Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Research Article(ISSN: 2637-4544) 
Clinical Safety Issues of Inpatient Versus Outpatient Management Lines in Preterm Premature Rupture of Membranes Volume 3 - Issue 5
Waleed Tawfik1* and Marwa Elsayed Ahmed2
- 1Obstetrics and Gynecology Department, Faculty of Medicine, Benha University, Egypt
- 2Pediatrics Department, Faculty of Medicine, Benha University, Egypt
Received:September 03, 2019; Published: September 18, 2019
Corresponding author: Waleed Tawfik, Lecturer of Obstetrics and Gynecology, Obstetrics and Gynecology Department, Faculty of Medicine, Benha University, Benha, Egypt
DOI: 10.32474/IGWHC.2019.03.000171
Abstract
Background: Preterm premature rupture of membranes is a frequent every day obstetric clinical scenario the proper line of management is considered lifesaving in some situations. The main aim of most investigators and practitioners all over the globe is to explore the safest management line according to the pros and cons of each decision.
Aim: To compare the neonatal clinical outcomes of cases women having PPROM before 34 gestational weeks, in accordance to the management protocol (inpatient versus outpatient care).
Methodology: A prospective clinical research trial that recruited 300 research study subjects Inclusive research criteria were admitted with a clinical diagnosis of PPROM between 24+0 and 33+6 gestational weeks and didn’t deliver within the 48 hours after PPROM. Exclusive research criteria have been twin gestations, fetal anomalies.
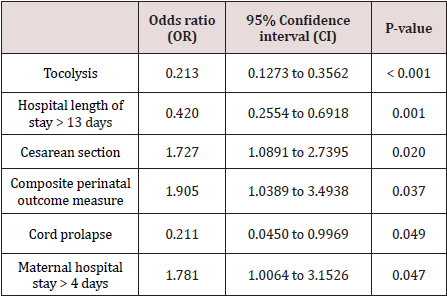
Results: The statistical Logistic regression analysis for factors associated to outpatient delivery showing that there was statistical significance concerning Tocolysis, Hospital length of stay > 13 days, Cesarean section, Composite perinatal outcome measure, Cord prolapse, Maternal hospital stay > 4 days (p values < 0.001, 0.020, 0.037, 0.049, 0.047 consecutively).
Conclusion: Outpatient care of PPROM clinical scenarios is considered a safe effective alternative traditional inpatient management line, however future research efforts are required to be conducted in a multicentric fashion with larger sample sizes to aid in future implementation of the best clinical management guidelines.
Keywords: Inpatient; Outpatient; PROM
Introduction
Preterm premature rupture of membranes is a frequent every day obstetric clinical scenario the proper line of management is considered lifesaving in some situations [1]. Morbid maternal and fetal complications are almost always expected in those clinical cases categories since the preterm premature rupture of membranes represents the anatomical and physiological breach of a natural barrier against arising bacterial infection that could cause prematurity and chorioamnionitis issue arousal particularly when diagnosis and management is delayed [2].
However, the best management line whether in patient or outpatient is an issue of research debate particularly when considering the patient compliance and resource limits especially in developing countries. Home deliveries and cord prolapse have been reported in cases that were managed conservatively in an outpatient setting although a considerable reduction in costs and increased patients preference of this line of management have led to the interest to investigate its effectiveness in comparison to inpatient management lines [3,4].
In patient management lines although more costly but are considered the safeguard against sudden developing unfavorable complications that could develop from preterm premature rupture of membranes. The main aim of most investigators and practitioners all over the globe is to explore the safest management line according to the pros and cons of each decision [5,6]. Antibiotics remain the cornerstone management agent implemented in all cases on the other hand the patient compliance in outpatient management and early detection of complications with proper transfer to hospital remains an issue of concern [7,8].
Aim of the Work
To compare the neonatal clinical outcomes of cases women having PPROM before 34 gestational weeks, in accordance to the management protocol (inpatient versus outpatient care).
Methodology
This study was done at Benha University hospital in the Obstetrics & Gynecology and Radiology departments.
A prospective clinical research trial that recruited 300 research study subjects Inclusive research criteria were admitted with a clinical diagnosis of PPROM between 24+0 and 33+6 gestational weeks and didn’t deliver within the 48 hours after PPROM. Exclusive research criteria have been twin gestations, fetal anomalies. Gestational age has been obtained from all recruited study subjects using the routine sonographic examination Conducted within the first gestational trimester. 150 cases were chosen to be managed on an outpatient basis, the following criteria were used to choose that management line involving absent signs of infections (maternal fever above or equal to 38 °C), uterine tenderness, fetal tachycardia (above 160 beats/min) and foul odor of amniotic fluid), presence of labor signs (regular uterine contractions, cervical dilatation over 3 cm), and case acceptability for management line. cases within that research group category have been discharged from the second day of admission and performing daily fetal cardiotocography, a laboratory blood sample twice a week and a weekly clinical and sonographic examination. the other research categorial group involved 150 research study subjects recruited for inpatient management line with the same criteria of management however cases were not discharged till occurrence of delivery. All cases have been administered betamethasone (two intramuscular doses of 12 mg 24 hours apart) for fetal lung maturation and antibiotic prophylaxis regimen (ampicillin or cefixime). The following research variables have been collected a composite measure of neonatal clinical outcome, involving perinatal death, early neonatal infection with sepsis, intraventricular hemorrhage, and necrotizing enterocolitis birth weight, gestational age at birth, and Apgar scoring levels. Other obstetric clinical outcomes obtained and recorded have been as follows, gestational age at time of delivery, latent period, chorioamnionitis, placental abruption, cord prolapse, and mode of delivery.
Statistical Analysis
Data were collected, revised, coded and entered to the Statistical Package for Social Science (IBM SPSS) version 23. The distribution of quantitative data was tested by Kolmogorov- Smirnov test of normality. So, the quantitative data were presented as mean, standard deviations and ranges according to parametric distribution. Also, qualitative variables were presented as number and percentages. The comparison between groups regarding qualitative data was done by using Chi-square test and/or Fisher exact test when the expected count in any cell found less than 5. The comparison between two independent groups with quantitative data and parametric distribution was done by using Independent t-test. Also, logistic regression analysis was used to assess the factors associated to outpatient delivery. The confidence interval was set to 95% and the margin of error accepted was set to 5%. So, the p-value was considered significant at the level of < 0.05.
Results
Table 1 reveals and displays the demographic characteristics of the investigated cases in which there was no statistical significance as regards maternal age, BMI, Smoking, History of miscarriage, spontaneous preterm delivery , history of PROM < 37 weeks, previous cesarean section, cervical cerclage, Low lying placenta and placenta previa, Gestational diabetes (p values= 0.149, 0.078, 0.727, 0.821, 0.368, 0.296, 0.743, 0.821, 0.759, 0.411 consecutively) whereas nulliparous cases were statically significantly higher among outpatient research group in comparison to inpatient research group (p value =0.010).
Table 1: Demographic and characteristics of the studied patients.
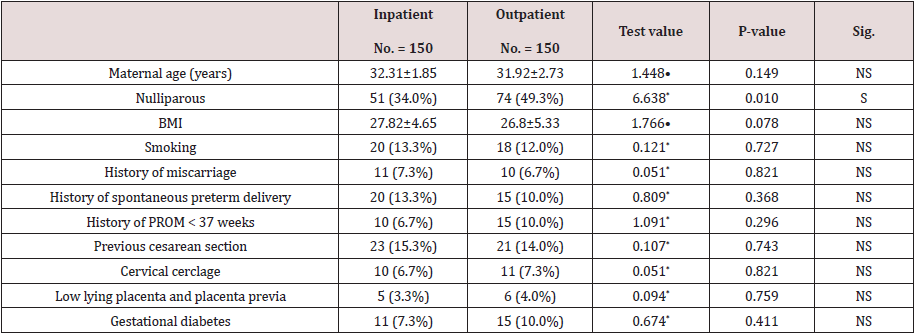
•: Independent t-test; *: Chi-square test.
Table 2 reveals and displays the Comparative statistical of management, delivery, obstetric and neonatal clinical outcomes between the two investigated research groups (outpatient versus inpatient) in which there was no statistical significant difference between both research groups as regards Gestational age at PPROM, elevated CRP at PPROM (>15mg/L), leukocytosis (>15G/L), cervical length <25mm, Cephalic presentation, latency duration (days), latency <7 days, Duration of antibiotic therapy (p values = 0.241, 0.766, 0.686, 0.729, 0.317, 0.147, 0.633, 0.070 consecutively) whereas tocolysis, Mean hospital length of stay (days), hospital length of stay > 13 days were statistically significantly higher among inpatient research group in comparison to outpatient research group (p values <0.001, <0.001, 0.001 consecutively) concerning delivery aspects there was no statistical significant difference as regards Gestational age at delivery, Labor induction, n (%), Vaginal delivery n (%), Cesarean before labor n (%),Cesarean during labor, n (%)Birth weight (kg), Apgar score at 5 minutes <7 (p values =0.393,0.447,0.380,0.208 consecutively) whereas mode of delivery showed statistical significant difference between both research groups (p value=0.023). Furthermore the obstetric neonatal outcomes there was no statistical significant difference as regards the neonatal sepsis (p value=0.777), whereas composite perinatal outcome measure was statically significantly higher among outpatient research group (p value=0.035). As regards the perinatal outcomes there was no statistical significant difference as regards the presence of Chorioamnionitis, Intrauterine death, Placental abruption (p values=0.557, 0.652, 0.734 consecutively) whereas cord prolapse was statically significantly higher among inpatient research group (P value=0.031), concerning the postnatal clinical outcomes there was no statistical significant difference as regards the endometritis ,maternal sepsis (p values =0.354, 0.561 consecutively) whereas Maternal hospital stay > 4 days was statically significantly higher among outpatient research group(p value =0.017).
Table 2: Comparison of management, delivery, obstetric and neonatal outcomes between the two studied groups
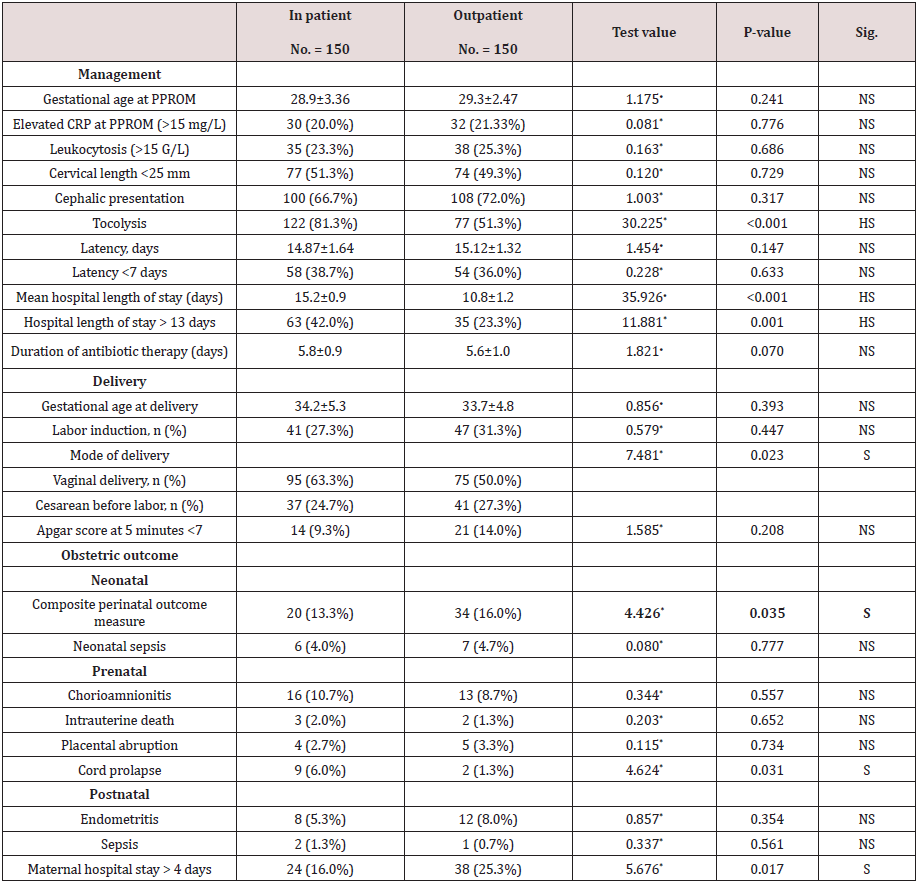
•: Independent t-test; *: Chi-square test.
Table 3 reveals and displays the statistical Logistic regression analysis for factors associated to outpatient delivery showing that there was statistical significance concerning Tocolysis, Hospital length of stay > 13 days, Cesarean section, Composite perinatal outcome measure, Cord prolapse, Maternal hospital stay > 4 days (p values < 0.001, 0.001, 0.020, 0.037, 0.049, 0.047 consecutively)
Discussion
Preterm premature rupture of membranes is considered a real challenging obstetric clinical scenario since improper or defective management line would result in highly serious morbid complications at maternal and fetal levels [9,10]. An issue of research debate is to consider the safety profile of outpatient management that would reduce the cost and burden of prolonged hospitalization, however the issues of cases compliance to outpatient management criteria remains a real challenging issue [11]. In patient management lines are preferred by various obstetric management teams due to proposed higher safety profile although caries higher burden as regards costs [1,3,5] A prior research study similar to the current study in approach and methodology have shown that outpatient management of preterm premature rupture of membranes between 24+0 and 33+6 gestational weeks is not correlated to more elevated neonatal morbidity or mortality issues in comparison and contrast to inpatient management protocols those research results are in harmony to the current study results in a great manner that could be justified by the fact that proper cases selection as regards the management line is one of the safe guards that prevent the emergence of maternal; or neonatal complications, besides the proper implementation of maternal and fetal monitoring in a satisfactory safe manner even when cases are managed on an outpatient basis [2,4,7].
In an interesting manner another research group of investigators have observed that acute forms complications e.g. placental abruption, cord prolapse are not observed to be more raised in frequency using an outpatient management line in presence of proper patient compliance [8,11]. Prior retrospective research studies have revealed and displayed that that maternal clinical outcomes (e.g. chorioamnionitis) and neonatal clinical outcomes (NICU admission) are greatly similar among cases that are managed by inpatient and outpatient basis [6,10]. Prior research groups of investigators and numerous clinicians have considered that the main issue is the clinical expected risk for developing acute complications such as placental abruptive events and cord prolapse that would necessitate the inpatient management lien as a matter of safety. It was concluded by various research efforts and findings that tocolysis more than 48 hours wouldn’t prolong the period of latency or reduce neonatal complications in comparison to no tocolysis [7,9].
Conclusion and Recommendations for Future Research
Outpatient care of PPROM clinical scenarios is considered a safe effective alternative traditional inpatient management line, however future research efforts are required to be conducted in a multicentric fashion with larger sample sizes to aid in future implementation of the best clinical management guidelines taking in consideration racial, ethnic and BMI differences that could affect the management line choice and effectiveness.
References
- Shree R, Caughey AB, Chandrasekaran S (2015) Short interpregnancy interval increases the risk of preterm premature rupture of membranes and early delivery. J Matern Fetal Neonatal Med 31(22): 3014-3020.
- Roberts CL, Wagland P, Torvaldsen S, Bowen JR, Bentley JP, et al. (2017) Childhood outcomes following preterm prelabor rupture of the membranes (PPROM): A population-based record linkage cohort study. J Perinatol 37(11): 1230-1235.
- Schaaf J, Mol B, Abu Hanna A, Ravelli A (2011) Trends in preterm birth: Singleton and multiple pregnancies in the Netherlands, 2000-2007. BJOG 118(10): 1196-1204.
- Tsafrir Z, Margolis G, Cohen Y, Cohen A, Laskov I, et al. (2015) Conservative management of preterm premature rupture of membranes beyond 32 weeks’ gestation: Is it worthwhile? J Obstet Gynaecol 35(6): 585-590.
- Goya M, Bernabeu A, García N, Plata J, Gonzalez F, et al. (2013) Premature rupture of membranes before 34 weeks managed expectantly: maternal and perinatal outcomes in singletons. J Matern neonatal Med 26(3): 290-293.
- Huret E, Chanavaz Lacheray I, Grzegorczyk Martin V, Fournet P (2014) Home care of premature rupture of membranes prior to 37 weeks’ gestation. Gynécologie Obs Fertil 42(4): 222-228.
- Garrido MM, Kelley AS, Paris J, Roza K, Meier DE, et al. (2014) Methods for Constructing and Assessing Propensity Scores. Health Serv Res 49(5): 1701-1720.
- Garabedian C, Bocquet C, Duhamel A, Rousselle B, Balagny S, et al. (2015) Preterm rupture of membranes: Is home care a safe management? J Gynecol Obstet Biol la Reprod 45(3): 278-284.
- Beckmann M, Gardener G (2013) Hospital versus outpatient care for preterm pre-labour rupture of membranes. Aust NZJ Obstet Gynaecol 53(2): 119-124.
- Palmer L, Grabowska K, Burrows J, Rowe H, Billing E, et al. (2017) A retrospective cohort study of hospital versus home care for pregnant women with preterm prelabor rupture of membranes. Int J Gynaecol Obstet 137(2): 180-184.
- Lorthe E, Goffinet F, Marret S, Vayssiere C, Flamant, et al. (2017) Tocolysis after preterm premature rupture of membranes and neonatal outcome: A propensity-score analysis. Am J Obstet Gynecol 217(2): 212.e1-212.e12.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...