Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1652
Review Article(ISSN: 2641-1652) 
Morphological Justification for Simultaneous Correction of Chronic Disorders of Duodenal Patency and Failure Bauhinias Flap in the Prevention of Guidance in the Esophagus and Stomach Volume 2 - Issue 2
Vladimir Leonidovich Martynov*
- Headquarters of the State Educational Establishment of the City of Nizhny Novgorod, Russia
Received:March 22, 2019; Published: March 29, 2019
*Corresponding author:Martynov VL, Headquarters of the State, Educational Establishment of the City of Nizhny Novgorod, Russia
DOI: 10.32474/CTGH.2019.02.000134
Abstract
In 37 patients under NBZ and HNDP conditions, 158 biopsy samples were taken from the esophagus SB (N = 29), cardial section of the stomach (N = 20), fundus of the stomach (N = 36), antrum (N = 36), with endoscopic examination. 12 - PC (N = 37). The morphological study revealed inflammatory changes in the mucous membrane of the upper digestive tract in all patients, its superficial inflammation was determined only in 29 preparations, diffuse inflammation (on all layers of the mucous membrane) - in 129 biopsies (82%), the active stage of inflammation - in 102 (65 %), atrophy - in 6, erosion - in 1 case. The obtained data reveal significant morphological changes in the mucous membrane of the digestive tract in conditions of reflux disease. A morphological analysis of the state of the mucous membrane of the esophagus, stomach, and 12-PC, performed in 12 patients before and after surgery, confirms the normalizing effect of PD in combination with DES, as the most adequate surgical tool for treating RB, on the indicated gastrointestinal sections.
Keywords: Chronic Violation of Duodenal Permeability; Failure of the Bauhinia Valve; Morphological Changes in the Mucous Membrane of the Esophagus and Stomach in Conditions Of Reflux Disease; Surgery of Reflux Disease; Prevention of Cancer of the Esophagus and Stomach
Introduction
The main pathogenetic factors in the development of diseases of the stomach in chronic impairment of duodenal permeability (CNV) are duodenogastric reflux (GHD) and motor-evacuation disorders of the stomach [1-3]. Many authors consider DGR as a factor in the formation of chronic gastritis [4-6], gastric cancer [7,8]. With increasing DGR, the epithelium of the antrum begins to atrophy, and as intestinal metaplasia occurs as an “defense reaction”, the resistance of the gastric mucosa decreases, and erosion is formed. Restructuring the coolant by intestinal type is regarded by a number of authors as a precancerous condition [7,9]. The emergence of this resonance, the realization of its pathological action is a consequence of chronic disturbance of duodenal patency (CNDP) and the failure of the bauhinia valve (NBZ) [10]. In our experience (more than 600 patients), HNDP and NBZ occur simultaneously in 94% of patients. Therefore, we believe that the concept of reflux disease should include this particular pathology, which entails a thick-intestinal reflux, DGR, gastroesophageal reflux, esophagolingual reflux, which requires the simultaneous surgical correction of CND and NBZ. The most adequate operational aid is Bauginoplasty in combination with duodenojejunostomy (DES).
Endoscopic examination of 37 patients in the NBZ and HNDP conditions took 158 biopsy specimens from the mucosa (CO) of the esophagus (N = 29), cardiac section of the stomach (N = 20), fundus of the stomach (N = 36), antral section of the stomach (N = 36), 12 - PC (N = 37). The morphological study revealed inflammatory changes in the mucous membrane of the upper digestive tract in all patients, its superficial inflammation was determined only in 29 preparations, diffuse inflammation (on all layers of the mucous membrane) - in 129 biopsies (82%), the active stage of inflammation - in 102 (65 %), atrophy - in 6, erosion - in 1 case. The obtained data reveal significant morphological changes in the mucous membrane of the digestive tract in conditions of reflux disease. Under conditions of reflux disease, the unchanged mucous membrane of the esophagus was not observed, superficial inflammatory changes in CO were noted in 6 biopsy specimens, diffuse (to the entire depth of the mucous membrane) - also in 6, in one case erosion was detected. After surgery, unchanged CO was noted in 3 patients, superficial inflammatory changes in 9, diffuse changes were not detected (p = 0.028). In the fundal section of the stomach, inflammatory changes in CR for the entire depth were detected in all 12 biopsy specimens; in 6, inflammation was in the active stage. After surgery, the inflammatory changes in CO for the entire depth remained in 5 biopsies, the superficial lesion was also determined in 7 biopsies, which is due to the decrease in inflammatory changes in CO for the entire depth (p = 0.018).
In the antrum of the stomach in the conditions of the Republic of Belarus, in all 12 biopsy specimens, inflammatory changes of CO were revealed to the full depth, in 3 cases it was in the active stage, in 2, atrophic inflammation was determined. After the operation, the inflammatory changes in CO for the entire depth were determined only in 8 cases (p> 0.05) with moderate activity of the process in 2 cases (p> 0.05), superficial gastritis - in 2 cases, atrophic - also in 2. In 12 - PC, in all 12 cases, chronic inflammation of CO took over its entire thickness, after the operation - only in 6 (p = 0.028). Summarizing the data obtained from the study of 48 biopsy specimens (12 out of the mucous membranes of the esophagus, fundus of the stomach, antrum, 12 - PC) taken before the operation, superficial (initial) inflammation was observed in 6 cases, but at the same time diffuse inflammation (for all layers of the mucous membrane) were noted in 42 biopsy specimens, in 9 cases there was an active stage of inflammation, and in 2 cases mucosal changes were atrophic.
Table 1: The condition of the mucous membrane of the esophagus, stomach and duodenum in the same 12 patients with RB before and after surgery.
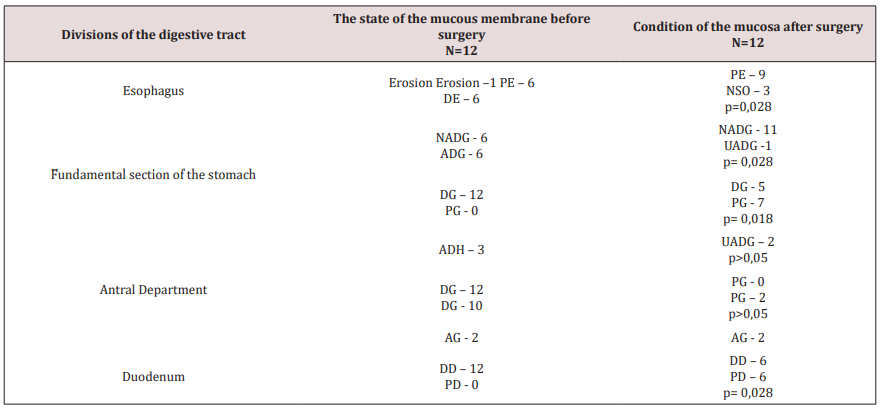
Note: NSO - unchanged mucosa, DE - diffuse esophagitis, PG - superficial gastritis, ADH - active diffuse gastritis, UDH - moderately active diffuse gastritis, DG - diffuse gastritis, AG - atrophic gastritis, DD - diffuse duodenitis, PD - superficial duodenitis NADH - inactive diffuse gastritis.
After bauginoplasty in combination with duodenojejunostomy in 48 biopsies taken from the same departments, unchanged mucosa was found in 3 biopsies (only in the esophagus), superficial inflammation was observed in 23 studies by reducing diffuse inflammation (p = 0.005), the active stage of inflammation also decreased to 3 observations (p = 0.028), mucosal atrophy remained at the same level - in 2 (Table 1). Thus, BP in combination with DES significantly improves the morphological characteristics of the mucous membranes of the esophagus, stomach, and 12 - PC, reducing the activity of the chronic process, reducing the depth of the lesion.
The morphometric parameters of CO also confirm the reduction of inflammation, the normalization of the characteristics of CO cells, which, according to our data, is preparing the structural basis for the normalization of their function (Tables 2 & 3). During the initial treatment of patients in biopsy specimens taken at endoscopy, the morphological picture of esophagitis was determined, with the finding of intraepithelial hemorrhages, papilla elongation, increased infiltration of the lamina propria, manifestations of stasis, and the presence of vasectasias. The mucosa of the cardial department of the stomach in the biopsy was not determined in all patients, the mucous membrane of the intermediary zone of the stomach was found in a significant number of observations, which is due to technical difficulties due to topographical features. In isolated cases, the mucous membrane of the cardia was characterized by manifestations of disregeneration with the presence of foveolar hyperplasia of the superficial-fossa epithelium or cystic-altered fossa and individual glands. In the surface section of the mucous membrane were detected vasectomies, everywhere - manifestations of stasis. In half of the cases, active diffuse gastritis of the intermediary zone of the stomach was detected.
Table 2: Morphometric indices of the gastric mucosa in diffuse gastritis in the same patients with RB before and after surgery.
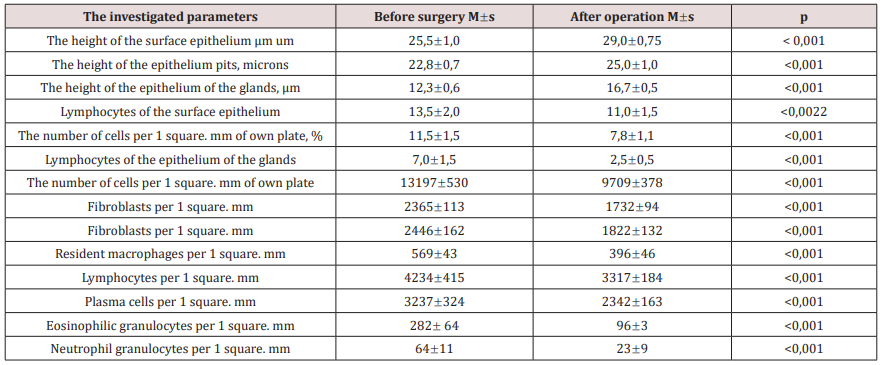
Table 3: Morphometric indices of the mucous membrane of the antrum of the stomach in diffuse gastritis in the same patients with RB before and after surgery.

In the body of the stomach, predominantly diffuse gastritis was determined, in a third of patients in the thickness of the mucous membrane there were accumulations of lymphocytes by the type of lymphoid nodule, or lymphoid nodules. Cell density of its own plate was most pronounced. The height of the superficial-patchy epithelium in all cases was significantly lower than the normal values. The lymphoplasmacytic infiltrate was unevenly distributed, there was an increased content of lymphocytes, plasma cells, eosinophilic granulocytes. The increased content of interepithelial eosinophilic granulocytes along with the presence of single neutrophilic granulocytes, the quantitative growth in the lamina propria of the mucous membrane of those and others testified to the activity of gastritis of varying degrees. In chronic inactive gastritis, a sharp increase in the number of plasma cells in the lamina propria of the mucosa was determined (3237324). Active diffuse antrum gastritis was diagnosed in 21 patients, while in the body of the stomach - in three cases.
The synthetic function of the superficial-patchy epithelium, determined by the height of the epithelial cells, as well as of the cells of the antral glands, was characterized by insufficient mucus formation of the entire epithelial layer (the height of the surface monocytes is 25.2 мкм1.3 microns, patchy -23.41.4 microns, while in normal those and others - 30 microns). The greatest morphological changes are characteristic of Helicobacter antrumgastritis, detected by direct microscopy. At the same time, a significant number of intraepithelial lymphocytes was determined in the surface-patchy epithelium, eosinophilic and neutrophilic granulocytes were always detected. Significantly, the presence of the listed intraepithelial cells is also characteristic of intercalated glands. Cell density in the lamina propria of the mucous membrane is sharply increased (14234–675) due to lymphocytes, plasma cells, with the presence of polymorphonuclear leukocytes, which was decisive in assessing the degree of activity of gastritis (the number of neutrophil granulocytes is 265 35, eosinophilic 312 53). After surgery in the mucous membrane of the esophagus, an increase in the resistance of the epithelial layer is determined, manifested in the absence of loosening of the epithelium and reactive hyperplasia of the basal cells (8 out of 12), absence of hemorrhages and shortening of the length of the subepithelial papillae (9 out of 12), which was noted before the operation. Four patients showed signs of inflammation in the lamina propria of the esophageal mucosa.
After the operation, the morphological picture of inactive diffuse gastritis or superficial gastritis was determined in the gastric mucosa. The severity of inflammation, determined by the cellular density of the infiltrate, was less pronounced. The density of infiltration was reduced by plasma cells. Cells characterizing the activity of inflammation, neutrophilic and eosinophilic granulocytes, were determined in a single quantity. Attention is paid to the normalization of the microcirculatory bed in the deep part of the mucous membrane. This led to an improvement in the epithelial layer, which resulted in an increase in the height of superficial-fossil epithelial cells. Morphological changes in the mucous membrane of the antrum of the stomach are like changes in the mucous membrane of the body of the stomach. However, there are a number of distinctive features that relate to the general histoarchitecture of the mucous membrane. Thus, for the antrum, a characteristic feature is the greater depth of the gastric dimples, the maximum degree of expression of the cellular density of the infiltrate. After surgery in patients, the superficial and hollow epithelium was characterized by clarity of cell boundaries, the presence of a contouring basement membrane. Quantitative indicators of cell density are significantly lower compared to the preoperative period, the predominant cell populations are lymphocytes, plasma cells and macrophages are determined, as single cells were detected eosinophilic and neutrophilic granulocytes. While maintaining lymphoplasmacytic infiltration with the presence of single eosinophilic and neutrophilic granulocytes in the deep part of the mucous membrane, attention is paid to reducing the height of the granulocytes.
In conditions of reflux - gastritis, a decrease in the height of the superficial and to a lesser extent of fossa epithelium is determined, the depth of the gastric dimples increases, their configuration changes, the layer of glands is narrowed. In the duodenal mucosa, before surgery, the morphological picture of diffuse duodenitis was determined in most patients in 32 (86%) of 37 patients, after surgery - in half of the cases - in 6 (50%) of 12. Conducted morphometric studies of the mucous membrane of 12 PCs showed that the cell density of the infiltrate in the villus and crypts own plate decreases, the number of infiltrate cells in the sections of the mucosa is equalized (8955–419 spores and 11689516- intercryptal). The regeneration of epithelial cells improves and the tendency for the postmitotic differentiation of goblet exocrinocytes and apical granular cells to be restored.
Comparative morphometric analysis showed that in patients with RB in the long-term period after surgery, there is a decrease in cell density of the infiltrate in the lamina propria of the mucous membrane with alignment in the duodenum (p <0.001), which creates more favorable conditions for the differentiation of the epithelium and increase its functional opportunities. The morphological expression of this is a statistically significant increase in the height of epithelial cells in the superficial-patchy zone of 12 PCs and granulocytes (p <0.001), an increase in the number of goblet cells in the epithelial layer of the duodenal villi (p <0.001) and apical granular cells in crypts (p <0.001).
In the epithelial layer of all types of epithelium, the content of intraepithelial lymphocytes decreased (p <0.001), which is also evidence of less pronounced inflammatory changes. Despite the fact that lympho-plasmocytic infiltration was preserved in its own plate, its severity was regarded as mild or moderate. The distinct decrease observed in parallel with the infiltration of eosinophilic (p <0.001) and neutrophilic (p <0.001) granulocytes, indicates an improvement in the microcirculation system in the 12-PC mucosa, which helps restore the metabolic functions of the muscle plate. Thus, in conditions of reflux disease, chronic inflammation is formed in the mucous membrane of the digestive tract, for the elimination of which the most adequate method is bauhinoplasty combined with duodenojejunostomy. Bauginoplasty in combination with duodeno-jejunostomy significantly improves the morphological characteristics of the mucous membranes of the esophagus, stomach and 12-pc, small and large intestine, reducing the activity of the chronic process, reducing the depth of the lesion. Morphometric indicators of the mucous membrane also confirm the reduction of inflammation, the normalization of the characteristics of cells of the mucous membrane, which prepares the structural basis for the normalization of their function.
References
- Vitebsky YaD (1976) Chronic violations of duodenal permeability and peptic ulcer of the stomach and duodenum. In: Ya D Vitebsky, Chelyabinsk: Yuzhnouralsk Prince Publishing house, pp. 190.
- Pixin IN (2002) Surgery of peptic ulcer. In: IN Pixin, VI Davytkin // Surgery of peptic ulcer: Prince. 3. - series: Difficult questions of practical surgery. Saransk: Publishing House Mordov, pp. 272
- Nesterenko YuA (1990) Chronic duodenal obstruction. M. Medicine, pp. 238.
- Samson EI (1975) Current issues of gastroenterology. Medicine, pp. 210-217.
- Bulgakov GA (1977) Lesions of the hepatobiliary-pancreatic system in secondary duodenostasis. In: GA Bulgakov, p. 9 -11.
- Bertolotti M (1981) Interdigestive gastroduodenal motiliti in duodenal ulser: the role of gastrik acid hypersecretion. Amer J Gastroenterol 84(1): 17-21.
- Mihaskiv IN (1980) The role of reflux of duodenal contents in the genesis of gastric stump cancer after stomach resection. Surgery 2: 44 - 51.
- V Poxon (1986) Insidens of bile reflux in gastric ulcer and after partial gastrectomy. Brit J Surg 73(4): 295 - 297.
- Vitebsky Ya D (1986) Diagnosis of secondary biliary reflux esophagitis.
- Pakhomova GV (2001) Prediction of vagotomy results. Surgery 2: 52-55.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...