a conservative treatment, in the control of postpartum hemorrhage (PPH).
Materials and methods: An observational, retrospective, cross-sectional and descriptive study was carried out, the clinical records were reviewed, and all the patients who had been subject to Hayman’s compressive sutures, due to postpartum hemorrhage resistant to pharmacological treatment were analyzed. The women received care between January 2009 and December 2018 in a third level private institution in Armenia (Quindío, Colombia). Women who suffered postpartum obstetric hemorrhage (vaginal and cesarean section), who did not respond to pharmacological management in the first 6 hours of puerperium were included. Women whose deliveries did not take place in the clinic, with a dead fetus or who did not have data on the selected variables were excluded. For data analysis, percentage frequencies, mean, median, ranges and averages ± standard deviation were used. The processing and analysis of the data was done with the statistical package SPSS version 22.0.
Results: The mean age of the participants was 24.31 ± 5.76 years. Of 17724 deliveries, 10701 (60.37%) were by caesarean section. There were 687 (3.87%) cases of postpartum obstetric hemorrhage (cesarean section: 61.57% and delivery: 38.42%). The main cause was uterine atony (78.16%). Of the 687 women with postpartum obstetric hemorrhage, this was resolved with medical management in 72.92%. Compressive hemostatic suture was indicated in 13.24% (n = 91/687) of the cases, of which 86.81% (n = 79/91) responded satisfactorily. The average surgical time was 4.96 ± 1.03 minutes (range between 3 and 8). No complications derived from the procedure were documented.
Conclusion: Hayman’s hemostatic compressive sutures are an adequate conservative option, in the presence of postpartum hemorrhage refractory to pharmacological treatment, demonstrating its therapeutic effectiveness with admirable results.
Keywords: Postpartum hemorrhage; Sutures; Caesarean section; Pharmacotherapy; Hysterectomy
Introduction
Postpartum hemorrhage is the most common form of obstetric hemorrhage and is the leading cause of maternal morbidity and mortality in the world [1,2]. It is defined as blood loss estimated in more than 500mL in the first 24 hours after vaginal delivery, and greater than 1000mL after a cesarean, or decrease in the hematocrit level of 10% (3); or the blood loss that causes hemodynamic involvement in the postpartum [3], making it necessary to transfer blood products [1,4].
Postpartum hemorrhage is the most common form of obstetric hemorrhage and the leading cause of maternal morbidity and mortality in the world [1,2]. It is defined as blood loss estimated in more than 500mL in the first 24 hours after vaginal delivery, and greater than 1000mL after a cesarean section, or 10% decrease in the hematocrit level [3]; or blood loss that causes hemodynamic involvement in postpartum that require the transfer of blood products [1,4].
Postpartum hemorrhage (PPH) occurs in 2 to 4% of deliveries and in 6 to 7% of cesarean sections [5]. It has been calculated that 140,000 women worldwide die every year, due to causes associated with PPH [3]. In Latin America and the Caribbean, it causes 13.3% of maternal deaths, and in Colombia the percentage rate is 23% [6], with a rate of approximately 40 maternal deaths per 100,000 live births. This places us somewhere between the United States reports (12 per 100,000 live births) and African reports (300 per 100,000 live births).
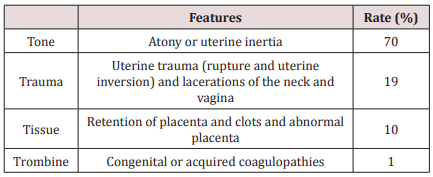
The causes of HPP have been simplified with the "4T” mnemonic [7], looking for an easy way to remember them (Table 1). Multiple risk factors for PPH have been identified: chorioamnionitis, multiple pregnancies, prepartum haemorrhage, fetal macrosomia, maternal obesity, preeclampsia, maternal anemia, primigravidae and extended labor [8], among others.
The diagnosis is established whenever hemorrhage generates a hemodynamic involvement during the postpartum [1]. It is classified as: Primary (immediate), if it occurs within the first 24 hours postpartum. Secondary (late): occurs after 24 hours and up to 6 weeks after postpartum [9].
The treatment of PPH involves finding and ceasing the cause as soon as possible. Management includes pharmacological options (oxytocin, ergot alkaloids, prostaglandins, tranexamic acid, etc.) and non-pharmacological options (manual massage, selective arterial embolization, arterial ligation, uterine tamponade, uterine compression sutures and hysterectomy) [1,8,10].
The uterine compression sutures, for the control of PPH, are useful in cases in which bleeding secondary to uterine atony cannot be controlled, and there is the desire to preserve the reproductive capacity. Dr. Christopher B-Lynch [11] was the first one to successfully describe this method, later some modifications were made to the original technique, all of which have been used, with greater or lesser advantages and disadvantages. These include Hayman uterine compression sutures [12], Cho [13]and Ohuahba [14], among others. The results are variable, but mostly satisfactory, according to the technique used.
Hayman's compression sutures are a simplified approach to the B-Lynch technique compression sutures [12], it includes slight modifications. The advantages offered are the ease and speed of application, in addition to avoiding the need to perform a hysterectomy of the uterine segment when PPH follows a vaginal delivery, which minimizes trauma in the bleeding of the uterus.
The objective of this study is to evaluate the effectiveness of Hayman's compressive sutures, as a conservative treatment, in the control of postpartum obstetric hemorrhage in patients of a highly complex private institution in Armenia, Quindío (Colombia).
Materials and Methods
An observational, retrospective, cross-sectional and descriptive study was carried out; the clinical histories were reviewed, and all the patients had Hayman's compressive sutures, for drug resistant PPH were analyzed. The patients were treated between January 1, 2009 and December 31, 2018 in a third level private institution in Armenia (Quindío, Colombia), which takes care of the population from private and state sponsored health care plans. We included women with postpartum hemorrhage (vaginal or cesarean section), who did not respond to pharmacological treatment during the first 6 hours of puerperium. We excluded women whose deliveries did not take place to in the clinic, with a dead fetus or who did not have data on the selected variables.
Process
The cases with postpartum hemorrhage (vaginal or cesarean section) were identified in the registry: Epidemiological Surveillance System (SIVIGILA). Once identified, the clinical histories were reviewed. A compilation of the data was made, and the cause of the postpartum obstetric hemorrhage was compiled, furthermore, patients with insufficient or incomplete information were contacted by telephone or visited.
Surgical technique
For all participating women, the technique was performed in accordance to what was originally described by Hayman RG et al. [12]. Through an exploratory laparotomy the uterus is exteriorized and rectified, then it is compressed manually, and compressive sutures are performed. A transfixion point (synthetic absorbable suture of polyglactin 910 # 1) is applied, with a straight needle, from the anterior to the posterior side, at the level of the uterine segment (3 to 4cm medial to the lateral border of the uterus). The suture is directed towards the uterine fundus, and is knotted at the antero-superior level, while the assistant executes a sustained and energetic uterine compression. The suture is made on each side of the uterus (one on the right side and one on the left side: parallel reins), it is important to try to maintain the tension in the same way on both sides.
Measured variables
Socio-demographic characteristics were measured (age, occupation, level of education, marital status, race, origin, social security affiliation, religion); weight, height, BMI; habits (smoking, alcohol intake, consumption of psychoactive substances); sexual and reproductive health (age of menarche, age of onset of sexual activity, age of first pregnancy, age of first birth, parity, gestational age, type of delivery). A descriptive analysis was made of the operative time of the sutures, calculated bleeding, complications, cause and risk factors of PPH, hospital stay, transfusions and evolution of the patients. Information on prenatal care (prenatal care, number of prenatal check-ups, uterine height, hemoglobin concentration (g/dL) of the last prenatal check-up and warning signs recorded in the perinatal card: medical history, diseases associated with pregnancy: anemia, hypertension , preeclampsia, diabetes, hypothyroidism, gestational urinary tract infection, history of postpartum hemorrhage), gestational age at the time of delivery (in weeks), induction of labor, birth pathway, episiotomy and neonatal weight.
Statistical analysis
A database was built in Excel. For data analysis, we used percentage frequencies, mean, median, ranges and averages ± standard deviation. The processing and analysis of the data was done with the statistical package SPSS version 22.0.
Ethical aspects
The study was presented at institution where it was carried out, following the recommendations of the Declaration of Helsinki; having been approved by the Ethics Committee prior to its execution.
Results
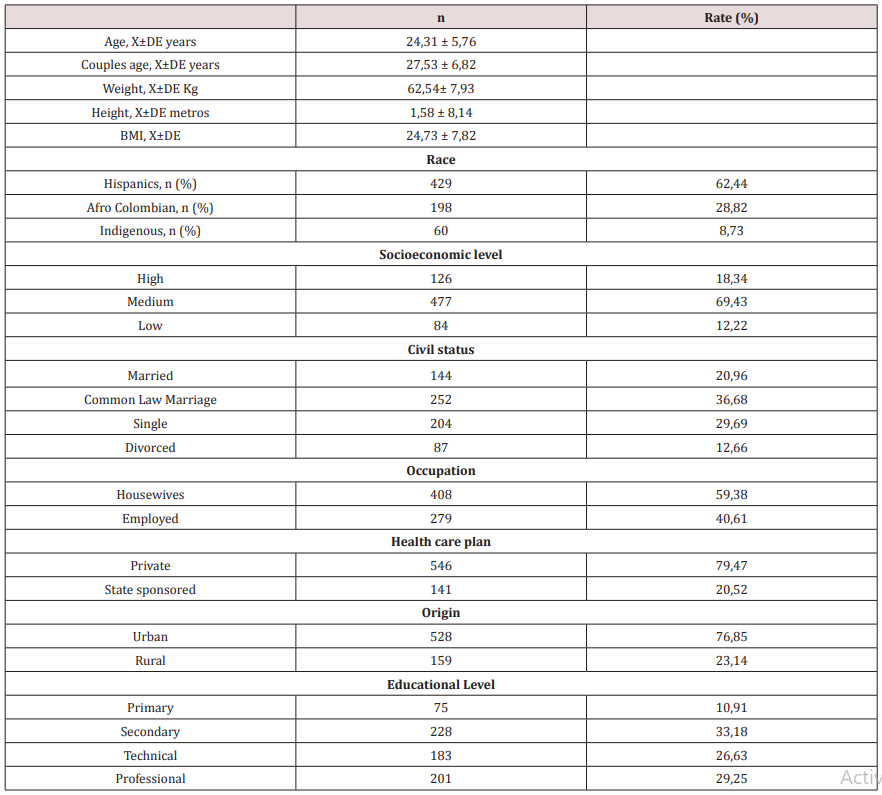
The mean age was 24.31 ± 5.76 years; being the group with higher frequencies between 18 to 29 years old (69. 31%). The population was characterized by being Hispanic, housewives, middle class, common law marriage, secondary school educational level, urban dwellers and belonging to the private health care program. 89.95% were Catholic, 19.21% were habitual smokers, and 86.46% consumed alcohol on a regular basis. 7.49% reported being frequent users of psychoactive substances. 27.51% were obese. The socio-demographic characteristics are described in Table 2.
Of a participating population of 17.724 deliveries in 10 years, 10.701 (60.37%) were done by cesarean section. There were 687 (3.87%) cases of PPH (caesarean section: 61.57% and delivery: 38.42%). 19.65% (n = 135/687) had more than 5 deliveries, 17.46% (n = 120/687) had had 3 or more caesarean sections and 16.59% had had at least one delivery after the cesarean section (Table 2).
The history of sexual and reproductive health offered the following data: the age of menarche was 13.72 ± 2.51 years (range between 10 and 19); the initiation of sexual activities was at 16.57 ± 2.38 years (range between 12 and 27). The age of the first pregnancy was at 16.59 ± 2.49 years (range between 13 and 42). The age of first childbirth was at 17.85 ± 2.71 years (range between 13 and 41). >For deliveries, it was found that 77.97% were multiparous; with a median of 3 children [(2 vaginal deliveries and 1 via cesarean section per woman), (range between 1 and 9 children)]. The multiparous to single delivery ratio was 3:1; 66.81% had had more than three pregnancies; 80.78% said that their first pregnancy was unplanned. 9.17% stated that the first pregnancy had been the result of a sexual intercourse under the influence of alcohol and without a condom. The prevalence of abortions was 16.15%, of which 1/3 were induced and performed under risky conditions (use of self-formulated drugs or in clandestine sites). 47.49% had a prior caesarean section, and 38.99% had undergone at least one episiotomy.
Regarding prenatal control, 68.17% had a median of 4 controls (range between 0 and 9). 86.93% were seen by the specialist on at least one occasion 26.98% were classified as having high obstetric risk. 81.97% had completed, correctly, the prenatal control card.
Regarding gestational age, it was observed that 87.37% of the patients underwent full-term labor, with a median of 39 weeks (range between 37 and 42). The uterine height showed an average of 34.17 ± 3.58 cm. Most cases of PPH occurred (73.81%) in women with preterm delivery. The average weight of the neonates was 3.425 ± 298 grams (range between 895 and 5.179 grams).
The majority (81.14%) of the women had hemoglobin levels compatible with anemia (hemoglobin less than 11 g/dL), according to the World Health Organization (WHO) criteria [15]. 27.99% had received at least one treatment for urinary infection. Hypothyroidism was detected in 23.59%, followed by preeclampsia (12.15%) and gestational diabetes (7.19%).
Among the main causes of PPH, uterine atony (78.16% / n = 537) stands out as the first, followed by traumatisms of the soft birth canal (14.84% / n = 102), retention of placental remains and abnormal placentation (6.11% / n = 42) and coagulopathies (0.87% / n = 6).
In the risk factors found prolonged labor (19.65%), followed by hypertensive disorders of pregnancy (17.46%) and multiparity (16.59%), the others are detailed in the Table 3. In the population of 687 women with PPH, this was resolved with medical management in 72.92% (n = 501); 5.96% (n = 41) required additional uterine tamponade (artisanal Bakri balloon) to control bleeding; 20.96% (n = 144) required surgical management: hemostatic compressive sutures (n = 91 / 13.24%), vascular suture (n = 31 / 4.51%) and obstetric hysterectomy (n = 23/3, 43%) (Table 3).
The surgical technique of Hayman's compressive sutures had an average surgical time of 4.96 ± 1.03 minutes (range between 3 and 8 minutes). The average of quantified bleeding in the group was 1475.39 ± 716.82mL (range between 950 and 3250mL). 85.58% of the patients required the administration of blood products, and 28.57% (n = 26/91) required admission to the ICU. The length of hospital stay was 2.14 ± 1.03 days (range between 2 and 5 days). The analgesic doses administered from the surgical procedure to the hospital discharge, on average were 7.41 ± 2.58 (range between 7 and 23 doses). No complication was documented due to the technique of compressive sutures, there was no need to reiterate, and no deaths occurred.
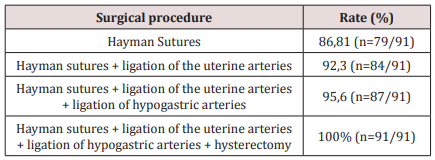
Adequate compression of the uterus and hemorrhage control with sutures was achieved in 86.81% (n = 79/91), where it was not necessary to perform any other surgical procedure in an additional way. In 5.49% (n = 5/91) the selective ligature of the uterine arteries was added; in 3.29% (n = 3/91) it was required to add the ligature of hypogastric arteries, and in 4.39% (n = 4/91) obstetric hysterectomy was the solution for the control of bleeding (Table 4). No difference was found in the satisfactory response according to the route of delivery (vaginal versus cesarean section).
Discussion
This study found an incidence of postpartum hemorrhage of 3.87% (n = 687/17724), being more frequent in caesarean section (61.57%) compared to vaginal delivery (38.42%). 72.92% of the 687 PPH were resolved with medical management. The main cause was uterine atony (78.16%) and prolonged labor (19.65%) was highlighted in the risk factors. The hemostatic compressive suture of Hayman was indicated in 13.24% (n = 91/687) of the cases, where 86.81% (n = 79/91) responded satisfactorily. The average surgical time was 4.96 ± 1.03 minutes. The 4.39% (n = 4/91) of the women merited the accomplishment of the hysterectomy for the control of the bleeding.
The results of the incidence of this study are superior to those reported by López et al. [16] in Bogotá, Colombia, in the year 2017, who report an incidence of 2.1%, and similar to 3.2% found in a rural area of central India, by Bang et al. [17]; but less than 7.2% in Oceania and 25.7% in Africa, published by Calvert et al. [18]. The risk factors of this investigation match those reported by Kramer MS et al. [19] in Montreal, Canada, in the year 2017, that included maternal age ≥35 years, multiple pregnancy, uterine myomatosis and preeclampsia.
Fernández et al. [20]in Mexico, in the year 2017, reported an obstetric hemorrhage rate of 2.4%, where they describe uterine atony as the main cause with 36.2%, which is lower than that found in the present study; nevertheless, placental accreta (32.7%) and placenta previa plus placental accreta (12%) replaced uterine atony as the first cause of PPH.
Regarding the effectiveness of Hayman's compressive sutures, our results are inferior to those published by Nanda S et al. [21] in Haryana, India, which indicate 93.75%, however, it was a group of only 48 women; but close to 90.9% of the success rate described in Varese, Italy, by Ghezzi et al. [22], in a group of 11 women; and are above 76% reported in Colombo, Sri Lanka by Marasinghe JP et al. [23] in a group of 17 women, or in Egypt by Fahmy et al. [24]which reports 64.63% in a series of 53 women, and similar to those of Majumdar A et al. [25] in India (83.72%) in 43 cases.
It is not uncommon for complications to be described with the use of uterine compression sutures. In our study, we did not report any complications, however, Hayman RG et al. [12] emphasized that unequal tension could be complicated by segmental ischemia. Akoury H et al. [26] in 2008, in Toronto, Canada, described a case of myometrial necrosis; On the other hand, Jamard A et al. [27] in 2014, in France, followed by hysteroscopy to 19 patients, who underwent uterine compression sutures, they found 16% with uterine synechia and 16% with placental retention.
Regarding the need for obstetric hysterectomy to control bleeding, in case of failure of the Hayman technique, our results are similar to the 4.87% reported by Fahmy MS et al. [24] in 2016, in Upper Egypt in 82 women. The surgical time reported in this study is lower than the 5.1 ± 0.9 minutes described by Moreno et al. [28] in Mexico, in a group of 87 women; as well as to that reported by Ghezzi et al. [22] and Majumdar et al. [25].
The study by Rubio et al. [29] recommends that, in the usual conditions of daily practice, the first approach, and therefore, the earliest for the diagnosis of abnormal postpartum hemorrhage, is the visual estimation with a point of established cut of 800mL, for the start of the hemorrhage control maneuvers, since the presence of signs of hemodynamic decompensation occur with bleeding near this volume; in such a way that, from there, therapeutic maneuvers are oriented.
The management of PPH, resistant to pharmacological treatment, requires conservative procedures that preserve the uterus, in addition to being cost-effective, and that can be used in emergency situations, and even by obstetricians who lack the training and skill necessary for the treatment. carrying out more complex interventions, this is where Hayman's technique becomes important.
We highlight the reduced number of the sample as weaknesses of this study, and that there was no comparison of the results with the B-Lynch technique, the pioneer in the techniques of compressive sutures for the treatment of postpartum obstetric hemorrhage. Among the strengths of this research, we point out that it is the first study of these characteristics carried out in the country; the other thing is that, because of the results, as well as the speed and simplicity of the technique, in addition to not requiring hysterotomy, or undoing previous hysterography, or the involvement of complex sutures, is available to any surgeon, with a minimum of experience, making it easily reproducible in any scenario.
Conclusion
Hemostatic compressive sutures of Hayman are an adequate conservative option, in the presence of postpartum obstetric hemorrhage, resistant to pharmacological treatment, managing to demonstrate its therapeutic effectiveness and conserving reproductive capacity. In the hands of surgeons without expertise, compressive sutures are safe, achieving satisfactory results with minimal or no complications. The effectiveness of the Hayman suture is such that hysterectomy could be avoided in 95.6 of the women with postpartum obstetric hemorrhage.
Acknowledgement
Our gratitude to the women who allowed us to complete the necessary information to achieve the results of this research; and my beloved wife, Dr. Lilian Orozco Santiago, for her permanent support in all my academic projects.
References
- Espitia De La Hoz FJ, Zuluaga Cortés OE, Orozco Santiago L (2016) Ligadura de arterias hipogástricas en hemorragia postparto severa. Rev CES Med 30(1): 26-34.
- World Health Organization (2012) WHO recommendations for the prevention and treatment of postpartum haemorrhage.
- American College of Obstetricians and Gynecologists (2006) ACOG Practice Bulletin: Clinical Management Guidelines for Obstetrician-Gynecologists Number 76, October 2006: postpartum hemorrhage. Obstet Gynecol 108: 1039-1047.
- Cabrera S (2010) Hemorragia Posparto. Rev Per Ginecol Obstet 56: 23-31.
- Say L, Chou D, Gemmill A, Tunçalp Ö, Moller AB, et al. (2014) Global causes of maternal death: A WHO systematic analysis. Lancet Glob Health 2: e323-e333.
- Representantes del Grupo Desarrollador de la Guía (2013) Guía de práctica clínica para la prevención y el manejo de la hemorragia postparto y complicaciones del choque hemorrá Rev Colomb Obstet Ginecol 64: 425-452.
- Lalonde A, International Federation of Gynecology and Obstetrics (2012) Prevention and treatment of postpartum hemorrhage in low-resource settings. Int J Gynecol Obstet 117(2): 108-118.
- Mousa HA, Blum J, Abou El Senoun G, Shakur H, Alfirevic Z (2014) Treatment for primary postpartum haemorrhage. Cochrane Database Syst Rev 13(2): CD003249.
- Patel A, Goudar SS, Geller SE, Kodkany BS, Edlavitch SA, et al. (2006) Drape estimation vs. visual assessment for estimating postpartum hemorrhage. Int J Gynaecol Obstet 93(3): 220-224.
- WOMAN Trial Collaborators (2017) Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post-partum haemorrhage (WOMAN): an international, randomised, double-blind, placebo-controlled trial. Lancet 389(10084): 2105-2116.
- B Lynch C, Coker A, Lawal AH, Abu J, Cowen MJ (1997) The B-Lynch surgical technique for the control of massive postpartum haemorrhage: an alternative to hysterectomy? Five cases reported. Br J Obstet Gynaecol 104(3): 372-375.
- Hayman RG, Arulkumaran S, Steer PJ (2002) Uterine compression sutures: surgical management of postpartum hemorrhage. Obstet Gynecol 99(3): 502-506.
- Cho JH, Jun HS, Lee CN (2000) Hemostatic suturing technique for uterine bleeding during cesarean delivery. Obstet Gynecol 96(1): 129-131.
- Ouahba J, Piketty M, Huel C, Azarian M, Feraud O, et al. (2007) Uterine compression sutures for postpartum bleeding with uterine atony. BJOG 114(5): 619-622.
- Espitia F, Orozco L (2013) Anemia en el embarazo, un problema de salud que puede prevenirse. Méd UIS 26(3): 45-50.
- López García LF, Ruiz-Fernández DP, Zambrano-Cerón CG, Rubio-Romero JA (2017) Incidencia de hemorragia posparto con base en el uso terapéutico de uterotó Resultados maternos en un hospital de mediana complejidad de Bogotá, Colombia. Rev Colomb Obstet Ginecol 68(3): 218-227.
- Bang RA, Bang AT, Reddy MH, Deshmukh MD, Baitule SB, et al. (2004) Maternal morbidity during labour and the puerperium in rural homes and the need for medical attention: A prospective observational study in Gadchiroli, India. BJOG 111(3): 231-238.
- Calvert C, Thomas SL, Ronsmans C, Wagner KS, Adler AJ, et al. (2012) Identifying regional variation in the prevalence of postpartum haemorrhage: a systematic review and meta-analysis. PLoS One 7(7): e41114.
- Kramer MS, Berg C, Abenhaim H, Dahhou M, Rouleau J, et al. (2013) Incidence, risk factors, and temporal trends in severe postpartum hemorrhage. Am J Obstet Gynecol 209(5): 449.e1-7.
- Fernández Lara JA, Toro Ortiz JC, Martínez Trejo Z, De la Maza Labastida S, Villegas Arias MA (2017) Tasa de hemorragia, histerectomía obstétrica y muerte materna relacionada. Ginecol Obstet Mex 52(4): 247-253.
- Nanda S, Singhal SR (2011) Hayman uterine compression stitch for arresting atonic postpartum hemorrhage: 5 years experience. Taiwanese Journal of Obstetrics and Gynecology 50(2): 179-181.
- Ghezzi F, Cromi A, Uccella S, Raio L, Bolis P, et al. (2007) The Hayman technique: a simple method to treat postpartum haemorrhage. BJOG 114: 362-365.
- Marasinghe JP, Condous G, Seneviratne HR, Marasinghe U (2011) Modified anchored B-Lynch uterine compression suture for post partum bleeding with uterine atony. Acta Obstet Gynecol Scand 90(3): 280-283.
- Fahmy MS, Kholef EF, Sobhy KM (2016) Hayman Uterine Compression Suture in Upper Egypt. Med J Cairo Univ 84(2): 257-263.
- Majumdar A, Mallick K, Vasava B, Desai KT, Dalal M (2012) A descriptive study on Hayman suture technique to control postpartum hemorhage. Sri Lanka Journal of Obstetrics and Gynaecology 34: 79-83.
- Akoury H, Sherman C (2008) Uterine wall partial thickness necrosis following combined B-Lynch and Cho square sutures for the treatment of primary postpartum hemorrhage. J Obstet Gynaecol Can 30(5): 421-424.
- Jamard A, Turck M, Chéret Benoist A, Dreyfus M, Benoist G (2014) Risk of uterine synechiae following uterine compression sutures during postpartum haemorrhage. Gynecol Obstet Fertil 42(10): 681-685.
- Moreno Santillán AA, Posadas Nava A, Martínez Adame LM, Celis González C (2018) Sutura compresiva de Hayman: experiencia de cuatro años. Ginecol Obstet Mex 86(9): 590-596.
- Rubio Romero JA, Guevara Cruz ÓA, Gaitán Duarte H (2010) Validez de la estimación visual como método diagnóstico de la hemorragia postparto severa en un hospital universitario. Bogotá. 2007. Rev Fac Med 58(3): 173-184.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...