Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1652
Mini review(ISSN: 2641-1652) 
Gut Microbiome in Health and Disease Volume 2 - Issue 3
Jayme Sack2 and Hari Tunuguntla1*
- 1 Department of Surgery and Urology, Rutgers Robert Wood Johnson Medical School, USA
- 2 Robert Wood Johnson Place, Medical Education Building 588, USA
Received:May 08, 2019; Published: May 13, 2019
*Corresponding author:Hari Tunuguntla,Department of Surgery and Urology, Rutgers Robert Wood Johnson Medical School, USA
DOI: 10.32474/CTGH.2019.02.000137
Abstract
The Gut Microbiome is an integral component to the mental and physical wellbeing of humans. The symbiosis of various microbacteria in cohabitation with our organs is crucial for daily function. In this review article, we reference current literature to demonstrate how important the link between the feelings of our gut is with the rest of our body. We detail critical points of how the gut microbiome affects other systems. The role of maternal microbiome in fetal development diversifies gut flora and enhances defense against stress. The enteric nervous system is intertwined with brain signals and hormonal impulses, which effectively connects two independent systems. The neuropsychiatric involvement with the gut and modulation of psychological disorders can influence gut dysbiosis- a term we define as shifts away from “normal gut microbiota diversity.” Lastly, we conclude with solutions to impaired gut-brain axes. Healthier lifestyle decisions with diet, exercise, and meditation are critical to positive influence of the intestinal microbiota. We discuss one such practice, Shivyog, which chooses a whole-body approach to fighting stress, while increasing physical stamina. We hope to shed light on how improvement in gut flora allows the systems of the human body to function synchronously.
Keywords: Gut; Microbiome; Symbiosis; Dysbiosis; Shivyog
Abbreviations: CNS: Central Nervous System; ENS: Enteric Nervous System; FGIDs: Functional Gastrointestinal Disorders; IBD: Inflammatory Bowel Disease; IBS: Irritable Bowel Syndrome
Introduction
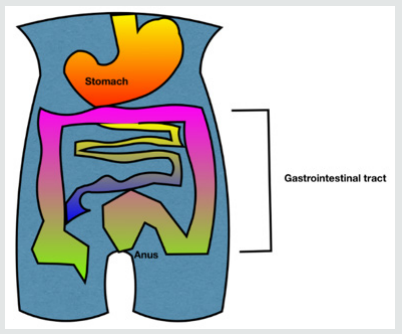
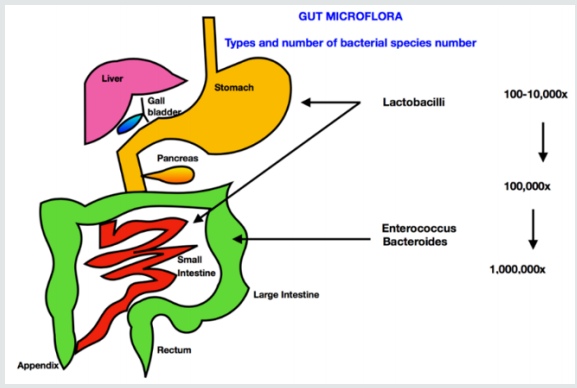
All of us are aware of a common metaphor, do not ignore your ‘gut feeling’ when making a decision. Now it is scientifically proven that our emotions are symbolically very much connected to the gut (i.e. the intestine). Lifestyle choices that mediate gut health, importantly, diet (i.e. reduction of excess sugar and refined carbohydrates) and pre and probiotic intake have been shown to be closely related to the well-functioning of our brain. All human beings have a microbiome, and the bacteria it is composed of, are as unique as our neural pathways. The human body is composed of more bacteria than cells. These trillions of bacteria are called the microbiome. They mostly reside in the gut, also referred to as the gut microbiota or gut microbiome and play multiple roles in our overall health. The gut is no longer seen as an entity that helps with our digestion. It is now believed to function as a key player in regulating inflammation and immunity. Their diversity help maintain health and homeostasis (internal milieu) (Figure 1,2).
Discussion
Human microbiome and intestinal flora
The human microbiome is composed of protozoa, archaea, eukaryotes, viruses and predominantly bacteria that live symbiotically on and within various sites of the human body. Examples of occupied habitats include our oral cavity, genital organs, respiratory tract, skin and gastrointestinal system [1]. The human microbiota is estimated to be 1013–1014 microbial cells, with around 1:1 microbial cells to human cells ratio. These numbers are derived from the total bacterial cells in the colon (3.8 x 1013 bacteria), the organ that harbors the densest number of microbes [2]. Gut microbiome is mostly composed of bacteria from three major phyla, namely Firmicutes, Bacteroides, and Actinobacteria [3]. Advances in sequencing technologies and subsequent largescale sequence based microbiome projects such as the Human Microbiome Project (HMP) consortium funded by The United States National Institutes of Health (NIH), as well as the Meta HIT (Metagenomics of the Human Intestinal Tract) consortium funded by the European Commission, have served as catalysts in nourishing research on the human microbiome.
Dysbiosis
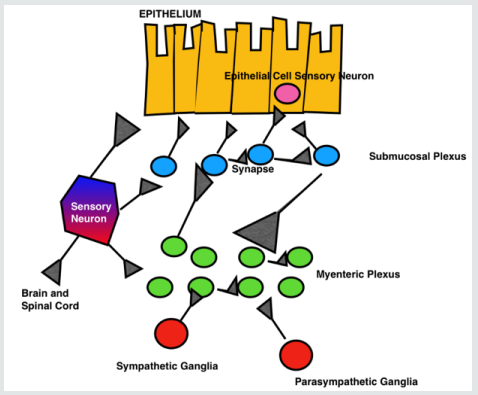
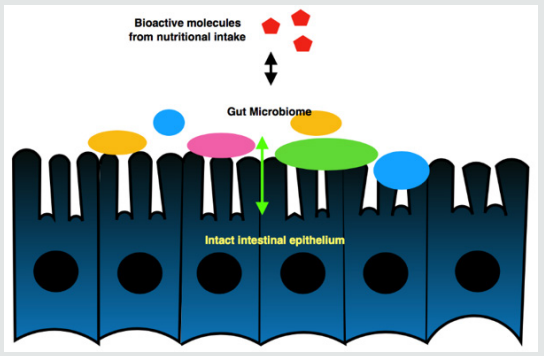
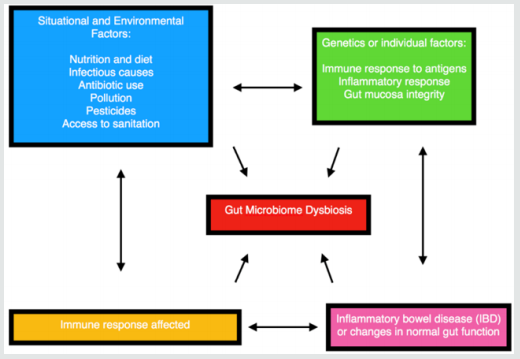
A shift away from so called normal gut microbiota diversity is called dysbiosis. Such an aberration and microbial imbalance contributes to disease per Dr. Avdhoot Shivanand. Gut microbiome is currently the focus of attention to understand autoimmune, brain, and gastrointestinal disorders (Figure 3-5).
Role of maternal microbiome in fetal development
The human fetus is extremely sensitive to any changes in the composition of maternal microbiota. A baby misses the opportunity to ingest mother’s bacteria (as it travels down the vaginal canal during normal
childbirth) if born via cesarean section. Compared to vaginally delivered babies, those born by cesarean section have to work to regain the same bacterial diversity of their microbiome [4]. Our microbiome remains a vulnerable entity throughout life to factors including, but not limited to stress, toxins, chemicals, and certain diets. Even regular exercise has been shown to result in a beneficial diversity of the microbiome [5].
The gut is our second brain
The gut microbiome plays a vital role to maintain our physical and psychological health via its own unique neural network called the ‘enteric nervous system’ (ENS) composed of over 100 million neurons found in the gut lining. The ENS is also called the ‘2nd brain’. There are structural and chemical similarities between the ENS and central nervous system (CNS). Embryologically, the ENS originates from the same tissues during fetal development as our central nervous system. The brain and gut closely communicate with each other through the mediation of intricate and highly coordinated neuronal, endocrine, and immune pathways involving electrical impulses, neurotransmitters and hormones. Our brain and gut are intimately connected and function as one integrated system, rather than 2 independent systems.
Emotions and gastrointestinal disorders
Psychosocial factors influence gut physiology (movement and contractions of the gut) and pathophysiology (inflammation, pain, increased/decreased motility and other bowel symptoms). Emotional and psychosocial factors potentially trigger symptoms in the gut and result in various functional gastrointestinal disorders (FGIDs) [6]. This group is composed of over 20 common chronic and difficult to treat disorders of the gastrointestinal tract.
Mental health and gut wellness
Modulation of stress and emotions is very important in the treatment of FGIDs. Better treatment outcomes could be achieved by incorporation of psychologically based approaches in conventional medical treatments.
A pilot study from the Harvard University affiliates, BensonHenry Institute for Mind Body Medicine at Massachusetts General Hospital and Beth Israel Deaconess Medical Center found that meditation could have a significant impact on those with irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD). The authors in this study reported reduced pain, improved symptom control, stress reduction, and the altered expression of genes that contribute to inflammation in 48 patients with IBS or IBD following a 9-week treatment arm that included meditation training [7].
Gut microbiome and neuro-psychiatric disorders
Poor gut health, pro-inflammatory states, and gut dysbiosis have been shown to result in neurological and neuropsychiatric disorders including Multiple Sclerosis, Autism, and Parkinson’s disease. Agerelated gut changes are also correlated with Alzheimer’s dementia.
Even depression is currently being considered as an inflammatory disorder mediated by poor gut health. Animal studies have shown that manipulating gut microbiota can result in behaviors related to anxiety and depression [8].
Conclusion
Gut-brain axis in the prevention and treatment of neuropsychiatric disorders
Maintenance of good gut health is of paramount importance in disease prevention and treatment, especially in neuropsychiatric disorders. Similarly, stress-reduction can help prevent and treat gastrointestinal disorders, reduce morbidity, impairment, and chronic dependency. Per Dr. Avdhoot Shivanand, our daily lifestyle choices (including healthy diet, physical exercises, Shivyog Sookshma Kriyas, Pran Kriyas, special Shivyog practices, Shivyog Sadhnas, sewa (service), sankirtan (e.g., Babaji Bhajan Singing) play a significant role in maintaining our overall wellness making us healthy, whole, and complete. Such a whole-body approach to health and wellness is crucial to improve longevity, well-being, and quality of life. Physical and mental health go hand-in-hand and help us to achieve the ability to lead a 200% life (per Dr. Avdhoot Shivanand, 100% worldly success and 100% spiritual success and upliftment).
References
- Lloyd-Price J, Abu-Ali G, Huttenhower C (2016) The Healthy Human Microbiome. Genome Med 8: 51
- Sender R, Fuchs S, Milo R (2016) Revised Estimates for the Number of Human and Bacteria Cells in the Body. PLoS Biol 14(8): e1002533.
- Tap J, Mondot S, Levenez F, Pelletier E, Caron C (2009) Towards the human intestinal microbiota phylogenetic core. Environ Microbiol 11(10): 2574-2584.
- Wampach L, Heintz-Buschart A, Fritz J, Ramiro-Garcia J (2018) Birth mode is associated with earliest strain-conferred gut microbiome functions and immunostimulatory potential. Nat Commun 9.
- Monda V, Villano I, Messina A, Valenzanpo A, Esposito T (2017) Exercise Modifies the Gut Microbiota with Positive Health Effects. Oxid Med Cell Longev p. 8.
- Jones M, Dilley J, Drossman D, Crowell M (2006) Brain-gut connections in functional GI disorders: anatomic and physiologic relationships. Neurogastroent Motil 18(2): 91-103.
- Kuo B, Bhasin M, Jacquart J (2015) Genomic and Clinical Effects Associated with a Relaxation Response Mind-Body Intervention in Patients with Irritable Bowel Syndrome and Inflammatory Bowel Disease. Plos one 10(4): e0123861.
- Smythies L, Smythies J (2014) Microbiota, the immune system, black moods and the brain- melancholia updated. Front Hum Neurosci 8: 720.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...