Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Research Article(ISSN: 2637-4544) 
Clinical Assessment of Short-Term Outcome of Para Aortic Lymphadenectomy in Cases of Cancer Ovary Volume 4 - Issue 1
Bassem A Islam*
- Department of Obstetrics and Gynecology, Ain Shams University, Egypt
Received: December 17, 2019; Published: January 10, 2020
Corresponding author: Dr Bassem A Islam Lecturer in Department of Obstetrics and Gynecology, Faculty of Medicine, Ain Shams University, Cairo, Egypt
DOI: 10.32474/IGWHC.2020.04.000178
Abstract
There is no uncertainty that total careful organizing is the standard of care for ovarian malignant growth. Lymphadenectomy is a fundamental piece of careful arranging as they have a potential job in both organizing and retroperitoneal debulking. Proof from the writing shows that medical procedure is lacking in 75% of situations when the method is performed by unpracticed specialists. This information reports a 50_100% contrast in 5-year generally endurance. Then again, the wellbeing of the medical procedure is much increasingly significant than its sufficiency in many cases. The careful intercession ought not open the patient to expanded paces of intraoperative difficulties while the specialist is endeavoring endeavors to play out an increasingly broad LND. Since the lymph hubs are found adjoining significant structures including extraordinary vessels and nerves, a few wounds might be seen during LND. the normal execution of lymphadenectomy in ovarian malignant growth patients is yet the subject of debate. In this way, the point of current investigation is to assess the recurrence and nature of employable and perioperative intricacies and to improve careful result identified with para-aortic lymphadenectomy in ovarian malignant growth patients. Patients were selected among those going to the oncology outpatient facility of branch of Obstetrics and Gynecology Ain Shams University The examination included 72 patients; analyzed by clinical assessments, ultrasound of midriff and pelvis and CT of mid-region and pelvis associated these outcomes with tumor marker CA125 level. Patients were admitted to medical clinic and a composed educated assent was marked by every patient with clarification of the administration technique, potential risks and development. Full history taking and Complete research center. Radiological assessment included ultrasound of stomach area and pelvis, CT of midriff and pelvis.
Patients and Methods: All patients (n=36) experienced medical procedure including para aortic LND, 8 patients experienced ripeness safeguarding medical procedure, 12 patients experienced formal arranging medical procedure for suspected beginning time ovarian malignant growth, 10 patients experienced essential debulking surgery and 56 patients experienced interim debulking medical procedure. The perioperative parameters of medical procedure were assessed as far as; employable time, the blood misfortune rate, perioperative blood transfusions, emergency unit and postoperative medical clinic stay, as well as assessment of perioperative morbidities and mortalities. Dismalness information was assessed by; entrail/bladder damage, ureteric damage, vascular damage, discharge, profound venous thrombosis (DVT), aspiratory embolism and wound disease.
Results: The result of para aortic LND was evaluated as far as; number of hubs retrieved, time for analyzation, related blood misfortune and careful intricacy exceptional to PALND. Present examination gives data to help in the structure of future studies and conventions for overseeing ovarian malignancy patients. Despite the fact that our information on perioperative horribleness of medical procedure included PALND for ovarian disease is promising; still exists a requirement for planned comparative preliminaries surveying endurance and personal satisfaction of ovarian disease patients treated with this class of medical procedure.
Conclusion: Surgical treatment of ovarian malignant growth, including para-aortic lymphadenectomy, ought to be performed distinctly at specific establishments as when radical ovarian disease medical procedure is performed at high volume focuses, the paces of precise organizing and ideal cytoreduction are far higher, and the related inconveniences and coming about postoperative bleakness are far lower than when similar medical procedures are performed at low volume focuses .Further huge scaled near investigations with longer follow up period are prescribed to assess the dismalness related with orderly lymphadenectomy in the executives of ovarian malignancy.
Introduction
Ovarian malignant growth (OC) is the seventh reason for disease passing around the world, and the 6th most basic malignant growth in ladies (Siegel et al., 2013). The sickness is frequently analyzed at a propelled stage, and therefore, the long-haul endurance of patients with ovarian disease ranges from 30% to 40% [1]. Metastasis to the Para-aortic lymph hubs (PALN) is the essential course of lymphatic spread in ovarian malignancy, and the high PALN over the secondrate mesenteric conduit (IMA) is an as often as possible included site. Another significant course for metastasis is through pathway enters the obturator and iliac hubs [2]. Retroperitoneal lymph hub contribution happens in 4-25% of ladies with early ovarian malignant growth, and 50-80% of ladies with cutting edge ovarian disease [3]. Nodal energy can’t be determined dependably either to have imaging or by intraoperative palpation [4], and hence, the best technique accessible for the recognition of nodal association is lymph hub dismemberment (LND) with histopathological assessment [5]. It has likewise been recommended that nodal metastases might be less touchy to fundamental chemotherapy, and therefore lymphadenectomy in patients with nodal metastasis is remedial [6]. Pelvic and para aortic LND is a fundamental piece of ovarian malignant growth organizing [7]. The basic role of LND in beginning time sickness is for organizing and to control resulting treatment. Notwithstanding, the main role in late-arrange infection is to accomplish ideal debulking [8]. Additionally, it has been indicated that lymphadenectomy in ovarian malignant growth patients has been related with more prominent in general 5-year endurance in both early and propelled organize sickness [9]. As indicated by the European Society of Medical Oncology (ESMO) Clinical Practice Guidelines, 30% of the cases at first named introductory stage ovarian malignant growth, were renamed in cutting edge illness after histopathological investigation of the lymph hubs. In patients with beginning time ovarian danger, the para-aortic lymph hubs were sure in about 9% of the cases with testing strategy, and 22% in cases with precise lymphadenectomy [10]. All in all, LND is a possible and well-endured careful system [11]. Notwithstanding, precise lymphadenectomy is troublesome and might be related with critical grimness. Horribleness is especially identified with intricacies that may happen during or after medical procedure and may prompt a more drawn out hospitalization and defer treatment [12]. Because of the danger of confusions identified with this procedure, the standard execution of lymphadenectomy in ovarian malignant growth patients is yet the subject of contention [13].
Aim of the Work
The point of this examination is to assess the result of the methodology of Para-aortic LND through laparotomy in the executives of patients with ovarian carcinoma.
Patients and Methods
Specialized plan
This investigation was an observational partner study did at the Oncology Department at Ain Shams University clinic. 72 patients experienced Para-aortic LND as a piece of medical procedure for associated early and propelled stages with ovarian malignant growth were remembered for the investigation during the period from August 2016 to June 2019.
Incorporation criteria
a) Patients experiencing organizing medical procedure for
suspected clear beginning period ovarian disease.
b) Patients experiencing Primary or interim debulking
medical procedure for suspected propelled arrange ovarian
malignant growth.
c) Patients were possibility for significant medical
procedure.
d) Eastern Cooperative Oncology Group (ECOG) execution
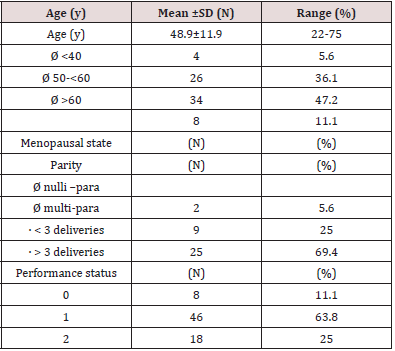
status (0-2) (Table 1).
Exclusion criteria
a) Patients with current malignancies.
b) History of past carefully and radiologically treated
abdominopelvic harm.
c) BMI >35.
Patients and methods
Histological analysis other than intrusive epithelial ovarian malignant growth.
Withdrawal criteria
a) Cases analyzed as unresectable propelled infection after
investigation what’s more, the activity was performed without
cytoreduction.
b) Cases with cutting edge ovarian malignant growth and
had remaining tumor after cytoreduction, in these cases Paraaortissc
analyzation was excluded. (Table 1): ECOG Performance
Status.
Grade ECOG
Fully dynamic, ready to continue all pre-infection execution
without confinement.
a) Restricted in physically strenuous action however
wandering and ready to do work of a light or stationary nature,
e.g., beacon work, office work.
b) Ambulatory and able to do all selfcare however incapable
to do any work exercises. Physically functional over half of
waking hours.
c) Capable of just constrained selfcare, bound to bed or seat
over half of waking hours.
d) Completely incapacitated. Can’t continue any selfcare.
Completely restricted to bed or seat.
e) Dead [14].
Ethical consideration
A composed educated assent structure was marked by every member with clarification of the administration methodology, potential risks and development.
Operational design
Patients in this examination were exposed to the accompanying.
History
a) Personal history: Age, living arrangement, occupation and
conjugal status.
b) Menstrual history: Menstrual example (premenopausal
or postmenopausal), history of sporadic uterine dying,
dysmenorrhea and date of last menstrual period.
c) Obstetric history: Gravidity and equality.
d) Present history: Analysis of the fundamental grievance
of female going to the outpatient center, with reexamining
different side effects and frameworks.
e) Contraceptive history: Type of the technique, term of use
and reason for stopping (whenever ended).
f) Family history of ovarian, bosom or colorectal malignancy.
g) Past therapeutic history: medicinal malady, medical
procedures and known medication sensitivity.
Clinical Assessment
Counting general, chest, stomach, pelvic and general lymph hubs assessment.
Investigations
a) Research center: Complete blood picture, glucose level,
renal capacity tests (Blood urea and serum creatinine), liver
capacity tests, coagulation profile, viral markers and tumor
markers (CA125, CA 19-9 and CEA.
b) Radiological imaging: This is finished by pelvi-stomach
US, chest X-beam, pelvi-stomach CT with differentiation and
chest CT just when shown.
c) Upper and lower GIT endoscopy for patients with unusual
manifestations or imaging discoveries reminiscent of GIT
contribution.
d) Heart assessment including ECG and ECHO for left
ventricular launch division for patients beyond 40 a year old or
in a patient with explicit signs or indications of cardiovascular
malady.
In the present investigation all patients with suspected ovarian
malignant growth experienced beginning assessment began with
physical assessment, research facility tests, and imaging. In the
present examination Pelvic ultrasound was commonly the principal
line imaging study used to portray any adnexal mass and we utilize
the accompanying sonographic qualities to be regularly connected
with an ovarian danger (Solid segment, Septations, if present, that are unpredictably thick (>2 to 3mm), Color or power Doppler show
of stream in the strong segment, peritoneal masses, developed hubs,
or tangled inside). In a critical number of patients, up to 20% had
uncertain US discoveries which require further imaging portrayal.
In this Situation, MRI was utilized as a critical thinking apparatus.
Serum biomarkers Included in the underlying assessment
were (CA)125 with shorts 35U/mL for postmenopausal ladies
and 20 to 200 U/mL for premenopausal ladies, CEA, and CA
19-9. In the present investigation CT with oral and intravenous
complexity before careful arranging and cytoreduction was utilized
to characterize malady degree which at that point illuminate’s
further administration in regard to reasonableness for essential
cytoreductive medical procedure or neoadjuvant chemotherapy.
CT criteria used to anticipate problematic careful result and
subsequently alluded patients for neoadjuvant chemotherapy in
the present investigation incorporated the accompanying:
CT criteria used to anticipate problematic careful result and subsequently alluded patients for neoadjuvant chemotherapy in the present investigation incorporated the accompanying:
a. Diffuse peritoneal thickening or embeds.
b. Large omental building up.
c. Diffuse upper stomach metastasis (tumor stores in
the porta hepatis, diaphragmatic stores, ailment in the
intersegmental crevice of the liver, lesser sac, little gut
mesentery and gastrosplenic tendon and parenchymal hepatic
sickness).
d. Pelvic sidewall association.
e. Extra stomach metastasis.
f. Massive ascites and pleural emission.
In the present examination Image guided omental biopsy
was done under US direction in all patients with cutting edge
OC regarded unsatisfactory for medical procedure clinically or
dependent on imaging requires histological affirmation of ovarian
threat before initiation of neoadjuvant chemotherapy. In the
present investigation all Patients with suspected clear beginning
time ovarian malignant growth dependent on clinical, research
facility and preoperative imaging thinks about were exposed to
formal arranging techniques including hysterectomy, reciprocal
salpingo-oophorectomy, peritoneal (washing, irregular peritoneal
biopsies, appendectomy with likely mucinous tumors and at any
rate infracolic omentectomy) and retroperitoneal(pelvic-and Paraaortic-
LND)organizing.
Ladies matured 40 years or more youthful, who were eager to
protect their potential childbearing, were enlisted for fruitfulness
saving medical procedure (essentially comprising in full careful
organizing with conservation of the uterus and in any event one
cylinder and the contra-horizontal ovary). Patients with cutting
edge organize ovarian malignant growth and not met the criteria
used to anticipate imperfect cytoreduction were exposed to
PDS pursued by adjuvant chemotherapy. Patients with cutting
edge organize ovarian disease and met the criteria used to
foresee problematic cytoreduction were oppressed ±3 courses of
neoadjuvant chemotherapy then IDS following (2 a month) trailed
by postoperative ±3 courses of adjuvant chemotherapy.
In the present examination, patients with cutting edge arrange ovarian malignant growth and were analyzed as unresectable propelled malady after investigation (I.e., patients with thick and vascularized grips, Extensive upper stomach illness or potentially Multiple spread knobs of carcinomatosis at the peritoneum surface or the outside of little and enormous gut) experienced careful investigation with tumor, peritoneal, or omental biopsy to affirm the analysis and were pulled back from the examination. Standard techniques of PDS or IDS comprise of absolute stomach hysterectomy, BSO, omentectomy (in any event infra-colic part) and complete debulking of metastatic tumors. Non-standard systems incorporate a solitary organ resection e.g., (small digestive system, colon, spleen) in the best approach to accomplish a total cytoreduction. Pelvic and para aortic LND was done just when complete cytoreduction was accomplished and discarded in patients with leftover sickness.
Careful Administration
Groundwork for medical procedure
Preoperative inside readiness: At least for 24 hours before medical procedure using:
a. Liquid and low buildup diet.
b. Intestinal disinfectant, for example, oral neomycin ±
metronidazole.
c. Laxative, for example, oral lactulose syrup.
Thromboprophylaxis
As 40-60mg Enoxaparin (Clexane) is allowed 6-12 hours preoperatively as SC infusions, at that point like clockwork for at any rate 7-10 days.
Perioperative anti-infection prophylaxis
As 2 grams cefotaxime (ceftriaxone vial) and metronidazole infusion (flagyl trickle) inside 2 hours before medical procedure, intraoperative rehashed portion might be given particularly in systems that most recent a few hours. Postoperative anti-infection agents were given in IV course for the primary 48h postoperative then patients proceeded on oral routine for 7 days.
i. Preparation of perfect blood.
ii. Intensive consideration unit (ICU) accessibility.
iii. Anesthesiologist assessment.
iv. Patient assent.
Careful systems
a) Abdominal passage through a midline vertical entry point
in the skin from the umbilicus to the pubic bone, at that point
stretched out superiorly past the umbilicus to pick up adequate
presentation to the upper mid-region.
b) Peritoneal wash/ascitic liquid drainage for cytology
c) Thorough investigation of the stomach and pelvic holes,
examination and palpation of every single peritoneal surface.
d) Total hysterectomy and two-sided salpingo-oophrectomy.
e) Omentectomy, in any event infracolic omentectomy was
finished.
Pelvic and para-aortic LND (a standard advance in careful
arranging of clear beginning period and in patients with cutting edge
sickness accomplished ideal cytoreduction). It was accomplished
for all patients.
Para-aortic LND was done from the left renal vein cranially to
the midpoint of the normal iliac vessels caudally and along the side
to the psoas muscle and the ureters, permitted full perception of
adventitia of IVC, aorta and left renal vessels, psoas muscles and
sacrum. In the present study the procedure used to access the
retroperitoneum for Para-aortic LND was as follow. The entrail was
tenderly uprooted until the base of the mesentery was uncovered.
An entry point was made in the peritoneum over the correct
normal iliac supply route and was stretched out cephalad along the
aorta to the degree of the duodenum. Dissection was done inside
the areolar plane between the lymph hubs and the peritoneum.
Para-aortic LND was then performed with the utilization of either
chilly scissors or electrocautery and with a De Bakey forceps. The
dismemberment was started over the aorta and continued in an
average to sidelong evacuating all the fibro-greasy tissue with
the lymph hubs till skeletonization of the aorta and IVC. Dainty
pedicles are made before transection so that puncturing veins
could be recognized. Infrarenal hubs: on the left side, the plane
of dismemberment is over the foremost surface of the aorta.
Presentation was encouraged by analyzing the areolar tissue
underneath the duodenum and afterward delicately withdrawing it
cephalad. The ureter was withdrawn along the side by the partner.
The left nodal pack is transected close to the degree of the left renal
vein.
On the correct side, analyzation was conveyed up to the level
between the ovarian vein and the privilege renal vein. The privilege
renal vein was frequently not pictured.
a) Appendectomy (for mucinous histology).
b) Maximal debulking of any metastatic tumors.
c) Intraperitoneal channel addition.
d) Wound conclusion: the stomach divider cut is shut with
a mass conclusion strategy utilizing monofilament postponed
absorbable suture (PDS circle number 1). Skin shut with careful
stapler after addition of subcutaneous vacuum channel.
All examples expelled were stamped and sent for
histopathological assessment for affirmation of conclusion,
reviewing, and lymph hub.
Information extraction
Illustrative information of the present investigation:
A. Patient attributes
B. Tumor attributes.
C. Surgery results
1. Surgeries.
2. Assessment of careful result: total cytoreductive medical
procedure in cutting edge ovarian malignancy characterizes just
like no naturally visible lingering ailment by any means.
3. Assessment of perioperative parameters: Total Operative
time, para-aortic LND time, the complete usable blood misfortune,
blood misfortune identified with para-aortic LND, intra and
postoperative blood transfusion, ICU affirmation, Period of
postoperative ileus and postoperative emergency clinic remain.
Evaluated intraoperative blood misfortune depended on
employable and anestheologist’s notes. The doused towel implies
around 150 cc blood misfortune and the drenched wipe implies
5cc. notwithstanding the sum in the suction compartment in the
wake of subtracting the measure of ascitic liquid or liquid utilized
for washing. Time of postoperative ileus was estimated from
recuperation of anesthesia till first go of flatus. Postoperative
emergency clinic remainPatients was released when they were sans
fever, walking, have no useful weakness of the bladder, they can
endure a delicate eating routine and their agony is gentle and can
be assuaged by oral medicine alone. Postoperative medical clinic
remain was characterized as the quantity of days in the emergency
clinic from the main postoperative day.
4. Assessment of perioperative morbidities and mortalities:
Bleakness information assessed by; entrail/bladder damage,
ureteric damage, vascular damage, drain, relaparotomy, profound
venous thrombosis (DVT), aspiratory embolism, lower appendages
lymphedema, symptomatic lymphocele, fistula and wound
recuperating issues.
Information the board
PC utilizing Statistical Package of Social Services adaptation 22 broke down the gathered information (SPSS) (IBM., 2015), Data was spoken to in tables and charts as mean + standard deviation, middle and range for quantitative factors and as number and rate for subjective factors.
Results
This examination was directed at the Department of Oncology
Ain Shams University emergency clinic and planned to assess the
exhibition of para aortic LND through laparotomy in the board
of ovarian malignant growth. At first, 82 Patients experienced
medical procedure for associated early and propelled stages with
ovarian malignant growth were remembered for this examination.
72 patients experienced Para-aortic LND as a piece of medical
procedure and 10 cases were pulled back from the outcomes, (Paraaortic
LND was excluded).
Table 1 show that the scope of age was (22-75) years. The
most elevated recurrence was seen in the age class between 50-<
60 years (47.2%). In the present examination, 22 patients (30.6%)
of the contemplated gathering were premenopausal, 50 patients (69.4%) were postmenopausal. As respects the equality, 2 patients
(5.6%) were nullipara, 34 patients (94.4%) were multipara. most
of the patients remembered for the examination (63.8%) had ECOG
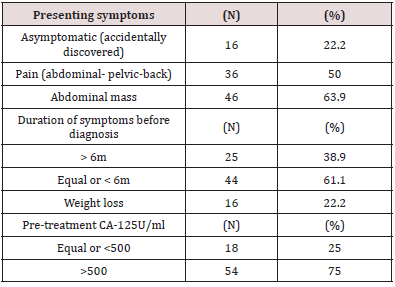
execution status 1as appeared in (Table 1). The most incessant
indications among patients in this investigation were gastrointestinal
side effects and stomach extension (77.8% of cases)trailed
by stomach/pelvic/back torment (half 0f cases), weight reduction
and exhaustion (22.2% of cases), stomach mass (63.9% of cases)
and urinary side effects (11.1% of cases). Practically all patients
were giving more than one indication. Most patients (61.1%) are
analyzed following a half year of indications. 54 patients(75% of
cases) had CA125 > 500U/ml. CA125 level ran from (212 -10180U/
ml and the middle was 775U/ml as appeared in (Table 2).Tumor
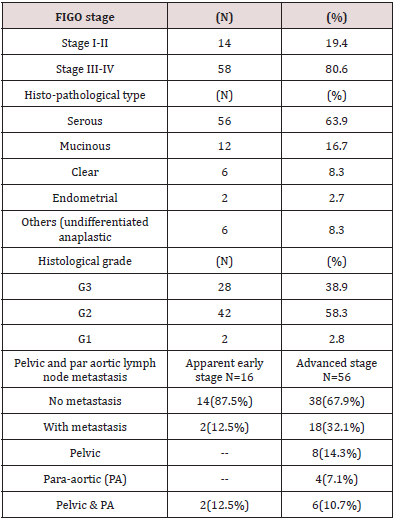
attributes: After careful assessment, 58patients (80.6%) had FIGO
organize III-IV ovarian malignant growth and 14 patients (19.4%)
had FIGO arrange I-II as appeared in (Table 3). One patient was
upstaged after proper organizing of 8 cases with clear beginning
period ovarian malignant growth.
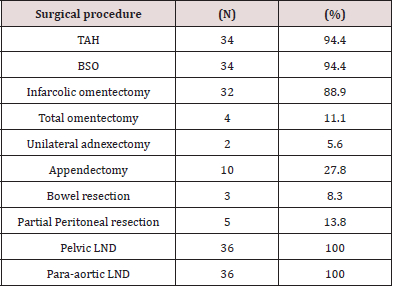
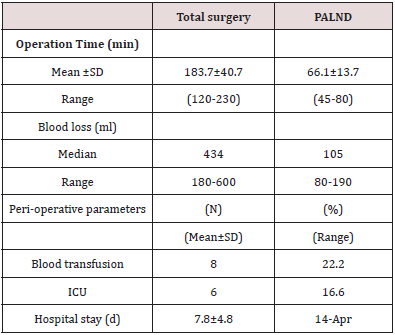
With respect to obsessive kinds, 46 patients (63.9 of cases) were analyzed as serous adenocarcinoma which is the most widely recognized sort of epithelial ovarian carcinoma. The vast majority of the patients (58.3%) in the present investigation had reasonably separated tumor (G2) and one of them was (G1) .The scope of recovered RT and LT pelvic lymph hubs was (9-17) with middle (11) hubs, the scope of recovered PA lymph hubs was (5-11) with middle (8) hubs, (Table 3) shows that 2 patient (12.5%) of 16 patients with clear beginning period ovarian malignant growth was upstaged to cutting edge organize after careful arranging which uncovered pelvic and PA nodal metastasis. 18 patients (32.1%) of 56 patients with cutting edge arrange ovarian disease had pelvic and Paraaortic nodal metastasis, 8 patients (14.3%) with just positive pelvic hubs, 4 patients (7.1%)with just positive Para-aortic hubs and 6 patients (10.7%) had both pelvic and Para-aortic nodal metastasis (Table 3). In the present examination, Pelvic lymphadenectomy (pelvic LND) and para-aortic lymphadenectomy (para-aortic LND) were performed to all patients (100% of cases) all out stomach hysterectomy and reciprocal salpingo-oophorectomy (TAH+BSO) were performed for 34 patients (94.4%), two patients (5.6%) had one-sided adnexectomy as a piece of richness conservation medical procedure, infra-colic omentectomy was performed in 32 patients (88.9), four patients (11. 1% of cases) had likewise supracolic omentectomy, 3 patients (8.3% of cases) had inside resection and essential anastomosis, five patients (13.8) had incomplete peritoneal resections, in conclusion, appendectomy was performed in 10 cases (27.8%). as appeared in (Table 4). Table 5 shows that the entire activity time from skin entry point to skin conclusion was inside a range (120-230 minutes) and the scope of entire blood misfortune was 180-600ml. The interim of PALND was around 65min, and the middle volume of blood misfortune related with PALND was roughly 105ml. 16 patients (22.2%) of cases got intra and post-usable blood transfusion, the scope of clinic remain for all patients was (7-14 days). Just 12 patients (16.6%) were admitted to ICU.
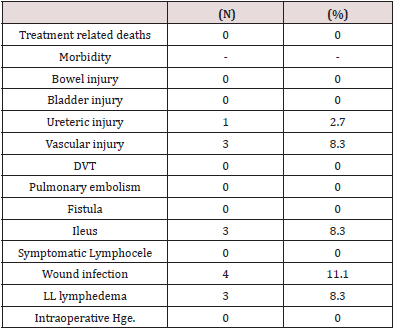
Table 6 shows that there was no treatment-related passing. Neither gut, bladder damage nor drain had happened during medical procedure. 2 patient (2.7% of cases) had ureteric damage and 6 patients (8.3%) had vascular damage during medical procedure. 6 patients (8.3%) had lower appendage lymphatic edema, 6 patients (8.3%) had crippled ileus and 8 patients (11.1%) had postoperative injury contamination. No patient had profound venous thrombosis (DVT) pneumonic embolism, fistula or symptomatic lymphocele.
Discussion
Numerous specialists revealed that the rate pace of paraaortic
lymph hub metastasis in beginning time ovarian malignant
growth extended from 4.3% to 8.6% [15] In a manner to keep away
from para-aortic lymphadenectomy in early ovarian malignancy.
The choice to perform lymphadenectomy should consider the
histological kind, the level of separation, and the CA-125 level at
the hour of conclusion [9]. The present examination researched the
pervasiveness of LN inclusion in a little arrangement of beginning
time epithelial ovarian disease experiencing retroperitoneal
organizing (N=16), we watched a relative high predominance of
LN contribution in beginning period epithelial ovarian malignant
growth, representing about 12.5%, These discoveries are steady
with the information of different investigations announcing that up
to 30% of early ovarian malignancy patients have positive lymph
hubs [16,17].
In Ovarian malignant growth, most of the patients influenced
are determined to have propelled phase of ailment (organize III
and IV as indicated by FIGO arranging framework). (In our study,56
patients (77%) determined to have propelled organize ovarian
malignant growth of each of the 72 ovarian disease patients),
In those patients, a lymph hub dismemberment is less helpful
prognostically and to manage treatment choices than for the patient
determined to have malady limited to the ovaries. However, it is as
yet imperative to evacuate suspicious or horribly extended hubs in
patients with cutting edge sickness experiencing tumor debulking
with the objective of ideal cytoreductive medical procedure [18].
The restorative job of lymphadenectomy in patients with
cutting edge ovarian disease is the subject of different clinical
investigations. Evaluation of its noteworthiness is troublesome as
the nearness of different variables may influence the visualization
in this gathering of patients. Moreover, a few specialists stress the
way that, because of the broad idea of the technique, the danger
of confusions is high, and the choice to execute lymphadenectomy
ought to be gone out on a limb in the wake of weighing both the
danger of entanglements and conceivable advantages’ Boas et al
indicated that in patients with no leftover ailment, lymphadenectomy
expanded middle endurance. For patients with little remaining
ailment, lymphadenectomy had no huge effect [19]. All the more as
of late in 2016, a meta-examination of 14 investigations including
3488 patients affirmed improved by and large endurance rate
in patients experiencing precise lymphadenectomy even with
residua tumors accomplishing 2cm [20]. The recently referenced
examinations still needed level-one evidence with respect to the
job of lymphadenectomy in cutting edge arrange. Then again,
Abe et al, revealed that efficient lymphadenectomy in cutting
edge ovarian malignant growth doesn’t appear to be useful [3].
Moreover, the aftereffects of the LION study were first exhibited
at ASCO 2017, This preliminary indicated that normal pelvic and
paraaortic lymphadenectomy in patients after naturally visible
complete tumor resection and with clinically negative lymph hubs
couldn’t improve malady free or generally endurance. In any case,
after production of consequences of LION study, numerous creators
begin to pose the inquiry, Is LION study is sufficiently amazing to
move the act of methodical lymphadenectomy in cutting edge
phase of ovarian malignant growth? However, the suggestions
concerning lymphadenectomy in cutting edge phase of ovarian
malignant growth remains debatable. In the present investigation
and dependent on the above information, it was the polof the careful
group to perform routine broad LND in every single propelled
case just when complete cytoreductive medical procedure was
accomplished and to be discarded in patients with leftover illness.
After distribution of the aftereffects of the LION study after
consummation of cases remembered for this examination, we
began to talk about training movement to resection of cumbersome
hubs after plainly visible complete tumor resection in patients with
cutting edge ovarian cancer. Women with cutting edge infection in
our territory keep on accepting problematic careful care.
We make the honorable stride of institutionalizing the careful
way to deal with ladies with cutting edge ovarian concentrating
on a multidisciplinary way to deal with malady the executives that
breezes through recognizing the basic commitment of the specialist
at each progression in the sickness procedure, unmistakably
sketching out and formalizing proposals for this illness, just as
perceiving the estimation of all suppliers with the accessible
assets in thinking about ladies with cutting edge ailment. this
multidisciplinary approach permits advancement of the treatment
procedure, considering patients’ attributes (age, execution/
healthful status, comorbidities, practical status) and tumor
dispersion (assessed pre-and intraoperatively). Likewise, this
treatment methodology attempt to adjust the need to maximally
draw out the movement free interim and limit treatment-related
morbidities. In the manner to accomplish this system, the treatment
idea of IDS has been presented as the neoadjuvant chemotherapy
is by all accounts noninferior to forthright medical procedure
[21] while adjuvant chemotherapy is related with improved
generally speaking and movement free endurance [22]. In this
elective administration approach the underlying treatment in
some progressed ovarian carcinoma patients ordinarily comprises
of 3 courses of chemotherapy pursued by cytoreductive medical procedure and extra three courses of postoperative chemotherapy.
It turns into an elective treatment for patients with low execution
status and those with obviously. unresectable tumors. Proposed
focal points of IDS incorporate an expanded pace of ideal
cytoreduction, less broad medical procedure, diminished blood
misfortune, lower dreariness, abbreviated emergency clinic remain
and improved personal satisfaction [23]. In this investigation, 46
patients of every one of the 56 patients with cutting edge organize
ovarian malignancy met the CT criteria used to foresee problematic
cytoreductive medical procedure that incorporate (peritoneal
carcinomatosis, pelvic sidewall penetration, and broad upper
stomach illness over stomach, liver, porta hepatis, mesentery,
and inside), these patients got platinum based convention as
neoadjuvant chemotherapy after austere cytology goal with cell
square as well as histology of percutaneous picture guided biopsy
(genuine cut) trailed by IDS whatever their response for ovarian
carcinoma, there is discussion about the degree of analyzation
(complete lymphadenectomy versus lymph hub examining) and
the anatomic degree of dismemberment that is required (i.e., pelvic
with or without paraaortic hubs), (i.e., Complete PAL (incorporates
infrarenal and suprarenal up to the coeliac trunk to midpoint of basic
iliac vessels), Infrarenal PAL (as above, yet does exclude suprarenal
dismemberment) and IMA-PAL (as above, however does exclude
dismemberment above IMA).Selective or arbitrary inspecting of
hubs from the pelvis or potentially the paraaortic district has been
depicted and is less exhaustive or complete contrasted and a lymph
hub dismemberment (lymphadenectomy).
On the off chance that particular hub testing is performed, hubs
are normally envisioned and palpated and examined in the event
that they are suspicious for metastatic sickness (Eg, augmented
to >1cm, adjusted rather than oval, hard, self-destruct when
dissected). But, lymph hub metastases are available in non-massive
hubs and have a breadth estimating exceptionally close to 2mm,
so palpation of lymph hub metastasis is anything but a sheltered
assessment technique [24]. Moreover, all accessible radiological
systems, for example, ultrasound, Magnetic Resonance Imaging,
Computer Tomography or Positron Emission Tomography are
likewise unfit to recognize lymph hub metastasis correctly [25]. in
view of these information, Selective or irregular inspecting is by and
large of little incentive aside from when executed as a component
of a conventional sentinel hub distinguishing proof method
and evaluation of paraaortic hubs ought to be through finished
dismemberment. Lymphatic seepage from the pelvic viscera
may continue in a stepwise manner from the pelvic to the lower
and afterward upper aortic lymph hubs; nonetheless, lymphatic
channels from the ovaries, fallopian cylinders, and uterus may
likewise deplete legitimately into the lower and upper paraaortic
nodes.
The lymphatic waste from pelvic viscera to the paraaortic hubs
is mind boggling and includes both ipsilateral and contralateral
associations notwithstanding direct lymphatic channels that may
sidestep the pelvic waste bowl. Also, ovarian lymphatics can deplete
legitimately to the paraaortic hubs over the degree of the mediocre
mesenteric supply route. In light of the above information, In the
present investigation LND included both the pelvic and aortic
lymph hubs up to degree of renal vessels, which is in concurrence
with distributed arrangement [26]. In this examination, 2patient
(12.5%) of 16 patients with clear beginning period ovarian disease
was upstaged to cutting edge organize after careful arranging which
uncovered pelvic and PA nodal metastasis.18 patients (32.1%) of 56
patients with cutting edge organize ovarian malignancy had pelvic
and para-aortic nodal metastasis, 8 patients (14.3%) with just
positive pelvic hubs, 4patients (7.1%)with just positive para-aortic
hubs and 6 patients (10.7%)had both pelvic and para-aortic nodal
metastasis. As per a novel careful order framework prescribed
by Pomel et for para-aortic hub evaluation [26], in the present
investigation the method applied in basically all cases experienced
paraaortic hub appraisal was broad para-aortic hub inspecting
(incorporates para-aortic regions, that permit full representation of
adventicia of aorta,IVC, renal vessels, psoas muscles and sacrum).
All patients experienced exploratory laparotomy with a midline
vertical entry point reaching out from the symphysis pubis to
simply over the umbilicus or the xiphisternum. Lymphadenectomy
was done after cytology, finishing of all out-stomach hysterectomy,
respective salpingoopherectomy and omentectomy. Deliberate
LND (pelvic and paraaortic) was performed after introduction of
the retroperitoneal space beginning caudally from the iliac vessels
at that point heading cranially skeletonizing the sub-par vena cava
then the aorta and expelling all the fibro-greasy tissue with the
lymph hubs till skeletonization of the vessels. We utilized either
cool scissors or electrocautery during LND. Bilateral pelvic LND
included outside iliac lymphadenectomy pursued by presentation
of the obturator fossa up to the degree of bifurcation of the regular
iliac vessels.
The PALND included dismemberment of the lymphatics from
the common iliac vessels up to the degree of left renal vein crossing
the aorta todrain into the second-rate vena cava and along the side
to the psoas muscle and the ureters. It is expressed that a radical
pelvic lymphadenectomy should yield in any event 9 to 27 hubs and
a para-aortic lymphadenectomy somewhere in the range of five and
12 hubs [15]. Our examination demonstrated that a scope of (9-17)
hubs gathered from the pelvic territory and (5-11) hubs from the
para-aortic area, this relative more modest number of hubs because
the method applied was testing instead of complete efficient
dismemberment. Careful inconveniences in ladies experiencing
a pelvic and paraaortic lymph hub analyzation are multifactorial
and normally identified with the patient age, existing patient
comorbidities, careful methodology, usable term, and simultaneous
surgeries [27,28]. pelvic and para-aortic LND is testing and may be
related with high danger of both intraoperative and postoperative
occasions, including the event of extreme difficulties and sequelae,
in this way affecting on patients personal satisfaction and
possibly on oncologic results (because of the postpone arranged
chemotherapy, when required) [29]. Because of the danger of
difficulties identified with this system, the normal execution of
lymphadenectomy in ovarian malignant growth patients is as yet
the subject of debate. Along these lines, the present investigation
planned to assess the recurrence and nature of intraoperative and
postoperative entanglements in ovarian malignant growth patients
treated with medical procedure including para aortic LND.
Intraoperative complexities: Although we have begun uniquely in the ongoing years to rehearse along these lines of para-aortic nodal evaluation in type of complete LND, just scarcely any intraoperative intricacies happened in direct connection to the paraaortic lymphadenectomy. The aftereffects of the present investigation indicated that the most regular intraoperative entanglements were vascular damage in 6 patients and urinary framework damage in 2 patients. The occurrence of significant organ and vessel damage identified with lymphadenectomy is low [30]. In the present examination and during the absolute first technique performed, one patient had IVC little tear quickly fixed by 5/0 vicryl and two patients had mediocre mesenteric vascular damage promptly cinched and ligated. The analyzation of the fat retroperitoneal tissue that contains the lumbar-aortic lymphatic ways is generally simple since it exists a decent dismemberment plane regarding vascular adventitia. Clear presentation and cautious analyzation of the retroperitoneal vessels, information on the probability of some vascular inconsistencies, particularly venous, acing basic methods of vascular suture and guaranteeing the presence of 4-0 or 5-0 strings add to bring down fundamentally the difficulties chance and their simple and quick tackling on the off chance that they show up. In the present investigation 2 patients had ureteric damage happened during left para aortic LND, analyzed intraoperative and quickly fixed utilizing 5/0 polyglactin sutures over a stent, at that point evacuated by a cystoscope 2weeks postoperatively. All iatrogenic wounds were constrained by the careful group with no help from different specialists from other related controls aside from two instance of IVC damage when a vascular specialist joined for consultation. In the present examination 4 patients (5.5%) had ripeness safeguarding medical procedure, 12 patients (16.7%) experienced formal careful organizing in assumed beginning period ovarian disease, 10 patients (13.9%) had PDS and 46 patients (64%) had IDS.
This makes wide varieties in the all-out usable time, the all-out blood misfortune and the requirement for intra and postoperative blood transfusion, yet, we consider the major surgery performed in this examination was interim debulking medical procedure. In this manner the outcomes will be contrasted and IDS of other trials. In present examination, absolute activity time run was (120-230 minutes) which was in a range with information of past preliminaries. Efficient survey of fifteen preliminaries gave an account of activity time found that general activity time ran from 95 to 276 minutes and the patients of NACT arms invested shorter energy in medical procedure (10-65 minutes) not as much as patients of essential medical procedure arms, this was frequently not measurably noteworthy. This could maybe be clarified by the littler volume of tumor that would be respected and the lesser degree of careful resections required to get ideal lingering ailment status [31]. The term of para-aortic lymphadenectomy is pretty much than 60 minutes (mean 66.1±13.7 and extend 45-80m) and the middle volume of blood misfortune was (105ml).
In an examination distributed in 2016, Comparing the dreariness between patients in the Inframesenteric para aortic dismemberment (IMLN)and infrarenal paraaortic analyzation (IRLND) gatherings, the middle volume of blood misfortune in IR-LND was 100ml [32]. The consequences of our examination are halfway in concurrence with aftereffects of the huge randomized LION Lymphadenectomy In Ovarian Neoplasms Gynecologic Cancer Intergroup preliminary, Lymphadenectomy, contrasted and no lymphadenectomy, required an extra hour of medical procedure (mean time: 340 versus 280min; p < 0.001), brought about 150ml more noteworthy blood misfortune (middle volume: 650 versus 500mL; p < 0.001). additionally, the aftereffects of our examination are halfway less or in concurrence with those of an investigation by Panici et al. One of the points of the investigation by Panici et al was the evaluation of perioperative complexities.
The specialists affirmed that the middle time of medical procedure was longer by around 90min in patients experiencing lymphadenectomy, and the middle volume of blood misfortune was higher by roughly 350 ml, when contrasted with the gathering with no lymphadenectomy [33]. In present examination, 8 patients (22.2%) got intra and postoperative blood transfusion, the scope of medical clinic remain for all patients was (7-14) days. These results are good with that revealed in the writing. Four preliminaries revealed that blood transfusion was required in (18-57%) of patients with measurably huge contrast among PDS and IDS in just two preliminaries [34]. Admission to ICU speaks to a critical expense to the social insurance framework [35]. Patients with cutting edge arrange ovarian malignant growth frequently require ICU-level of care. More seasoned age, more noteworthy ailment weight and increasingly extreme medicinal comorbidities have all been referred to as components inclining ovarian malignancy patients to ICU affirmation at the hour of medical procedure [29]. In the present examination the pace of postoperative ICU affirmation was generally low (16.6%). This might be clarified by diminished employable time, decreased intraoperative blood misfortune, exclusion of poor careful candidates and IDS in patients with extraordinary sickness trouble. most of the patients have been conceded for observing hardly any hours after medical procedure.
Pepin, et al, announced that 7% of patients experiencing debulking medical procedure required ICU confirmation [36]. This rate is on the lower end of what has been recently detailed in different examinations, with ICU confirmation in this patient populace answered to run somewhere in the range of 6% and 39 [37]. In present examination, the postoperative medical clinic stay was in arrange of (7-14 days). Thus, past preliminaries report a scope of (4-12 days) emergency clinic remain in patients got IDS contrasted with a scope of (5-20 days) for patients with PDS [38].
Postoperative Complications
All patients were followed up for 3 weeks after medical
procedure, patients encouraged to be followed up at Gynoncology
center each Wednesday in the wake of being released
for 3 weeks after medical procedure. There were no postsurgical
treatment-related passings. In the present examination, the most
regular postoperative confusions were ileus (8.3%), LL lymphatic
edema (8.3%) and significant injury recuperating complexities
(11.1%). These confusions settled with suitable administration inside about fourteen days. A large portion of our patients had
the option to restart their chemotherapy inside 3 weeks of
medical procedure and without a higher danger of hematologic or
irresistible inconveniences. No patient had drain, relaparotomy,
profound venous thrombosis (DVT), aspiratory embolism, fistula or
symptomatic lymphocele. The frequency of postoperative ileus was
8.3%, however practically every one of the patients were restored
inside seven days without careful treatment.
Lymphedema is the most widely recognized intricacy of pelvic
and paraaortic lymphadenectomy, announced in 1.5 to 28 percent
of patients. This is likely lower than the real frequency, since this
intricacy is probably going to be underreported in review reports
[39]. In the present investigation 6 patients (8.3%) had lower
appendage lymphedema and introduction was by and large very
factor. A few patients just notice some expanded lower leg growing,
others saw edema reached out from the feet to the stomach
divider. Another potential entanglement identified with nodal
dismemberment is lymphocele. In a forthcoming investigation
of 800 ladies who experienced performance pelvic or potentially
paraaortic lymphadenectomy for gynecologic malignancy, the
pace of lymphocele was 20 percent, and the pace of symptomatic
lymphocele was 6 percent [40] In the present examination no case
gave symptomatic lymphocele, asymptomatic lymphocele may pass
unnoticed as normal imaging postoperative not done.
At long last, the principle impediments of this examination
were the little example size, nonappearance of coordinated near
gathering treated without lymphadenectomy, the brief time of
follow up which isn’t sufficient to remark on tolerant endurance
and the all-out lymph hub check recovered was generally little.
This may bring about the underestimation of the occurrence of
nodal metastasis in our study or underestimation of perioperative
result. Then again, in the present investigation all precise
lymphadenectomies were performed in a solitary emergency clinic
by one group that utilized the equivalent careful strategy to avoid
the predisposition of the potential impact of various methodologies
of lymph hubs’ gather and its complexities. Additionally, the lymph
hubs were analyzed by a similar pathology group. We trust that
Present examination gives data to help in the structure of future
investigations and conventions for overseeing ovarian malignancy.
Conclusion
This examination demonstrated that ovarian malignant growth
patients may securely experience far reaching organizing including
broad para-aortic lymph hub dismemberment in open medical
procedures without huge perioperative dreariness, whenever
gave via prepared gynae oncologists. In any case, efficient
lymphadenectomy is related with an expanded working time,
blood misfortune, blood transfusions, emergency clinic remain
and a higher rate of postoperative difficulties. Such information
is with regards to the consequences of every single randomized
examination in ahead of schedule or progressed ovarian malignant
growth [41].
Likewise, bleakness related with deliberate lymphadenectomy
through laparotomy in ovarian malignant growth patients
particularly while performing fastidious analyzation around the incredible vessels up to the renal vessels ought not be viewed
as the factor that pushes the specialist to preclude lymph hub
dismemberment or move to lymph hub inspecting. However, the
choice to continue or not for a methodical lymphadenectomy ought
to be exclusively founded on oncological premise.
References
- Hunn J, Rodriguez GC (2012) Ovarian Cancer: Etiology, Risk Factors, And Epidemiology. Clin Obstet Gynecol 55:3-23.
- Kimmig R, Buderath P, Mach P, Rusch P, Aktas B (2017) Surgical treatment of early ovarian cancer with compartmental resection of regional lymphatic network and indocyanine-green-guided targeted compartmental lymphadenectomy (TCL, paraaortic part). J Gynecol Oncol 28(3):e41.
- Abe A, Furumoto H, Irahara M (2010) The impact of systematic para-aortic and pelvic lymphadenectomy on survival in patients with optimally debulked ovarian cancer. J Obstet Gynaecol Res 36:1023-1030.
- Harter P, Gnauert K, Hils R, Lehmann TG, Fisseler-Eckhoff A, et al. (2007) Pattern and clinical predictors of lymph node metastases in epithelial ovarian cancer. Int J Gynecol Cancer 17:1238-1244.
- Goff BA, Mandel LS, Melancon CH, Muntz HG (2004) Frequency of symptoms of ovarian cancer in women presenting to primary care clinics. JAMA 291:2705.
- Angioli R, Plotti F, Palaia I (2008) Update on lymphadenectomy in early and advanced ovarian cancer. Obstet Gynecol 20.34-39.
- Prat J (2004) Pathology of the Ovary. Philadelphia: Saunders.
- Mikami M (2014) Role of lymphadenectomy for ovarian cancer. J Gynecol Oncol 25:279-281.
- Zhou J, Shan G, Chen Y (2016) The Effect of Lymphadenectomy on Survival and Recurrence in Patients with Ovarian Cancer: A Systematic Review and Meta- Analysis. Jpn J Clin Oncol 46(48):718-726.
- Ledermann JA, Raja FA, Fotopoulou C, Gonzalez-Martin A, Colombo N, et al. (2013) Newly diagnosed and relapsed epithelial ovarian carcinoma ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol Suppl 6: vi24-vi32.
- Larson DM, Johnson K, Olson KA (2011)Pelvic and para-aortic lymphadenectomy for surgical staging of endometrial cancer: morbidity and mortality. Obstet Gynecol 79: 998-1001.
- Warwick J, Vardaki E, Fattizzi N, et al. (2009) Defining the surgical management of suspected early-stage ovarian cancer by estimating patient numbers through alternative management strategies. Br J Obstet Gynaecol 116: 1225-1241.
- Camara O, and Sehouli J (2009) Controversies in the management of ovarian cancer-pros and cons for lymph node dissection in ovarian cancer. Anticancer Res 29: 2837-2843.
- Oken MM, Creech RH, Tormey DC, Horton (1982)Toxicity and Response Criteria Of The Eastern Cooperative Oncology Group. Am J Clin Oncol 5: 649-655.
- Nomura H, Tsuda H, Susumu N, Fujii T, Banno K, et al. (2010) Lymph node metastasis in grossly apparent stages I and II epithelial ovarian cancer. Int J Gynecol Cancer 20(3): 341-345.
- Powless CA, Aletti GD, Bakkum-Gamez JN, Cliby WA (2011)Risk factors for lymph node metastasis in apparent early-stage epithelial ovarian cancer implications for surgical staging. Gynecol Oncol 122: 536-540.
- Harter P, Sehouili J, Lorusso D (2017) LION: Lympha-denectomy in Ovarian Neoplasms-A Prospective Randomized AGO Study Group Led Gynecologic Cancer Intergroup Trial. Journal of Clinical Oncology 35(15_suppl): 5500.
- Krasner C, and Duska L (2009) Management of women with newly diagnosed ovarian cancer. Semin Oncol 36(2): 91-105.
- Du Bois A, Reuss A, Harter P (2010) Potential role of lymphadenectomy in advanced ovarian cancer: a combined exploratory analysis of three prospectively randomized phase III multicenter trials. J Clin Oncol 28(10): 1733-1739.
- Zhou J, Shan G, Chen Y (2016) The effect of lymphadenectomy on survival and recurrence in patients with ovarian cancer: asystematic review and meta-analysis. Jpn J Clin Oncol 46(8): 718-726.
- Department of Gynecologic Tumor, Zhejiang Cancer Hospital, International Journal of Gynecological Cancer, Hangzhou, Zhejiang Province, China, pp. 944-952.
- Paulino E, Nogueira Rodrigues A, Strasser-Weippl K, St. Louis J, Bukowski A, et al. (2017) Barriers to Primary Debulking Surgery for Advanced Ovarian Cancer in Latin America. Int J Gynecol Cancer 27(8):1645-1649.
- Chung YS, Kim Y-J, Lee I (2017) Impact of neoadjuvant chemotherapyand postoperative adjuvant chemotherapy cycles on survival of patients with advanced-stage ovarian cancer. PLoS One 12(9): e0183754.
- Feuer DJ, Broadley KE, Shepherd JH (2000) Surgery for the resolution of symptoms in malignant bowel obstruction in advanced gynaecological and gastrointestinal cancer. Cochrane Database Syst Rev 1: CD002764.
- Ayhan A, Gullekim M, Celik NY (2007) Occult metastasis in early ovarian cancer: risk factors and associated prognosis. Am J Obstet Gynecol 196(81): e1-e6.
- Risch HA, McLaughlin JR, Cole DE (2001) Prevalence and penetrance of germline BRCA1 and BRCA2 mutations in a population series of 649 women with ovarian cancer. Am J Hum Genet 68(3): 700-710.
- Pomel C, Naik R, Martinez A, Ferron G, Nassif J, et al. (2011) Systematic (complete) para-aortic lymphadenectomy: description of a novel surgical classification with technical and anatomical considerations BJOG 119(2): 249-253.
- Galaal K, Bryant A, Fisher AD (2012) Laparoscopy versus laparotomy for the management of early stage endometrial cancer. Cochrane Database Syst Rev 9: CD006655.
- Lawrie TA, Medeiros LR, Rosa DD (2013) Laparoscopy versus laparotomy for FIGO stage I ovarian cancer. Cochrane Database Syst Rev 10: CD005344.
- Gallotta V, Ghezzi F, Vizza E (2016) Laparoscopic Management of Ovarian Cancer Patients with Localized Carcinomatosis and Lymph Node Metastases: Results of a Retrospective Multi-institutional Series. J Minim Invasive Gynecol 23(4): 590-596.
- Walker JL, Piedmonte MR, Spirtos NM (2009) Laparoscopy compared with laparotomy for comprehensive surgical staging of uterine cancer: Gynecologic Oncology Group Study LAP2. J Clin Oncol 27(32): 5331-5336.
- National Breast and Ovarian Cancer Centre and Australian Cancer Network (2008) Neoadjuvant chemotherapy in ovarian cancer: A systematic review. National Breast Ovarian.
- Clothilde P, Henri A, Louise G, Emmanuelle B (2016) Morbidity of Staging Inframesenteric Paraaortic Lymphadenectomy in Locally Advanced Cervical Cancer Compared with Infrarenal Lymphadenectomy. Int J Gynecol Cancer 27(3): 575-580.
- Panici BP, Maggioni A, Hacker N (2005) Systematic aortic and pelvic lymphadenectomy versus resection of bulky nodes only in optimally debulked advanced ovarian cancer: a randomized clinical trial. J Natl Cancer Inst 97: 560-566.
- Milam MR, Tao X, Coleman RL (2007) Neoadjuvant chemotherapy improves peri-operative outcomes in patients with advanced epithelial ovarian cancer. Annual Meeting on women's Cancer pp:152.
- Rota M, Pasquali E, Scotti L (2012) Alcohol drinking and epithelial ovarian cancer risk. A systematic review and meta-analysis. Gynecol Oncol 125: 758.
- Pepin K, Bregar A, Davis M (2017) Intensive care admissions among ovarian cancer patients treated with primary debulking surgery and neoadjuvant chemotherapy-interval debulking surgery. Gynecol Oncol 147(3): 612-616.
- Ruskin R, Urban R, Sherman A (2011) Predictors of intensive care unit utilization in gynecologic oncology surgery. Int J Gynecol Cancer 21(8): 1336-1342.
- Shimoji K, Ito K, Tashima (2017) Comparison between Primary Debulking Surgery and Neo-Adjuvant Chemotherapy Followed by Interval Debulking Surgery for Patients with Stage III-IV Ovarian Cancer. Gan To Kagaku Ryoho 44(8): 675-679.
- Todo Y, Yamamoto R, Minobe (2010) Risk factors for postoperative lower-extremity lymphedema in endometrial cancer survivors who had treatment including lymphadenectomy. Gynecol Oncol 119(1): 60-64.
- Zikan M, Fischerova D, Pinkavova I, Slama J, Weinberger V, et al. (2015) A prospective study examining the incidence of asymptomatic and symptomatic lymphoceles following lymphadenectomy in patients with gynecological cancer. Gynecol Oncol 137(2): 291-298.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...