Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Research Article(ISSN: 2637-4544) 
Assessment of Current Women’s Health Risks During the Prenatal Period-Implications for Midwifery Practice Volume 5 - Issue 2
Stefania Andrascikova1*, S Alena Schlosserova1 and Alexandra Archalousova2
- 1Department of Midwifery, Faculty of Health Care, University of Presov, Slovakia
- 2Department of Nursing, University Konstantin Philosoph of Nitra, Slovakia
Received:January 31, 2022; Published: February 11, 2022
Corresponding author: Stefania Andrascikova, Department of Midwifery, Faculty of Health Care, University of Presov, Slovakia
DOI: 10.32474/IGWHC.2022.05.000207
Abstract
Background: Assessment of risk factors affecting women’s health during pregnancy has been in the Centre of several researchers’ interest. However, there is a lack of studies investigating risk factors affecting women’s health during pregnancy in Slovakia.
Methods: A cross-sectional survey was used to investigate relationships among risk factors (age, genetics, education, social status and parity), selected laboratory parameters, and BMI during pregnancy. The study sample consisted of 104 pregnant women (whose health histories had detected risk factors) from four hospitals in the East Slovakia region. Data were collected by means of analysis of medical documentation and obtained during ward rounds., multi-factor ANOVA procedure was performed for the purpose of statistical analysis.
Results: 19.23% of respondents were ≥ 35 years old; 44.23% of the respondents showed genetic risk; 58.66 % of the respondents were primiparas, 32.70 % of the respondents completed elementary education; 31.77 % of the respondents had a lower social status. The mean value of BMI was 28.28 (SD 5.22), and obesity (BMI ≥ 29.1) was identified in 34.62 % of the respondents. We confirmed that parity (the number of times a female has given birth) was a significant factor in relation to the selected laboratory parameters (Tr, Urea, Cholesterol). BMI was not in significant relationship to the selected risk factors. Social status and education were synergic factors influencing women’s health status. Only one risk factor, i.e., parity was confirmed as a significant factor in relation to the selected laboratory parameters. Our study was only a pilot one with some limitations (e.g., non-representative sample coming only from one specific East Slovakia ragion, and specific laboratory parameters). Future research should include a representative random sample and general evaluation of health status during pregnancy (comorbidity, etc.). There were not many results found in literature sources dealing with the topics.
Keywords: Risk Factor; Pregnancy; BMI; Pregnant Women’s Health Status
Introduction
A risk factor is a lifestyle factor or an environmental factor that increases probability of defect, causes some health complications or, in general, increases extent and severity of related health complications. Diminution of risk factors is an important part of prevention and treatment. Risk factors can endanger a woman, foetus, and external or internal family environment. They factors can cause discomfort and partly endanger biological, psychological, and social needs. Risk factors occurring in a community can be divided according to age, genetic factors, biological characteristics, personal health habits, family history, lifestyle and environment. Health Risk Assessment represents a method used by midwives to determine qualitative or quantitative degree of health risks endangering women’s health and role; midwives have to take into account and expect potential negative effects on women’s health status or fulfilment of their roles [1]. Fundamental steps in risk assessment consist of danger identification-it means determination how negative risk factors affect women. They are e. g. polluted source of potable water, low hygiene standard-infectious disease risk; lack of food, incorrect diet composition-eating disorders of women-obesity, malnutrition; negative relationship of mother to her child-parent role acceptance disorder; tearfulness and increased emotional sensibility of woman-baby blues; ineffective nursing-low weight gain in a baby etc. The next step is assessment of the relationship between number of risk factors and their impact on bio-psycho-social status of women; identification of their ability or disability to adapt to changed life situation and to use their own compensation possibilities for coping with the problem situation; midwives assess degree of help needed and ways how to help the women. The assessment of exposition to risk is the third step specifying severity and duration of individual risk factors influencing women; it can be anticipated as a result of assessing the conditions women are exposed to, and of the effect and reaction to their influence as well; it means it is assessed if the risk factor has a short-time or long-time effect if the effect is continuous, intermittent or occasional, or if this phenomenon is constant or reversible. Risk classification means specification of the risk for a receiver by means of result synthesis - it means that midwives classify the risk as low, medium, or high. Risk assessment is a complicated process therefore its results must be assessed very carefully and responsibly. Following these steps, midwives draw up respective care plans for women and identify the priorities and methods to achieve the goal.
This research was performed due to increasing number of women attending risk pregnancy care centers. Risk factors influence the course of pregnancy negatively and may have negative impact on the overall women’s and fetuses’ heath. Taking a comprehensive health history and targeted detection of risk factors in prenatal care are known to help identify the risks [2]. Thanks to obtained information it is possible to detect thread to pregnancy early and thus to compile individual plans of care and nursing procedures to reduce their adverse impact on the course of pregnancy and women’s health. It is recommended to perform the prognostics and diagnostics of development of diseases during pregnancy in the early stage of pregnancy [3]. The respondent sample and data collection were performed in the Presov region, Slovakia-in the hospitals and prenatal care centers in Poprad, Prešov, Levoča and Bardejov. Pregnant women living in the settlements (mostly Roma ethnic population) were also included in the studied group as they show lower social standard and thus potentially higher incidence of investigated risk factors.
Materials and Methods
Selection criterion was pregnant women attending six risk pregnancy care centers. Out of 526 pregnant women 104 were monitored and statistically reported to have diagnosed risk factors influencing the course of pregnancy. Groups of variables - the most frequently occurring risk factors were created, i.e., qualitative variables-age, parity, genetics, education and social status-habitation; quantitative variables - BMI, blood pressure and laboratory values of blood tests. The division was based on literature sources dealing with risk factors [4,5] and aimed at their comparison with our results achieved in the investigated respondent group. As regards the age risk factor, there was no woman under the age of 19, the others were divided into two subgroups: women aged up to 34 and the ones over 35. Parity was examined in these categories: primiparas and multiparas. Multiparas included also some secundiparas which is a separate group in the obstetric practice. Genetics was assessed in two subgroups: women having the risk factor of predisposition to a genetic disease detected in their family health histories, and the ones with no genetic risk. On the basis of the estimated BMI the following subgroups were created: group 1: BMI of 1 to 19.8 (underweight), group 2: 19.9 to 26 (normal weight), group 3: 26.1 to 29 (overweight), group 4: 29.1 and higher (obesity). The subgroup of underweight women was omitted as no woman had BMI below 19.8. The factors of educational level and social status - habitation were divided into 3 subgroups, namely primary, secondary and university education; habitation: living in towns, villages and settlements. Living in a certain habitat represents a specific social status and lifestyle hence it includes a subset of latent factors, such as amount and quality of food, housing standards, lifestyle, etc. The achieved educational level influences lifestyle significantly and therefore contains lots of other potential factors [6]. The assessed information was obtained from medical documentation. Methods of frequency analysis enabling to evaluate relationships between variables, and descriptive statistics with the characteristics of average, median, standard deviation, minimum value, maximum value, and significance level for mean value of 95%. (≤ 0.05) were used.
Results
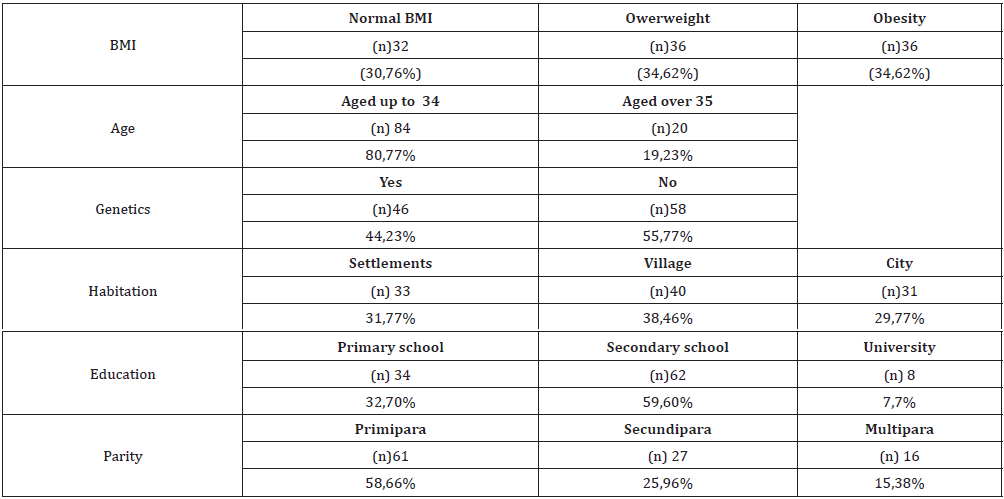
The frequency analysis shows the multiplicity of factor combinations. Age as an important risk factor can lead to diseases. Age risk factor for a disease occurred respondents aged up to 34 and in 20 (19.23%). Genetic predisposition was detected in 46 (44.23%) respondents, 58 (55.77%) were without any genetic risks. The investigated respondent sample included 61 primiparas (58.66%) and 43 multiparas (41.34%). Primary education was completed by 34 respondents (32.72%), secondary education by 62 respondents (59.60%) but university-educated respondents amounted to only four in total (7.7%). 33 respondents (31.77%) come from and live in settlements, 40 (38.46%) live in villages, and 31 (29.77%) come from and live in towns [7]. Body Mass Index showed a normal weight in 32 respondents (30.76%), overweight in 36 respondents (34.62%) and obesity in 36 respondents (34.62%). These results indicate that actually 69.24% of the respondents reached the level of overweight or obesity.
Frequency analysis showed the following results
Age Factor in Dependence on The Genetic Predisposition
The investigated group shows that genetic predisposition does not play any significant role in both respondent subgroups. But on the other hand, cases with genetic predisposition include 36.54% of respondents aged below 34 in comparison with 7.69 % of those aged above 35 [8].
Genetics Factor in Dependence on Habitation
In the investigated sample 23.08% respondents living in the countryside, 17.31% living in towns and 15.38% living in settlements are without any genetic predisposition. Genetic predisposition was found in 15.38% respondents living in villages and settlements, and in 13.46% of the ones living in towns. The result indicates that genetic factor does not depend on women’s habitation [9].
Disease Predisposition in Dependence on Parity
In the investigated group genetic predisposition to disease is negative in almost the same ratio in primiparas (26.92%) and multiparas (28.85%) as well as positive in the same ratio - 23.08 % of primiparas and 21.15% of multiparas. It means that in the examined sample age and parity are not significant factors contributing to a disease in the course of pregnancy [10].
Dependency of Genetic Predisposition Upon BMI
In the examined sample genetic predisposition was not found in 21.15% of respondents with the normal BMI and in 17.31% of overweight and obese respondents. 9.62% respondents with normal weight were at risk for genetic disease. 17.31% of women with genetic predisposition reach the level of overweight and obesity. The results indicate that overweight and obesity are synergic risk factors for genetic predisposition for diseases, e.g., preeclampsy [11].
Dependency of BMI on Age
In the investigated group aged up to 34, BMI categories 2, 3 and 4 were estimated in the same number of respondents, namely 26.92% of those with the normal weight, overweight, and obesity, In the group of respondents aged over 35, 3.85% of the respondents have the BMI category 2, which is the normal weight, and 7.69% are in the categories of overweight and obesity. From this it follows that the older pregnant women are, the more they suffer from overweight and obesity [12].
BMI in Dependence on Habitation
The investigated sample includes 9.62% of respondents living in settlements having the normal weight, 13.46% are overweight and 7.69% reached obesity; the same percentage of respondents living in the villages, i.e., 11.54% have the normal weight or overweight, and 15.34% are obese; the respondents living in towns belong equally to the categories of normal weight and overweight-9.62%, however, 11.54% of respondents suffer from obesity. From this it results that BMI category 2 occurs equally in all respondent groups, the number of women with BMI 3 is higher in those living in villages and settlements, but BMI 4, i.e., obesity is the problem of the most women living in villages and towns whereby the worst BMI score was found in the respondents living in villages [13].
BMI in Dependence on Achieved Education
In the examined group 11.54% of the respondents with primary education occur in the BMI category of normal weight, BMI 2, i.e. overweight occurs in 13.46%, and the index of obesity is reached by 7.69% of the respondents; as for the respondents with secondary education, 19.23% reaches the rate of normal weight and overweight, and 21.15% of the respondents are obese; none of the respondents with university education reaches the level of normal weight, 1.92% reaches BMI 3 i.e. overweight, and 5.77% reaches BMI 4 i.e. obesity [14].
BMI in Dependence on Parity
In the examined sample 17.31% of primiparas and 13.46% multiparas have the normal weight; 15.38% of primiparas and 19.23% of multiparas are overweight, the level of obesity is equally reached by 17.31% of both primi- and multiparas [15]. The Table 1 shows decomposition of BMI variance in relation to degree of contribution of individual factors. As the type III of sum of squared deviations had been chosen, every factor has been counted separately without any influence of other factors. Following the fact that in the studied respondent sample P-values of the statistical significance test do not reach the value below 0.05 it can be concluded that none of the factors influences the BMI value on the statistically relevant significance level of 95%. The result may be partly influenced by the size, of particular subgroups in certain factors [16].
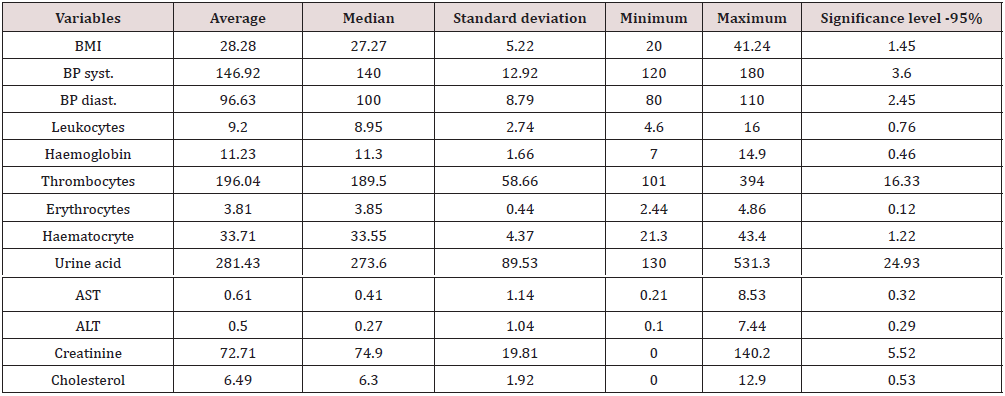
Multi-factor ANOVA procedure explains variances of quantitative variables by means of some factors, therefore more relevant relationships between quantitative variables (laboratory results) and qualitative variables (factors) have been searched for [17]. In correlation of qualitative (autonomous) variables (age, genetic predisposition, habitation, education, parity) and quantitative variables (laboratory values), the evaluation of the entire sample of 104 respondents shows the following average values: average BMI of 28.28 and median of 27.27 that is the category of overweight; average blood pressure is 146.92/96.63 mmHg with the median of 140/100 mmHg, what indicates potential preeclampsy in the respondents; AST average value of 0.61 μkat/l, with the median of 0.41 μkat/l what is not significant when the normal value is up to 0.52 μkat/l; average cholesterol level is 6.49 with the median of 6.30, as the at normal value is up to 5.18 it counts as increased level of cholesterol. Other parameters are within normal limits. Average laboratory results, BMI and blood pressure were evaluated in the descriptive statistics (Table 2).
All F-values come from Residual Average of square errors.
The cholesterol level in relation to parity was found to be statistically significant in the analysis of single quantitative variables correlating with the autonomous variable. As P-values of statistical significance test are below 0.05 only in one case, it can be concluded that only one factor influences the cholesterol value in the level of 95% statistical significance [18]. It is the case of parity. The descriptive statistics shows that the average and median are higher in primiparas than in multiparas, whereby both the averages reach a higher level than physiological value. The value of thrombocytes in relation to parity was found to be statistically significant in the analysis of single quantitative variables correlating with the autonomous variable (Tables 3-5). As P-values of statistical significance test are below 0.05 only in one case, it can be concluded that in the investigated sample only one factor statistically significantly influences the value of thrombocytes in the level of 95% significance. It is the case of parity. In the values of descriptive statistics, the average and median confirm that decrease of average thrombocyte values is statistically more significant in the primiparas than in multiparas.
All F-values come from. Residual average of square errors.
All F-values come from Residual average of square errors.
Discussion
Risk factors influencing health status of pregnant women and course of pregnancy are dealt with by lots of authors. Their studies confirm that BMI risk factor in relation to laboratory blood values is one of serious factors having negative impact on course of pregnancy and triggering certain deficiencies in woman’s and foetus’s health status [6] (Herring, 2009, Saldana,2006). Naftalin & Paterson- Brown (2008) explain that obese women’s health status becomes worse, and their bodies are less able to cope with risks attacking them. Other authors describe genetic risk factor that may affect woman’s and foetus’s health status and trigger some diseases, such as preeclampsy or diabetes mellitus (Andrews, 2005, Luczak, 2005, Mazouz,2011). Jasovic (2011) focuses on the issue of detection of the risk factors in women’s life that can influence their pregnancy and points out the risk factors of age and parity. Negative impact of higher cholesterol, age and BMI values on the development of woman’s health status and their possible impact on potential pregnancy is described by Gostinskij et al (2004) in the study of the WHO project Monica. They discovered the linear relationship between overweight and risk of cholesterol and confirm that obese women often have higher level of blood cholesterol than women of a healthy weight. But [7] says that BMI is only one way of measuring obesity, and it is not without its limitations; it is important to take a woman–centered approach and consider each woman as individual.
References
- Jasovic-Siveska E, Jasovic V, Stoilova S (2011) Previous pregnancy history, parity, maternal age and risk of pregnancy induced hypertension. Bratislavské lekárske listy: international journal for biomedical sciences and clinical medicine ISSN 0006-9248 112(4): 188-191.
- Dekker G, Gustaaf A, Sibai B (1998) Etiology and Pathogenesis. Current concepts. Am J Obstet Gynecology ISSN 1359-1375 179(5): 1359-1375.
- Gostinski M, Gutzwiller F, Kuulasmaa K (2004) Analysis of the relationship between total cholesterol,age,body mass index among males and female in the WHO Monica project. International Journal of obesity 28(8): 1082-1090.
- Drábková J (2001) Genetická predispozice k preeklampsii. Anest. Resuscit. Roč. 48, č. 4/5, s. 239, ISSN 1212-3048.
- Haelterman E, Marcoux S, Croteu A, Dramaix M (2007) Population-based study on occupational risk factors for preeclampsia and gestational hypertension. Scandinavian Journal of Work, Environment & Health. Stockholm 33(4): 304-317.
- Rosenberg TJ, Garbers S, Chavkin W, Chiasson MA (2003) Prepregnancy weight and adverse perinatal outcomes in an ethnically diverse population. Obstet Gynecol 102: 1022-1027.
- Allen R (2010) The risk of emergency caesarean in labour for the overweight or obese woman. Mirids Midwifery digest 20(4): 464-470.
- Aftlas A, Wang W, Rish H, Woolson R, Bracken M (1993) Prepregnancy body mass index and gestational weight gain as risk factors for preeclampsia and transient hypertension. College of Public Health University of Iowa City IA USA 2001. N Engl J Med 329: 1213-1218.
- Budde M, Lange L Dekker G, Chan N, Minh Nguyen (2007) Risk factors for placental abruption in a socio-economically disadvantaged Region. Journal of Maternal - Fetal & Neonatal Medicine 20(9): 687-693.
- Hájek Z (2004) a kol Rizikové a patologické tehotenství. 1vyd Praha Grada. 444s.ISBN 80-247-0418-8.
- Harrison PA, Sidebottom AC (2008) Systematic prenatal screening for psychosocial risks. J Health Care Poor Underserved 19(1): 258-276.
- Joy S, Istwan N, Rhea D, Desch C, Stanziano G (2009) The impact of maternal obesity on the incidence of adverse pregnancy outcomes in high-risk term pregnancies. Am J Perinatol 26(5): 345-349.
- Leifer G (2004) Úvod do porodnického a pediatrického ošetrovatelství. 1vyd Praha: Grada 915s. ISBN 80-247-0668-7.
- Nord M, Andrews M, Carlson S (2002) Household food security in the United States (FAN Research Report No. 35). Washington DC: USDA Economic Research Service 2003.
- Naftalin J, Paterson Brown S (2008) A pilot study exploring the impact of maternal age and raised body mass indexon cesarion sectionrates. Journal of obstetrics and gynecology 28(4): 394-397
- Parker B, McFarlane J, Soeken K (1994) Abuse during pregnancy: effects on maternal complications and birth weight in adult and teenage women. Obstet Gynecol. 8(3): 323-328.
- Pearce C, Easton K (2005) Management of complications in early pregnancy. Nursing Standard 19(34): 56-64.
- Thorstensen KA (2000) Midwifery management of first trimester bleeding and early pregnancy loss. In J Midwifery Women’s Health 45(6): 481-497.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...