
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Research Article(ISSN: 2637-4544) 
Dehydration, is it an issue in threatened preterm labor? Volume 3 - Issue 3
Mohamed El Sayed Rafeek*
- Department of Obstetrics and Gynecology, Zagazig University, Egypt
Received:June 10, 2019; Published: June 17, 2019
Corresponding author: Mohamed El Sayed Rafeek, Department of Obstetrics and Gynecology, Zagazig University, Egypt
DOI: 10.32474/IGWHC.2019.03.000161
Abstract
Background: Understanding the complex physiological and pathological mechanisms that increases the risk for developing preterm labor could aid in reducing the clinical scenarios that are presented in everyday practice that cause preterm labor.
Aim: To investigate whether cases presenting at 23 0/7 to 36 6/7 gestational weeks having painful, regular contractions are more expected to be dehydrated than cases at the same gestational ages.
Methodology: A prospective clinical research trial conducted on 250 cases performed from January 2016 till February 2019. Urine analysis was performed for all research study subjects at the time of entry to Ward before administration of an intravenous line or any other mode of therapy. Urine specific gravity was assayed from a dipstick of a urine specimen, comparative analysis of urine specific gravity have been conducted between both research groups.
Results: No statistically significant difference between both research groups (no threatened preterm labor research group and threatened preterm labor research group as regards urine specific gravity among compared gestational age groups and (p values =0.543, 0.405, 0.263, 0.136 consecutively).
Conclusion: Intravenous hydration according to the current study findings doesn’t appear to be an effective mode of therapy in preterm labor that was observed due to the insignificant differences in both research groups as regards the urine specific gravity readings.
Keywords: Dehydration; Threatened preterm labor; Intravenous hydration
Introduction
Preterm labor is classically defined as presence of regular, painful uterine contractions before 37 complete gestational weeks. Preterm labor a growing issue all over the globe due to raised ART pregnancies that increases the clinical risks of maternal and fetal morbidities and mortalities [1]. Understanding the complex physiological and pathological mechanisms that increases the risk for developing preterm labor could aid in reducing the clinical scenarios that are presented in everyday practice that cause preterm labor [2]. Tocolytic agents although considered one of the cornerstone agents implemented in management of those cases it is not the only preventive or therapeutic mode. Hydration at proper levels was revealed and displayed at molecular and hormonal levels to reduce secretion of both ADH hormone and oxytocin thus reducing the uterine contractility [3].
One of the first lines of management in cases of threatened preterm labor that reduces the uterine intensity and frequency of contractions is intravenous hydration. Another group of researchers have revealed and displayed among their research study findings that dehydration releases ADH hormone that triggers uterine contractility due to molecular similarity to oxytocin hormone. An area of great research debate is whether hydration arrests the preterm labor contractions [4]. The hypothesis that intravenous hydration therapy is an efficient mode for inhibiting uterine contractility relies on the principle that ADH and oxytocin hormones release is suppressed by hydration and therefore hinders the uterine contract6ions besides the hypothesis that cases having uterine contractions are considered more severely dehydrated than cases without contractions. On the other hand, all these assumptions are not backed up by clinical evidence-based research [5,6]. ADH to be precise is complex in its assay for evaluation of the hydration status since it is released in in a pulsatile manner and have a short half-life. The usage of urine specific gravity as an alternative to the hydration status is considered more practical and applicable on clinical basis [7,8].
Aim
To investigate whether cases presenting at 23 0/7 to 36 6/7 gestational weeks having painful, regular contractions are more expected to be dehydrated than cases at the same gestational ages.
Methodology
A prospective clinical research trial conducted on 250 cases performed from January 2016 till February 2019, inclusive research criteria were singleton gestations that were presented with preterm contractions, no medical comorbidities e.g. DM, hypertension, cases having medical scenarios that could affect urine specific gravity e.g. preeclampsia vaginal bleeding, ruptured membranes, and bacteriuria besides cases having advanced cervical dilation (above 3cm), multifetal gestations, fetal congenital anomalies, and IUFD. research cohort was categorized into two research categorial groups 145 women having no threatened preterm labor manifestations as controls, 105 women having threatened preterm labor as cases research group.
Urinalysis was performed for all research study subjects at the time of entry to Ward before administration of an intravenous line or any other mode of therapy urine specific gravity was assayed from a dipstick of a urine specimen, comparative analysis of urine specific gravity have been conducted between both research groups.
Clinical definition of dehydration as a urine specific gravity >=1.020, was used as a threshold value, threatened preterm labor was defined as the main complaint of contractions in absence of cervical changes.
Statistical Analysis
Data were collected, revised, coded and entered to the statistical package for social science (SPSS) version 23 (IBM SPSS Ver. 23). The qualitative data were presented as numbers and percentages and compared between groups using Chi-square test while the quantitative data with parametric distribution were presented as mean, standard deviations and ranges and compared between groups using Independent t-test. The diagnostic accuracy of urine specific gravity test was assessed by using Receiver Operating Characteristic curve (ROC) in the qualitative form. The confidence interval was set to 95% and the margin of error accepted was set to 5%. So, the p-value was considered significant at the level of < 0.05.
Results
(Table 1) reveals and displays that as regards demographic research data there was no statistical significant difference between both research groups (no threatened preterm labor research group and threatened preterm labor research group ), as regards age (years),gestational age at presentation, gestational age categories compared (23 to 27 weeks, 28 to 38 weeks, 32 to 37 weeks), BMI (kg/m2), Smoking, Preterm birth (p values =0.072, 0.442, 0.658, 0.498, 0.813, 0.872 consecutively).
Table 1: Demographic data of the two studied groups.
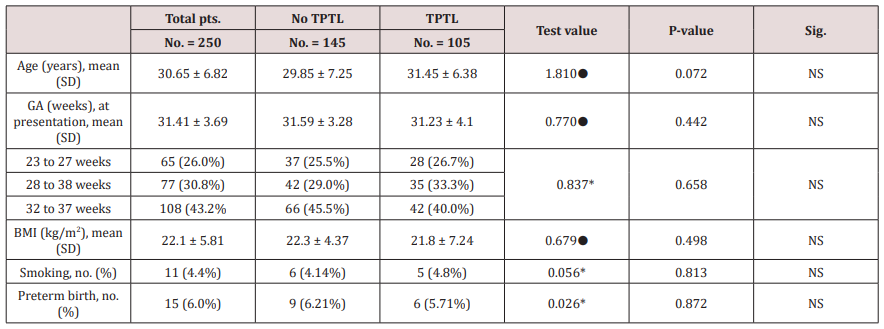
GA: Gestational age; BMI: Body Mass Index; ●: Independent t-test; *: Chi-square test
(Table 2) reveals and displays that Receiver operating characteristic curves for urine specific gravity as a predictor for threatened preterm labor by gestational age groups In which urine specific gravity at 23–27 gestational weeks had a true positive =15, false positive =17, true negative =20, false negative= 13 sensitivity =53.60%, specificity =54.05%, PPV=46.88% NPV= 60.61%, accuracy =58.33%, whereas at 28–31 gestational weeks had a true positive =20, false positive =20, true negative =22, false negative =15 sensitivity =57.10%, specificity =52.38%, PPV=50.00% NPV=59.46%, accuracy =54.55%, whilst at 32–37 gestational weeks had a true positive =25, false positive =32, true negative =34,false negative =17, sensitivity =59.50%,specificity =51.52%, PPV=43.86%, NPV=66.67%,accuracy =54.63%, finally total number of cases had a true positive =60, false positive =69, true negative =76, false negative =45, sensitivity =57.14%, specificity =52.41%, PPV=46.51%, NPV=62.80%, accuracy =54.40%, there was no statistically significant difference both research groups (no threatened preterm labor research group and threatened preterm labor research groups as regards urine specific gravity among compared gestational age groups and as a whole (p values =0.543, 0.405, 0.263, 0.136 consecutively).
Table 2: Receiver operating characteristic (ROC) curves for urine specific gravity as a predictor for threatened preterm labor by gestational age groups.
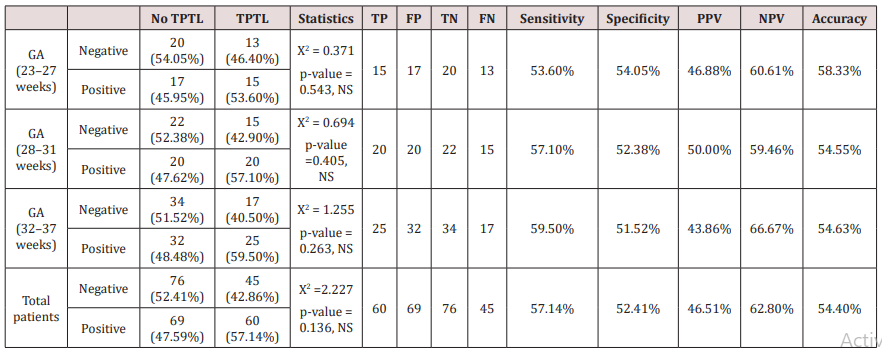
GA: Gestational age; X2 : Chi-square test; TP: True positive; FP: False positive; TN: True negative; FN: False negative; PPV: Positive predictive value; NPV: Negative predictive value
Discussion
Around 30% to 50% of preterm deliveries are statistically correlated to spontaneous forms of preterm labor. preterm labor remains a challenging clinical scenario due to multifactorial possible etiologies underlying its clinical presentation e.g. infections, overdistended uterus and among other issues arising such as the patterns of secretion of ADH hormone that could be triggered by the hydration status [9,10].
A prior research team of investigators have conducted a similar research study to the current study in approach and methodology revealing and displaying among their research findings that hydration levels in cases of threatened preterm labor are not different from cases that have the same range of gestational ages not having premature contractions. Those research findings are in harmony and great similarity to the current study findings denoting that hydration therapy could not be useful as expected in those categories of cases [11-13].
Interestingly it was mentioned by various investigators that there are hazardous complications that could arise from trying to use dehydration as an explanation for premature labor and subsequently implementing intravenous hydration as a mode of therapy besides Fluid overload consequently could cause pulmonary edema, heart failure, particularly with some tocolytic agents such as beta 2 agonists pulmonary edema have been observed in the usage of intravenous hydration therapy mode implemented in the USA practice [1,7,9].
Additionally, it was noticed and observed by various prior research groups of investigators that practioners usually administer intravenous hydration as a primary therapy more willingly than investigating the true etiology causing the pathophysiological development of preterm labor [2,5,10].
Another prior research study to investigate if cases suffering from threatened preterm labor have dehydration issues. The research team of investigators have implemented a case control clinical research trial in which they recruited initially 840 cases from which 391 cases were excluded. 188 cases had threatened preterm labor 261 were controls. Cases having threatened preterm labor haven’t been more dehydrated than cases of the same gestational age range clinically presenting with other complaints (p value =0.12). Those research findings are in addition support the current research study findings [3,6,13].
Cases having preterm labor caused by placental abruption, infection, could be managed in adequately due to intravenous hydration due to delay in etiological diagnosis of premature uterine contractions cause Another prior research study priorly conducted have revealed no correlation between threatened preterm labor and hydration level. Even though there is a hypothesis that ADH and oxytocin have similar molecular features, researchers in the current and prior research studies didn’t observe a correlation between hydration level and premature contractions [4,8,10].
Conclusion and Recommendation
Intravenous hydration according to the current study findings doesn’t appear to be an effective mode of therapy in preterm labor that was observed due to the insignificant differences in both research groups as regards the urine specific gravity readings. Future research studies however are recommended to be performed on larger number of cases putting in consideration the variabilities regarding racial and ethnic differences that could affect the findings in those categories of cases. Additionally, assay of ADH and oxytocin hormone levels is strongly recommended in future research studies to elucidate the hydration status impact on preterm labor.
References
- American College of Obstetricians and Gynecologists (2016) ACOG practice bulletin no. 159: Management of preterm labor. Obstetrics & Gynecology 127: e29-e38.
- Baron S, Courbebaisse M, Lepicard EM, Friedlander G (2014) Assessment of hydration status in a large population. British Journal of Nutrition 113(1): 147-158.
- Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake P (2018) Births: Final data for 2016. National Vital Statistics Reports 67(1): 1-55.
- Sommerfield LM, McAnulty SR, McBride JM, Zwetsloot JJ, Austin MD, et al. (2016) Validity of urine specific gravity when compared with plasma osmolality as a measure of hydration status in male and female NCAA collegiate athletes. Journal of Strength and Conditioning Research 30(8): 2219-2225.
- Stan C, Boulvain M, Pfister R, Hirsbrunner-Almagbaly P (2013) Hydration for treatment of preterm labour. Cochrane Database of Systematic Reviews.
- Naik Gaunekar N, Raman P, Bain E, Crowther CA (2013) Maintenance therapy with calcium channel blockers for preventing preterm birth after threatened preterm labour. Cochrane Database of Systematic Reviews 10: CD004071.
- Phillips SM, Sykes D, Gibson N (2014) Hydration status and fluid balance of elite European youth soccer players during consecutive training sessions. Journal of Sports Science & Medicine 13(4): 817-822.
- Zubac D, Antelj T, Olujic D, Ivancev V, Morrison SA (2017) Fluid balance and hydration assessment during the weights table preparation phase in elite youth boxers. Journal of Sports Sciences 35(8): 719-726.
- Walsh JM, Doyle LW, Anderson PJ, Lee KJ, Cheong JL (2014) Moderate and late preterm birth: effect on brain size and maturation at term-equivalent age. Radiology 273(1): 232-240.
- Gyamfi-Bannerman C, Ananth CV (2014) Trends in spontaneous and indicated preterm delivery among singleton gestations in the United States, 2005-2012. Obstetrics & Gynecology 124(6): 1069-1074.
- Martin JA, Hamilton BE, Ventura SJ, Osterman MJ, Wilson EC, et al. (2012) Births: final data for 2010. Natl Vital Stat Rep 61(1): 1-72.
- Pike KC, Lucas JS (2015) Respiratory consequences of late preterm birth. Pediatric Respir Rev 16(3): 182-8.
- Ramachandrappa A, Jain L (2015) The late preterm infant. In: Martin R, Fanaroff A, Walsh M [Edt.], Fanaroff and Martin’s neonatal-perinatal medicine. Philadelphia: Elsevier Saunders: p. 577-591.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...





