Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Review Article(ISSN: 2637-4544) 
Determinants of Perceived Susceptibility to Cervical Cancer and the Uptake of Screening Services Among Women of Reproductive Age Attending UCH, Ibadan, Nigeria Volume 4 - Issue 2
Ajayi Ayodeji f1,2*
- 1Maxwell Opemipo Olubunmi, 2AJAYI Ayodeji Folorunsho, Department of Nursing (LODL)
- *Ladoke Akintola University of Technology, Ogbomoso, Nigeria
- 2Department of Physiology, Ladoke Akintola University of Technology, Ogbomoso, Nigeria
Received: November 16, 2020 Published: December 15, 2020
Corresponding author: Ayodeji Folorunsho Ajayi, PhD, Department of Physiology, Ladoke Akintola, University of Technology, Ogbomoso, Nigeria
DOI: 10.32474/IGWHC.2020.04.000187
Abstract
Background:The burden of cervical cancer and the perception of its susceptibility remains alarming. This study evaluates perceived susceptibility and utilization of Cervical Cancer Screening (CCS) services among women of reproductive age attending the Gynecology Clinic at University College Hospital (UCH) Ibadan, Nigeria.
Methods: The study adopted a quasi-experimental research design, and a semi-structured questionnaire was used to obtain data from the respondents. A total number of 228 respondents took part in this study with an age mean of 32.71. The data sourced from this study were subjected to descriptive and inferential statistical analysis methods. Descriptive statistics were used to establish the frequencies and percentages of responses while inferential statistics (regression analysis) was used to test the hypotheses.
Results: The findings show that 82.9% ever heard of CCS, 45% reported knowing the screening procedure, but only 22.4% ever undertook the screening. Also, perceived susceptibility had a significant effect on the uptake of CCS. Concerning perceived barriers to uptake of CCS, 32.8% reported a lack of information and 32.5% reported long distance. Perceived barriers, perceived benefits and cues to actions showed no significant influence on CCS uptake.
Conclusion: The findings showed a low level of knowledge about cervical cancer. Also, the level of knowledge had no significant influence on the uptake of CCS. Thus, the study recommends community-integrated cervical cancer screening program that will be available, accessible and affordable for all women regardless of their socio-economic status.
Keywords: Cervical cancer; Human Papilloma Virus; Pap smear; Reproductive age; Sexual intercourse
Introduction
The reproductive health needs of women are germane to
the health of the family as women carry out vital and numerous
responsibilities in the family. Their health is essential to their
functioning in the family. As a result, a woman is healthy as long
as diseases, organic disorders and deficiencies do not affect her
sexual and reproductive functions. [1] Cancer of the cervix is a
disease condition that is exclusive to women; it adversely affects
their sexual and reproductive health, general condition, and family
life. Cancer of the cervix is a major cause of death in developing
countries among reproductive-age women. [2] Globally, cancer of
the cervix takes the second position after breast cancer in terms
of most common cancer reported among women.[3] In 2008, the
worldwide record showed an estimate of 530,000 new cases of
cervical cancer and 275,000 deaths. However, developing nations
recorded 90% of these deaths. According to WHO (2015a), 2 and
the African region recorded around 75,000 new cases in 2008.
In Nigeria, reported new cases of diagnosis of cervical cancer is reported in about 10,000 women, while an estimate of 8,000 women dies as a result of cancer of the cervix in Nigeria annually [4,5]. A researcher opined that eight out every ten deaths due to cervical cancer take place in developing nations 5. Others found that cancer of the cervix was the foremost cause of gynecological cancers in the Northern part of the country, responsible for about 65.7% of all cases of gynecological cancer [6]. Annually, the report had it that 14,089 women have new cases of cervical cancer, and 8,240 deaths are documented in Nigeria. [7]
However, cancer of the cervix is an avoidable disease and has good prognosis at the latent pre-invasive stage. Thus, early diagnosis is the most appropriate means of preventing its development to an incurable stage of the disease. The screening involves examination like Papanicolaou test (Pap smear test) from age 21, with regular screening alternating from once per year up to once in five years as long as there is no abnormal result. [8] According to WHO (2006), [9] Pap smear test is a vital screening tool for early diagnosis of cancer of the cervix, and it has been reported to be very effective in reducing susceptibility to the disease. The significance of Pap smear screening in reducing the susceptibility to cervical cancer and mortality in developed countries like Finland, United States, United Kingdom and Sweden with national screening programs is well established. [10]
Researchers reported that 47.72 million women in Nigeria are susceptible to cervical cancer. [11] They also estimated that the country would be documenting around 19,440 new diagnoses of cervical cancer and 10,991 deaths by the year 2025. Although making use of cervical cancer screening to reduce susceptibility to the disease is very low in Nigeria [12]. WHO (2012) [13] similarly reported that the response of women to utilize cervical cancer screening in Nigeria is low in comparison to the effort involved in promoting cancer screening. It buttresses the fact that awareness of cervical cancer among women in Nigeria is still shallow; therefore, it is crucial to improve the dissemination of health education in this aspect. Poor health education is still a significant factor that discouraged women from undertaking cervical cancer screening [14]. Using the Health Belief Model (HBM), this study evaluates factors influencing perceived susceptibility to cervical cancer and uptake of screening services among women of reproductive age attending the University College Hospital Ibadan, Nigeria.
Methods
Research Design
The study adopted a Quasi-experimental research design. It assessed respondents’ knowledge and perceived susceptibility, benefits, barriers, severity and cues to action on cervical cancer and uptake of screening services among women of reproductive age attending the gynecological clinic at University College Hospital (UCH), Ibadan, Nigeria.
Study Setting
University College Hospital (UCH), Ibadan is situated in Ibadan North Local Government Area of Oyo State, Nigeria. Established in 1957 as the foremost Federal Tertiary Hospitals in the country and a referral centre. The health institution is made up of 16 clinical and six non-clinical Departments. The study made use of the Gynaecological clinic under the Obstetrics and Gynecology Department out of the 16 clinical departments in the institution.
Sampling Procedure and Sample Size
Random sampling technique was employed in the selecting 228 women of reproductive age who participated in the study.
Research Instrument
The study used a structured questionnaire with six sections out of which four sections measured the perception of the respondents on HBM constructs.
Pre-treatment of Questionnaire
The questionnaire was pre-treated by carrying out a pilot study involving administration of 30 copies of questionnaires 30 women of reproductive age. The outcome of this pre-treatment established the suitability of the research design.
Data Collection Procedure
The patients’ consent was sought, before administration of the 228 copies of the questionnaire to the respondents who have given their consent. The copies of the questionnaire were retrieved from the respondents immediately after completion.
Data Management, Analysis and Presentation
The copies of questionnaire retrieved from the respondents were collated, cleaned, coded and entered into Statistical Package for Social Sciences (SPSS) version 17.0 for analysis. Using descriptive and inferential statistics. For the descriptive statistics, frequency count and percentage were used to represent the responses of respondents on each item of the questionnaire, and the categorical variable was analyzed using ANOVA. For the inferential statistics, linear regression analysis was used to test the five hypotheses stated in the study.
Ethical Consideration
The study adhered to the ethics regulating the use of human respondents in scientific research. Ethical approval was obtained from the Ethics and Research Committee of University College Hospital, Ibadan, Oyo State with reference number NHREC/05/01/2008a. Before administering the questionnaire, the aim and procedure of the study were explained to the prospective respondents; they were made to realize that it is a voluntary exercise and respondents could quit at any time. After that, the consent of all the interested respondents was obtained. Also, the researcher adhered to anonymity and confidentiality of data throughout the process of the study.
Results
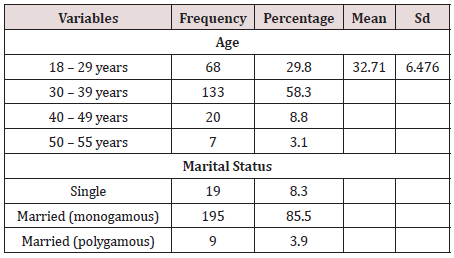
Socio-demographic variables of respondents
A total number of 228 women of reproductive age attending
the gynecological clinic in the University College Hospital, Ibadan
participated in the study. The average age of respondents was
32.7, with a standard deviation of 6.47. The highest percentage
(58.1%) of the respondents was within 30-39 years, and 89.4% of
the respondents were married, and 92.5% were employed. Also,
93.4% had a post-secondary academic qualification, and 4.8% had
secondary school qualification. Others, as shown in (Table 1).
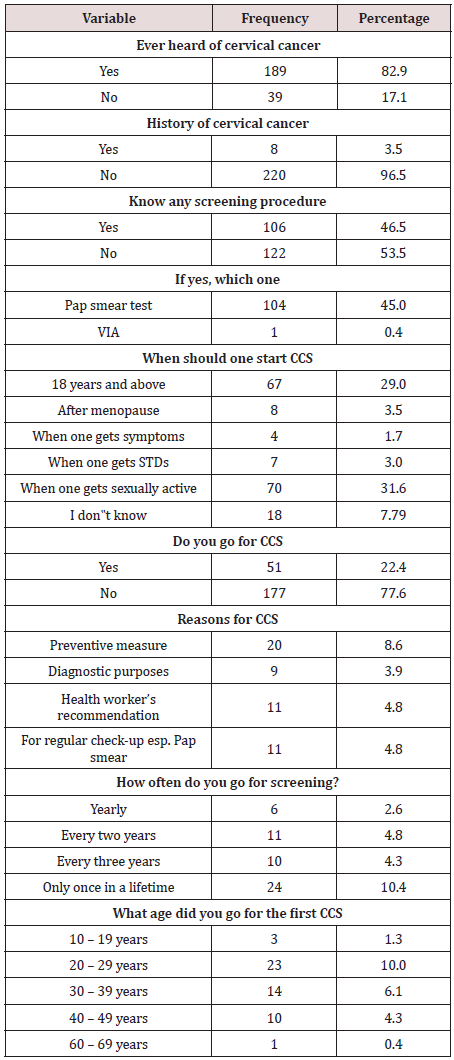
Respondents on knowledge and uptake of CCS
Most of the respondents (82.9%) ever heard of cervical cancer,
96.5% had no history of cervical cancer, 46.5% knew any CCS
procedure with 45.0% reporting Pap smear test. Also, 31.6% of
respondents reported that a person should start CCS when such
a person is sexually active, 29.0% said that one should start CCS
when that individual is 18 years and above.
Also, only 22.4% had ever gone for CCS, 8.6% reported
preventive measure as the reason they went for CCS. However,
10.4% reported that they had gone for CCS only once in their
lifetime with 10.0% reporting they went for CCS when they were
within the age bracket of 20-29 years. (Table 2) highlighted others.
Furthermore, regression analysis shows that the level of knowledge
had no significant influence (R2=0.10, F (1,227) =1.987, P >.05) on
the uptake of CCS.
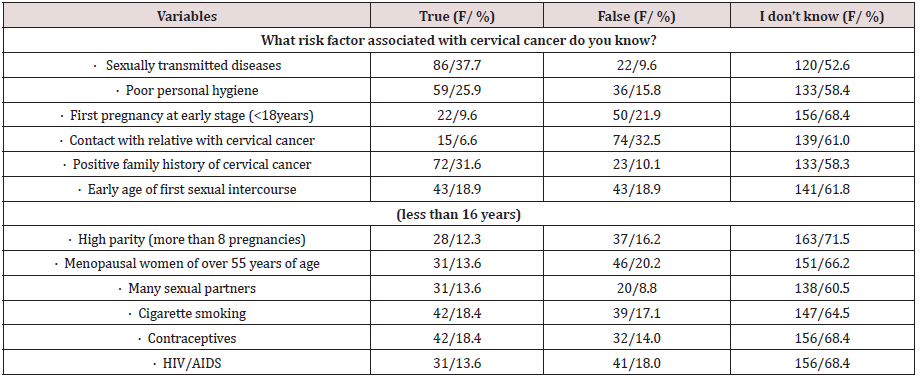
Respondents’ responses to risk factors (perceived susceptibility)
Table 3 shows the risk factors that are associated with cervical cancer, 37.7% of the respondents reported sexually transmitted diseases, poor hygiene (25.9%), positive family history (31.6%), 30.7% had several sexual partners, early age of first sexual intercourse (18.9%), cigarette smoking (18.4%), contraceptives (17.5%) and HIV/AIDS (13.6%). Regression analysis shows that perceived susceptibility had significant influence (R2=0.92, F (1,227) =16.022, P <.001) on the uptake of CCS.
Respondents’ responses to perceived benefits
(Table 4) shows that (62.7%) of the respondents strongly agreed that it is essential to have CCS to now if one is healthy, 46.1% strongly agreed that CCS could find changes in the cervix before becoming cancerous, and 47.8% strongly agreed that changes found from CCS are easily curable. Regression analysis shows that perceived benefits had no significant influence (R2=0.007, F (1,227) =1.396, P >.05) on the uptake of CCS.
Table 4: Showing participants’ responses to perceived benefits.
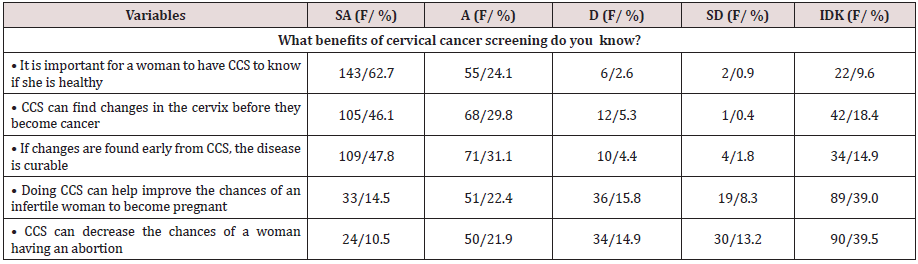
SA-Strongly Agreed, A-Agreed, D-Disagree, SD-Strongly Disagreed, IDK- I do not know; F/% - Frequency and Percentage
Respondents’ responses to perceived barriers
About (32.9%) reported lack of information about CCS procedures, 14.9% reported not knowing where to go for CCS, tests are costly (11.4%), cervix is part of the sex organ and it is private (11.4%), lack of female screeners (10.1%), attitude of health workers (10.1%), and lack of convenient screening time (10.1%). (Table 5) highlighted others. The regression analysis shows that perceived barriers had no significant influence (R2=0.00, F (1,227) =0.34, P >.05) on the uptake of CCS.
Table 5: Showing participants’ responses to perceived barriers.
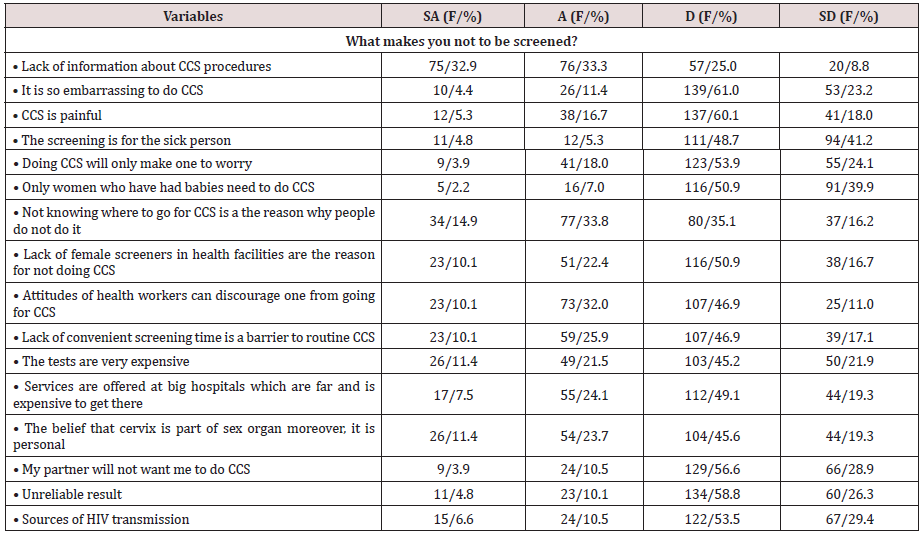
SA-Strongly Agreed, A-Agreed, D-Disagree, SD-Strongly Disagreed; F/% - Frequency and Percentage
Respondents’ responses to cues to action on CCS
Almost half (48.7%) reported take care of my health, (29.8%) after hearing something about CC, (20.2%) because a nurse or mid wife told me, (17.1%) listened to radio or read newspaper, (15.8%) because a doctor told me, and (14.0%) saw it on social media platforms. Table 6 reported others. The regression analysis shows that cues to action had no significant influence (R2=0.007, F (1,227) =1.358, P >.05) on the uptake of CCS.
Table 6: Showing participants’ responses to Cues to Action on CCS.
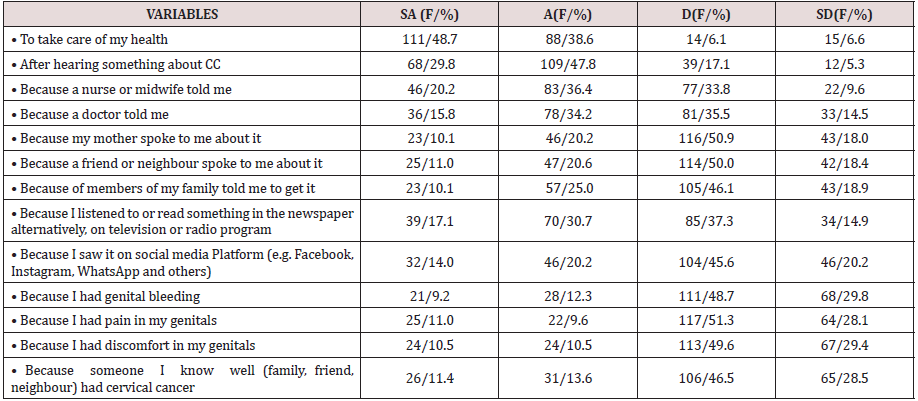
SA-Strongly Agreed, A-Agreed, D-Disagree, SD-Strongly Disagreed; F/% - Frequency and Percentage
Discussion
The participants’ level of knowledge reported in this study is contrary to previous findings. [15] Despite having over nine out of ten participants with post-secondary educational qualification, one would expect a significant level of knowledge about cervical cancer among them. However, the findings of WHO in the year 2012 13 among six sub-Saharan nations also established a low level of awareness of cervical cancer, which led to low uptake of CCS uptake [7]. Also, the studies have substantiated this finding and emphasized that the level of CCS uptake among females in Nigeria is very discouraging [16, 17]. The fact that an individual attained a higher level of education does not necessarily culminate in having excellent knowledge about health issues, let alone taking appropriate preventive steps.
The perceived susceptibility reported by the participants has a significant effect on the uptake of CCS, which shows that the perception that one is at risk of cervical cancer could motivate such individual to undertake CCS. On the other hand, individuals might not undertake CCS if they perceive that they are not susceptible to cervical cancer. As a result, significant perceived susceptibility would positively influence the essence of taking preventive measures towards cervical cancer. The findings of previous studies supported this finding. [8, 18] Among perceived barriers on uptake of CCS reported by the participants of this study is the lack of female screeners, which makes it uncomfortable and painful for women to allow men to examine them. Previous studies established that women prefer female physician to perform CCS [19, 20]. Also, the lack of information plays a significant role in the low uptake of CCS. Since they know next to nothing about the availability of CCS, one would not expect them to go for screening. To corroborate this finding, Ndikom and Ofi [14] also found a lack of information as a perceived barrier among the participants. The studies conducted by other researchers established a lack of information as the main predicting barriers of uptake of CCS among African women [16, 21, 22].
Furthermore, perceived benefits reported by the participants had no significant effect on the uptake of CCS. Their perceived benefits did not culminate to practice, which shows that the participants have low perceived benefits of CCS. In other words, they place insignificant value on what they stand to gain from CCS. Other study also reported similar findings among Saudi Arabian women. [20]
The final finding shows that cues to action reported by the participants did not result in uptake of CCS. Though some participants strongly agreed that taking care of their health is a cue to action; 47.8% (n=109) agreed that hearing something about cervical cancer is a cue to action, and 17.1% (n=39) reported getting information from the media while 14.0% (n=32) reported social media as their source. Still, the cues to action reported did not translate into practice. This finding is contrary to the previous work, [23] where significant others and healthcare professionals influenced the uptake of CCS among the respondents.
Conclusion
Findings from the present study revealed a low level of knowledge about cervical cancer and the level of knowledge had no significant influence on the uptake of CCS. However, the participants’ perceived susceptibility significantly modified CCS uptake. Furthermore, perceived barriers had no significant effect on the uptake of CCS. Similarly, perceived benefits had no significant effect on the uptake of CCS.
Recommendation
The study recommends community-integrated cervical cancer screening program, which will be available, accessible and affordable for all women regardless of their socio-economic status. Such should be planned with the intention of creating more awareness and increase the present level of knowledge about cervical cancer and its consequences so that women would better comprehend how susceptible they are to the disease and as such take appropriate steps.
References
- Baileff A (2000) Cervical Screening: Patients “Negative Attitudes and Experiences. Nursing Standard 14(44): 35-37.
- WHO Cervical Cancer, World Health Organization, Geneva 2015a
- World Health Organization http://www.who.int/mediacentre/factsheets/fs380/en/ 2015b
- Aiyede LR, Onakewhor JUE, Aziken ME, Ande ABA, Aligbe JU, et al. (2010) Carcinoma of the Uterine Cervix in Nigerian Women: The Need to Adopt a National Prevention Strategy. Sahel Medical Journal 11(1): 1-11.
- Okunnu J (2010) No woman needs to die from cervical cancer cynics, and jenny limited 1st floor, Oakland centre, 48 AguiyeIronsi Street Maitama District Abuja.w ww.bwsinit.org. www.bwsinit.org. 2010
- Oguntayo O, Zayyan M, Kolawole A, Adewuyi S, Ismail H, et al. (2011) Cancer of the cervix in Zaria, Northern Nigeria. E cancer medical science 5: 219.
- Ferlay J, Soerijomataram I, Ervik M, Sultan Eser, Colin Mathers, et al. (2015) Cancer Incidence and Mortality Worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136(5): 359-386.
- Saslow D, Solomon D, Lawson HW, Maureen Killackey, Shalini Kulasingam, et al. (2013) American Cancer Society' American Society for Colposcopy and Cervical Pathology; and American Society for Clinical Pathology Screening Guidelines for the Prevention and early detection of Cervical cancer. Am J Clin Pathol 62(3): 147-172.
- WHO (2006) Comprehensive cervical cancer control: A guide to essential practice. Geneva, Switzerland pp. 272.
- Bastos J, Peleteiro B, Gouveia J, Coleman MP, Lunet N, et al. (2010) The state of the art of cancer control in 30 European countries in 2008. Int J Cancer 126(11): 2700-2715.
- WHO (2014) Nigeria: Human Papillomavirus and Related Cancers, Fact Sheet 2014. WHO/ICO HPV Information Centre, World health organization
- Arulogun OS, Maxwell OO (2012) Perception and utilization of cervical cancer screening services among female nurses in University College Hospital, Ibadan, Nigeria. Pan Afr Med J 11: 69.
- World Health Organisation (WHO) Prevention of Cervical Cancer through Screening Using Visual Inspection with Acetic Acid (VIA) and Treatment with Cryotherapy: A Demonstration Project in six African Countries: (Malawi, Madagascar, Nigeria, Uganda, the United Republic of Tanzania, and Zambia). Geneva: WHO Document Production Services. 2012.
- Ndikom CM, Ofi BA (2012) Awareness, perception and factors affecting utilization of cervical cancer screening services among women in Ibadan, Nigeria. Reproductive Health 9-11.
- Wright KO, Faseru B, Kuyinu Y, Faduyile F (2014) Awareness and uptake of the Pap smear among market women in Lagos, Nigeria. Journal of Public Health in Africa 2(1): e14.
- Nwankwo KC, Aniebue UU, Aguwa EN, Anarado AN, Agunwah E, et al. (2011) Knowledge Attitudes and Practices of Cervical Cancer Screening among Urban and Rural Nigerian Women: a Call for Education and Mass Screening. European Journal of Cancer Care 20(3): 362-367.
- Awodele O, Adeyomoye AA, Awodele DF, Kwashi V, Awodele IO, et al. (2011) A study on cervical cancer screening amongst nurses in Lagos University Teaching Hospital, Lagos, Nigeria. J Cancer Educ 26(3): 497-504.
- Rajkumar R (2012) Topics on Cervical Cancer with an Advocacy for Prevention. Rijeka, Croatia: Intech 1-286.
- Ma GX, Gao W, Fang CY, Tan Y, Feng Z, et al. (2013) Health beliefs associated with cervical cancer screening among Vietnamese Americans. J Women's Health 22(3): 276-288.
- Yakout SM, Moawed S, Gemeay EM (2016) Cervical Cancer and screening test (Pap test): knowledge and beliefs of Egyptian women. Am J Nurs Sci 5(5): 175-184.
- Gichangi P, Estamble B, Bwayo J (2003) Knowledge and practice about cervical cancer and pap smear testing among patients at Kenyatta National Hospital. International Journal of Gynaecological Cancer 13(6): 827-833.
- Fort VK, Makin MS, Siegler AJ, Ault K, Rochat R, et al. (2011) Barriers to cervical cancer screening in Mulanje, Malawi: a qualitative study. Patient preference and adherence 5: 125-131.
- Ackerson K (2010) Personal influences that affect motivation in Pap smear testing among African American women. Journal of Obstetric, Gynecologic and Neonatal Nursing 39(2): 136-146.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...