Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1652
Research Article(ISSN: 2641-1652) 
Hispanic Ethnicity is Associated with Milder Disease Severity in Crohn’s Disease but not Ulcerative Colitis Volume 2 - Issue 2
Christie Choi, Amit Singal, Kunjali Padhya, Avegail Flores, Ezra Burstein and Tasneem Ahmed*
- Department of Internal Medicine -Division of Digestive& Liver Diseases, Dallas, TX, USA
Received:March 08, 2019; Published: March 19, 2019
*Corresponding author:Tasneem Ahmed, Department of Internal Medicine -Division of Digestive& Liver Diseases, Dallas, TX, USA
DOI: 10.32474/CTGH.2019.02.000132
Abstract
Background: The incidence of inflammatory bowel disease (IBD) is rising among minority patients; however, few studies have examined racial/ethnic disparities in epidemiology, disease severity, and treatment course.
Aim: To characterize differences in IBD disease severity and outcomes among IBD patients from minority communities.
Methods: A cohort of adult patients with IBD was followed from January 2007- December 2012 in a large urban safety-net hospital. Fisher exact and Mann-Whitney rank sum tests were used to compare disease phenotype, severity, need for anti-TNF therapy, receipt of IBD-related surgery, and hospitalizations.
Results: We identified 291 adult IBD patients; 148 with Crohn’s Disease (CD), 143 with ulcerative colitis (UC). Our cohort was racially diverse with 32% Caucasian, 37% Black, 28% Hispanic, and 2% Asian. 54% were male and the median age of the cohort was 44 years. Hispanic patients had a more benign disease course characterized by less IBD-related surgeries (mean 0.4 vs. 1.1, p=0.001), less hospitalizations (mean 2.1 vs. 2.9, p=0.04), and lower need for anti-TNF therapy (27% vs. 39%, p=0.05) when compared to non-Hispanic patients. On subgroup analysis, these differences were noted particularly among those with CD but not UC. Hispanic UC patients had a similar number of IBD-related surgeries (p=0.16) and hospitalizations (p=0.62), whereas Hispanic CD patients had less IBD-related surgeries (mean 0.8 vs. 1.8, p=0.01), less hospitalizations (mean 2.4 vs. 3.8, p=0.05), and lower need for anti-TNF (38% vs. 57%, p=0.09).
Conclusion: Hispanic ethnicity is associated with lower disease severity in CD but not associated with disease severity in UC.
Keywords:Inflammatory Bowel Disease; Crohn’s Disease; Ulcerative Colitis; Race; Ethnicity; Disparities
Introduction
Crohn’s disease (CD) and Ulcerative colitis (UC) are chronic inflammatory disorders of the gastrointestinal tract, collectively termed IBD. In the United States, it is estimated that 1 million people are affected by IBD with studies demonstrating a rise in incidence within the past two decades, particularly for CD among non-Caucasian patients. Despite the increasing numbers of Hispanics, African-Americans (AAs), and Asians being identified with IBD, few studies have examined racial/ethnic disparities in epidemiology, disease severity, and treatment course. Existing reports paint a conflicting picture regarding disease phenotype, severity, and use of immunosuppressive therapy in AAs with IBD. Results have ranged from demonstrating no significant differences in disease course, severity, or extra-intestinal manifestations (EIMs) [1-3] to studies showing AAs having a less severe disease course characterized by lower need for steroid treatment [4,5], immunomodulator therapy (IMMs) [6], or to undergo colectomy in UC [7] compared to Caucasians. A more recent study demonstrated AAs with CD had a higher rate of IBD-related arthralgias and surgeries, but less ileal involvement, without further differences in extraintestinal manifestations (EIMs) or disease locations compared to Caucasian CD patients. This same study found AA UC patients were older at diagnosis and had more EIMs, but without any differences in disease extent or rate of IBD-related surgeries compared to Caucasian UC patients. Furthermore, in this cohort, race did not play a role in medication usage for CD and UC patients [8]. Hispanics, accounting for 17.1% of the US population according to the 2013 U.S. Census Bureau, are increasingly being identified with IBD [9].
Therefore, it is important to recognize epidemiologic differences in order to optimize treatment for these patients. Similar to what was seen in AAs, studies identifying phenotypic variations, treatment preferences, and disease outcomes in Hispanics have been conflicting [10-13]. One group found that Hispanics were diagnosed at a significantly older age than Caucasians and had a lower number of bowel resections per patient. Additionally, UC was found to be more common than CD in Hispanic IBD patients [14]. On the other hand, another group found that prolonged steroid exposure was more common among Hispanics with UC, and these patients had more UC-related surgeries and hospitalizations, although these differences were not significant in multivariate analysis [15]. Altogether, the existing data leave open several unanswered questions regarding IBD disease course and management among different ethnicities. The large urban safetynet health care system of Parkland Hospital serving 2.4 million in the Dallas County provided an ideal setting to investigate these questions given its widely racially diverse population. Our intent was to determine if ethnicity is a clinically significant variable influencing disease severity, need for IMM or anti-TNF therapy, surgery, and hospitalization in this ethnically diverse cohort of IBD patients.
Materials and Methods
Study Setting and Population
We performed a retrospective cohort study of adult IBD patients (> 18 years old) followed at Parkland Health and Hospital System, the safety-net health system for Dallas County, between January 2007 and December 2012. Given its integrated structure and function as a safety-net institution, patients admitted to Parkland Hospital often receive their continuity care through the Parkland Health System clinics. Parkland utilizes a single comprehensive electronic medical record (EMR), including laboratory and radiology results, for all inpatient and outpatient care. Patients were identified using ICD-9 codes for CD and UC as well as a prospectively maintained database of patients with IBD seen in the Gastroenterology clinic. One author (C.C) reviewed all cases to confirm that patients truly had a confirmed diagnosis of IBD. Patients were excluded if 1) they had an indeterminate or alternate etiology of colitis (infectious, ischemic, diverticular-associated, etc.), 2) received steroids, IMM, or anti-TNF therapies for conditions other than IBD, 3) received anti-TNF therapy prior to establishing care at Parkland, 4) were lost to follow up within 6 months of IBD diagnosis, or 5) had insufficient data for assessment of our primary outcome. This study was approved by the Institutional Review Board at the University of Texas Southwestern Medical Center and Parkland Memorial Hospital.
Data Collection
Patient demographics, clinical history, laboratory data, and endoscopic data were obtained through review of EMR records. One investigator (C.C.) extracted information using standardized forms, with another investigator (T.A.) available for questions. Age, gender, race/ethnicity, and smoking history (ever vs. never), and family history of IBD were recorded. Dates of IBD diagnosis, any IBD-related surgeries, and IBD-related hospitalizations were documented. IBD related surgeries were defined as any bowel resection or intervention for peri-anal disease (i.e. incision and drainages of abscess, seton placement, fistulotomy, etc) that required time in the operating room. IBD-related hospitalizations were defined as any inpatient stay exceeding 24 hours for which the primary reason of admission was related to IBD or IBDrelated treatment. We categorized disease location as upper GI vs ileal vs. ileocolonic vs. colonic vs. perianal for patients with CD, whereas disease location was classified as proctitis vs. left-sided vs. pancolitis for those with UC. Patients with CD were classified as having an inflammatory vs. stricturing vs. fistulizing disease phenotype, whereas UC patients were categorized as having mild vs. moderate vs. severe disease based on their index colonoscopy. We also recorded any extra-intestinal manifestations and/or other IBD-related complications for each patient. Treatment regimens of interest included any use of steroids, 5-ASA agents, IMMs, and anti- TNF agents.
Statistical Analysis
Our primary outcome of interest was ethnicity as a clinically significant variable in disease outcomes. In univariate analysis, Fisher exact and Mann Whitney rank-sum tests were performed to identify factors associated with IBD-related surgeries and hospitalizations. IBD-related surgeries and hospitalizations were both categorized as none vs. ≥1 during the follow-up period. The multivariate logistic regression model included variables of interest (i.e., race/ethnicity), those of a priori clinical importance (i.e., anti-TNF therapy), and factors significant on univariate analysis. Statistical significance was defined as p< 0.05 for univariate and multivariate analyses. All data analysis was performed using Stata 11 (Stata Corp, College Station, TX).
Results
Patient Demographics
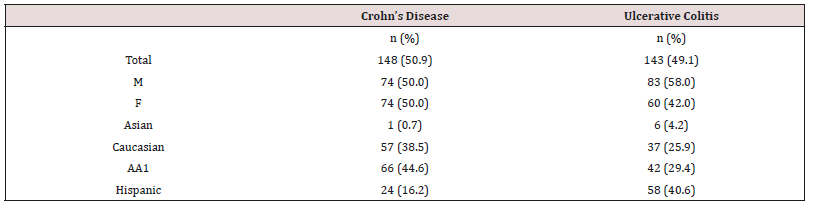
We initially identified 351 patients with a diagnosis of IBD seen at Parkland Health and Hospital System between January 2007 and December 2012. After further review, we excluded 25 patients with alternate etiologies for their colitis and 2 patients with indeterminate colitis, leaving 324 with a confirmed diagnosis of IBD. An additional 33 patients were excluded because of (i) IMM therapy received prior to establishing care at Parkland or IMM given for another disease process (n=6), (ii) being lost to follow up within 6 months of IBD diagnosis (n=21), (iii) having had prior colonic surgeries (n=2), or, (iv) having insufficient data for assessment of our primary outcome (n=4). Of the final 291 patients remaining in the cohort,148 had CD and 143 had UC (Table 1). Overall, 54% were male, and the median age of patients was 44 years. Our cohort was racially diverse with 32% Caucasians, 37% Blacks, 28% Hispanics, and 2% Asians. Due to small sample size, Asians were not included in ethnic comparisons but were included in all “non-Hispanic” vs. “Hispanic” group comparisons.
Table 1: 291 adult IBD patients were identified, 148 with Crohn’s Disease (CD) and 143 with Ulcerative Colitis (UC). 1African- American.
Racial/Ethnic Differences in Disease Presentation
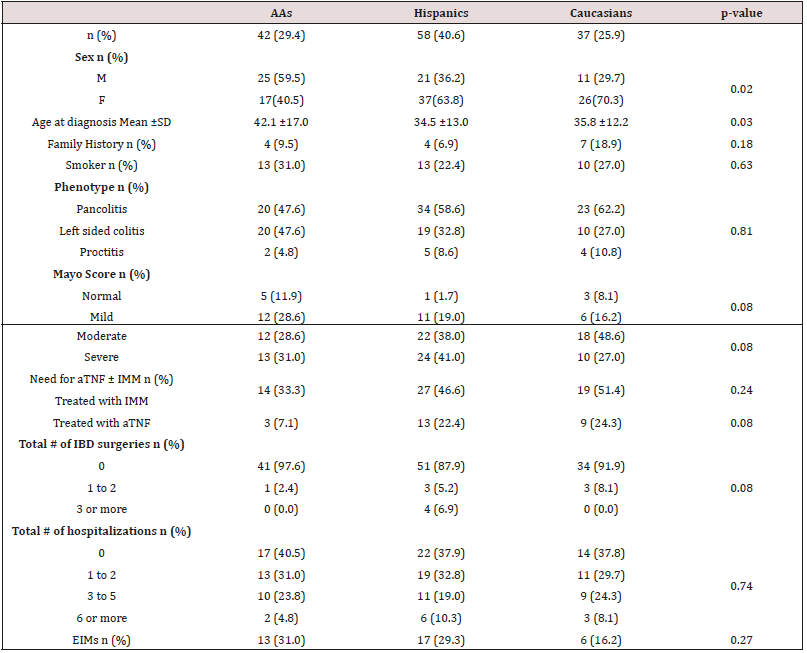
We found significant racial/ethnic differences in age at IBD presentation (Table 2). Hispanic patients were diagnosed at an older age (mean 36.8) compared to AAs and Caucasians (32.5 and 31.9, respectively). On subgroup analysis, we found that this difference was largely driven by the age of diagnosis among CD patients (Table 3), with Hispanics being diagnosed at a significantly later age (mean 42.1) compared to AAs (mean 26.4) or Caucasians (mean 29.4), p=< 0.001. On the other hand, among UC patients (Table 4), Hispanics were diagnosed at a somewhat earlier age (mean 34.5), compared to Caucasians (mean 35.8) and particularly AAs (mean 42.1), p=0.03. Overall, we found significant differences in having ever been a smoker (Table 2), which on subgroup analysis was found to be due to a lower rate of ever smoking among Hispanics compared to non-Hispanics for the entire cohort (p=0.003), which was also observed in subgroup comparison of Hispanics vs. non- Hispanics within CD, (p=0.05). In addition, Caucasians were more likely to have a positive family history of IBD (20.2%) compared to AAs (8.3%) or Hispanics (7.3%, Table 2). We failed to find significant differences in the distribution of disease phenotypes among the three ethnic groups. Within CD patients (Table 3), there were no significant differences in disease phenotype (p=0.16) or location (p=0.96). Similarly, there were no significant differences in disease phenotype (p=0.81) or Mayo score (p=0.08) within UC patients (Table 4). Finally, we found no significant differences in rates of EIMs (p=0.50) between AAs, Hispanics, and Caucasians.
Table 2: Characteristics of all IBD patients by ethnicity (African-Americans, Hispanics, and Caucasians). Asians are not presented in the table due to small sample size but included in the total count & analysis of “Non-Hispanics” comparisons to “Hispanics.”
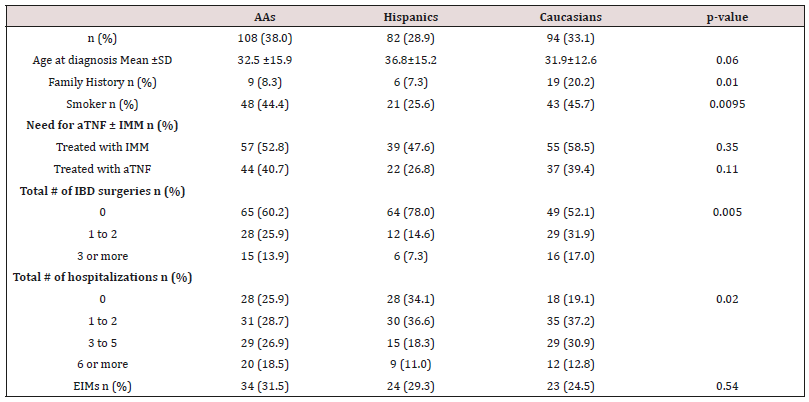
Table 3: Comparisons among Crohn’s Disease patients by ethnicity. Asians are not presented in the table due to small sample size but included in the total count & analysis of “Non-Hispanics” comparisons to “Hispanics.”
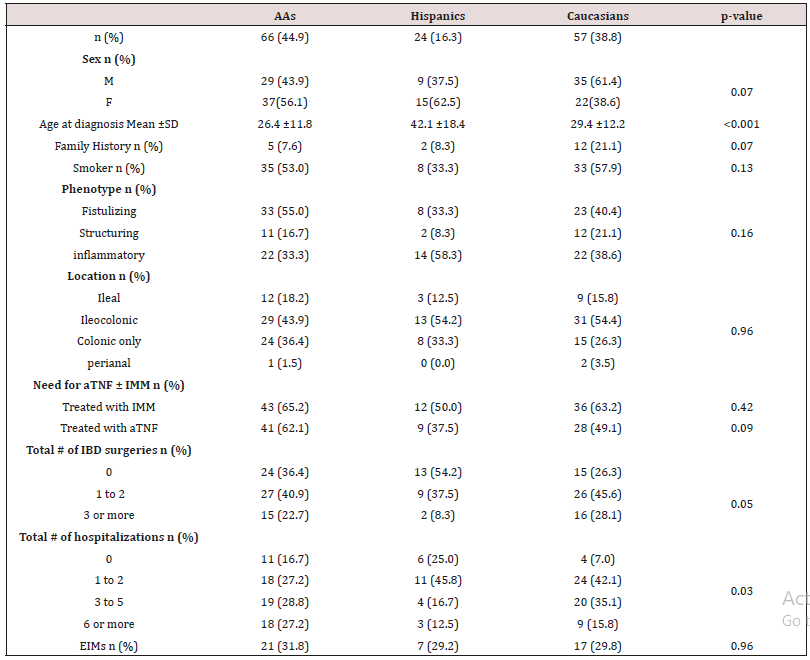
Table 4: Comparisons among Ulcerative Colitis patients by ethnicity. Asians are not presented in the table due to small sample size but included in the total count & analysis of “Non-Hispanics” comparisons to “Hispanics.”
Racial/Ethnic Differences in Disease Severity And IBDRelated Outcomes
Considering IBD-related surgeries and hospitalizations, Hispanic patients had a more benign disease course (Table 2). Compared to non-Hispanics, they had significantly less IBD-related surgeries (mean 0.4 vs. 1.09, p=0.0008) and total hospitalizations (mean 2.1 vs. 2.9, p=0.04). On subgroup analysis, these differences were primarily noted among those with CD and not among those with UC. Compared to non-Hispanics, Hispanic UC patients had a similar number of IBD-related surgeries (p=0.16) and hospitalizations (p=0.62), whereas Hispanic CD patients had lower rates of both IBD-related surgeries (mean 0.8 vs. 1.8, p=0.01) and total hospitalizations (mean 2.4 vs. 3.8, p=0.05). Among all IBD patients, Hispanics were also significantly less likely to require anti- TNF therapy, (39.2% vs. 26.8%, p=0.05). On subgroup analysis, this difference was more pronounced in those with CD; however, this difference failed to reach statistical significance (56.9% vs. 37.5%, p=0.09).In addition, we found a trend for greater need for anti-TNF therapy among AAs compared to Caucasians (62.1% vs. 49.1%) in the CD population, but this did not reach statistical significance (Table 3).
Racial/Ethnic Differences on Multivariate Analysis
Hispanic ethnicity was associated with significantly fewer IBDrelated surgeries as mentioned above. However, in multivariate analysis upon adjusting for age at diagnosis, tobacco use, and need for anti-TNF therapy, Hispanic ethnicity was no longer significantly associated with total number of IBD-related surgeries (p=0.09) or hospitalizations (p=0.56) among CD patients. Adjusting for those same variables, Hispanic ethnicity was also not a significant factor in UC.
Discussion
Though current literature remains conflicting, ethnicity does seem to play a clinically significant role in disease activity.
Significant strides are being made in the field of genetics and IBD, the gut microbiome and changes in this among immigrants (especially Hispanic and Asians) which may help to shed more light on IBD in different ethnicities [16-18]. Moreover, cultural differences, socioeconomic factors, and racial disparities in access to health care [19] must be examined carefully to see what role they play in IBD care. In our study, we found that overall Hispanics had less severe disease and were treated with less anti-TNF therapy compared to non-Hispanics (p=0.05). On subgroup analysis with CD patients alone, Hispanic patients appear to have less severe disease than non-Hispanics, with diagnosis at later ages, lower rates of IBD related surgeries, and IBD related hospitalizations. Conversely, Hispanic ethnicity did not appear to play a role in UC with no differences found in treatment, hospitalizations, or surgeries. This is in direct contrast to findings by Li et al who found Hispanics to have a more aggressive disease compared to AAs, Caucasians, and Asians in an exclusively UC population [15]. However, our findings are somewhat similar to Damas et al who found Hispanics to be treated with fewer therapies [20]. From our own experience, we hypothesized that AA IBD patients would have a more severe disease course compared to their Caucasian and Hispanic IBD counterparts. Interestingly, no significant differences, outside of age, were found in comparisons made with AA patients compared to the other ethnicities. Our findings support those found in prior studies [1,2,5,8].
With respect to age of onset, AAs were diagnosed later than Caucasians in UC but not in CD. This finding is in contrast to prior studies [8,21]. Our study has several strengths. First, it is comprised of a highly ethnically diverse cohort from one of the largest urban safety net hospitals in the country. Second, our patient population has equal access to the Parkland Health Plus program for Dallas County residents reflecting relatively uniform access to care for IBD patients. These patients receive care from the same set of gastroenterology faculty thus reducing potential confounding from site-specific factors and disparities in treatment access. The inclusion of all IBD patients seen within one health care system may reduce selection bias and improve generalizability in our findings. Lastly, we utilize a step-up approach to biologic therapy in patients with moderate IBD. This then limits use of anti-TNF therapy to those who have failed IMMs thus categorizing this subgroup of IBD patients as those with severe disease. This stepup approach to biologic therapy also eliminates any variability in practitioners’ perspective and bias in this setting. There are a number of limitations to this study that are important to mention. The retrospective nature of our study design did not allow for assessment of treatment response among the ethnicities. However, this is not dissimilar to most studies to date, which have assessed use of anti-TNF and IMM therapy rather than actual treatment response [1,4-6, 8,10,13-15,20-23]. The clinical practice does not routinely utilize disease activity indices as part of clinical care, and therefore these were not available in our retrospective analysis.
Additionally, using biologic therapy primarily in those who have failed IMM therapy does not represent the most common practices among IBD experts. Moreover, the use of anti-TNF therapy as also a marker of disease severity may not be entirely accurate and confound other variables. The modest sample size of Asians as well as short recruitment period of five years may make it difficult to adequately compare the different ethnicities as well as assess disease severity and complications and may explain the lack of findings upon extrapolating to multivariate analyses. Another notable point is that our foreign-born Hispanic patient population is largely from Mexico which is different from the largely Cuban foreign-born Hispanic population studied by Damas and colleagues. Altogether, this study contributes additional evidence that ethnic differences can influence the phenotypic expression and treatment needs of IBD. Future studies will be required to elucidate whether this is driven by underlying genetic differences or environmental influences that are disproportionately segregated among these groups.
References
- Moore L (2012) Comparison of the natural history of ulcerative colitis in African Americans and non-Hispanic Caucasians: a historical cohort study. Inflamm Bowel Dis 18(4): 743-749.
- Straus WL (2000) Crohn’s disease: does race matter? The Mid-Atlantic Crohn’s Disease Study Group. Am J Gastroenterol 95(2): 479-483.
- Mahid SS (2008) Inflammatory bowel disease and African Americans: a systematic review. Inflamm Bowel Dis 14(7): 960-967.
- Flasar MH (2008) Disparities in the use of immunomodulators and biologics for the treatment of inflammatory bowel disease: a retrospective cohort study. Inflamm Bowel Dis 14(1): 13-19.
- Flasar MH (2008) Racial differences in disease extent and severity in patients with ulcerative colitis: a retrospective cohort study. Dig Dis Sci 53(10): 2754-2760.
- Nguyen GC (2010) Racial disparities in utilization of specialist care and medications in inflammatory bowel disease. Am J Gastroenterol 105(10): 2202-2208.
- Nguyen GC (2006) Racial and geographic variations in colectomy rates among hospitalized ulcerative colitis patients. Clin Gastroenterol Hepatol 4(12): 1507-1513.
- Sofia MA (2014) Clinical presentation and disease course of inflammatory bowel disease differs by race in a large tertiary care hospital. Dig Dis Sci 59(9): 2228-2235.
- (2014) US Census Bureau. United States Census Bureau - Foreign Born.
- Basu D (2005) Impact of race and ethnicity on inflammatory bowel disease. Am J Gastroenterol 100(10): 2254-2261.
- Nguyen GC (2006) Inflammatory bowel disease characteristics among African Americans, Hispanics, and non-Hispanic Whites: characterization of a large North American cohort. Am J Gastroenterol 101(5): 1012-1023.
- Malaty HM, JK Hou, S Thirumurthi (2010) Epidemiology of inflammatory bowel disease among an indigent multi-ethnic population in the United States. Clin Exp Gastroenterol 3: 165-170.
- Yarur AJ (2014) The impact of Hispanic ethnicity and race on postsurgical complications in patients with inflammatory bowel disease. Dig Dis Sci 59(1): 126-134.
- Hou J (2011) Inflammatory bowel disease characteristics and treatment in Hispanics and Caucasians. Dig Dis Sci 56(5): 1476-1481.
- Li D (2014) Racial and ethnic differences in health care utilization and outcomes among ulcerative colitis patients in an integrated health-care organization. Dig Dis Sci 59(2): 287-294.
- Kugathasan S (2005) Comparative phenotypic and CARD15 mutational analysis among African American, Hispanic, and White children with Crohn’s disease. Inflamm Bowel Dis 11(7): 631-638.
- Dassopoulos, T (2010) NOD2 mutations and anti-Saccharomyces cerevisiae antibodies are risk factors for Crohn’s disease in African Americans. Am J Gastroenterol 105(2): 378-386.
- Wang MH (2012) Contribution of higher risk genes and European admixture to Crohn’s disease in African Americans. Inflamm Bowel Dis 18(12): 2277-2287.
- Jackson JF, A Kornbluth (2007) Do black and Hispanic Americans with inflammatory bowel disease (IBD) receive inferior care compared with white Americans? Uneasy questions and speculations. Am J Gastroenterol 102(7): 1343-1349.
- Damas OM (2013) Phenotypic manifestations of inflammatory bowel disease differ between Hispanics and non-Hispanic whites: results of a large cohort study. Am J Gastroenterol 108(2): 231-239.
- White JM (2008) Inflammatory bowel disease in African American children compared with other racial/ethnic groups in a multicenter registry. Clin Gastroenterol Hepatol 6(12): 1361-1369.
- Mukewar S (2013) Ethnicity and the risk of development of Crohn’s disease of the ileal pouch. J Crohns Colitis 7(5): 178-185.
- Sewell JL, JM Inadomi and HF Yee (2010) Race and inflammatory bowel disease in an urban healthcare system. Dig Dis Sci 55(12): 3479-3487.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...