Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1652
Review Article(ISSN: 2641-1652) 
Evaluating the Therapeutic Role of Acupuncture in Gastrointestinal Disorders Volume 2 - Issue 3
Alexandra Sack1, Jayme Sack2 and Hari Tunuguntla3*
- 1 Departments from Teachers College, Columbia University, USA
- 2 Robert Wood Johnson Place, Medical Education Building, USA
- 3 Department of Surgery and Urology, Rutgers Robert Wood Johnson Medical School, USA
Received:June 17, 2019; Published: June 24, 2019
*Corresponding author:Hari Tunuguntla, Department of Surgery and Urology, Rutgers Robert Wood Johnson Medical School, USA
DOI: 10.32474/CTGH.2019.02.000140
Abstract
Gastrointestinal disorders currently plague millions of Americans and place an immense physical, emotional, and financial burden on society. The conventional medicine paradigm produces modest effects but are often accompanied with adverse side effects as well as increased healthcare utilization. Thus, the demand for alternative therapies is increasing. In the event that conventional medicine offers no satisfactory solution, research provides consistent and compelling evidence for the efficacy of acupuncture as a safe and cost-effective alternative approach to alleviating symptoms associated with digestive dysfunction. This review discusses the pathophysiology of common gastrointestinal disorders and the mechanisms underpinning the regulatory effect of acupuncture. Using principles of Traditional Chinese Medicine, we explain the therapeutic benefits of acupuncture and its’ ability to restore the body’s internal equilibrium and elicit a return to health. Lastly, we conclude with suggestions for optimizing long-term gastrointestinal health and disease prevention through a whole-body approach and healthy lifestyle modifications. We hope to unveil acupuncture as an effective alternative treatment for treating gastrointestinal disease.
Keywords: Acupuncture; Acupoints; QI; Gut; Yin; Yang; Eastern; Western
Abbreviations: TCM: Traditional Chinese Medicine; IBD: Inflammatory Bowel Disease; IBS: Irritable Bowel Syndrome; PCNA: Proliferating Cell Nuclear Antigen; GI: Gastrointestinal
Introduction
According to the National Institute of Health, more than 60 million Americans were diagnosed with digestive diseases in 2004 resulting in nearly $142 billion expended on direct and indirect costs [1]. Conventional pharmacological treatments have shown to produce modest effects but are costly, run the risk of adverse side effects, and often only provide temporary relief. Gastrointestinal (GI) disorders significantly impair health-related quality of life and work productivity as well as dramatically increase consumption of medical resources. These burdens warrant increasing attention towards the efficacy of alternative therapies for reducing the adverse symptoms that accompany GI diseases. Traditional Chinese Medicine (TCM) and conventional western medicine were long considered two distinct and independent medical models. While western medicine aims to treat disease symptoms using modern medications and procedures, TCM employs a more holistic approach that relies on natural remedies and therapies to restore balance in the body. Acupuncture has been used for thousands of years to treat a variety of illnesses, but it is today’s advanced technology that has allowed us to better understand the mechanisms underpinning the efficacy of this ancient healing method. Research provides promising scientific evidence that acupuncture is a safe and cost-effective approach to alleviating symptoms associated with digestive dysfunction. Acupuncture should not be visualized as competition to treatment modalities of western Medicine, but rather its clinical applications may better focus on conditions for which the conventional medicine has no satisfactory solution. This review will elucidate the current research surrounding the efficacy of acupuncture for treating various gastrointestinal disorders and its symptomatology.
Pathophysiology of Common Gastrointestinal Disorders
Researchers at the Ziamen University elucidate the possible mechanisms underlying common GI disorders which include a number of substances, notably proliferating cell nuclear antigen (PCNA), substance P, and neurotensin. These biomolecules play a vital role in regulating gastric motility, preserving the intestinal epithelial barrier, inhibiting intestinal inflammation, and protecting gastric mucosa. Acupuncture balances the levels of these biomarkers by either stimulating or suppressing the expression of PCNA, substance P, and neurotensin that encourages gastrointestinal mucosal epithelial growth, reduces gastric acid excretion and promotes healthy digestive motility [2]. The therapeutic effects of acupuncture may also result from its ability to regulate the neuroendrocrine immune system and activate the cholinergic antiinflammatory-dependent pathway, which aids in the preservation of intestinal barrier integrity and optimizes organ function [3].
Discussion
What is Acupuncture?
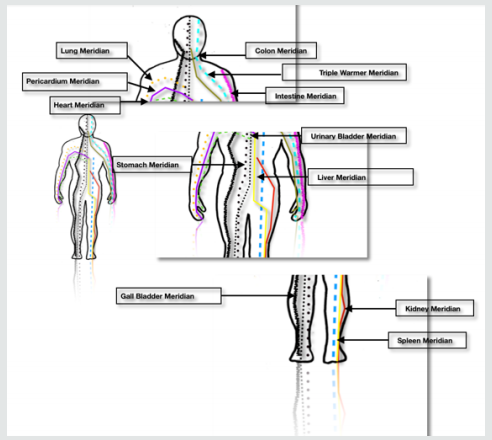
In TCM, the human body is visualized as a small universe, a microcosm, within a larger universe, a macrocosm, whereby inputs of the macrocosm (food, air, medication or stimuli arousing the five senses) affect qualities of the body’s energy field. Per the traditional Chinese medical texts, the human body contains a vital life energy, or qi, that circulates to every part of the body through an intricate channel network known as the meridian system. There are twelve primary meridians in the human body: six yang meridians on the posterior body and six yin meridians on the anterior body (Figure 1). There are also eight extraordinary meridians. Positioned along these meridians are more than 300 acupuncture points (i.e. acupoints), located on regions of the dermis with low electrical resistance and close to nerve bundles. Acupuncture utilizes a stainless-steel needle to stimulate these acupoints, which each contain a specific therapeutic action. Furthermore, stimulating a combination of acupoints can elicit varied healing effects. This stimulation of the acupoint(s) promotes the circulation of qi and helps to restore the steady internal physical and chemical milieu within the human body. In optimal health, qi harmoniously flows through the meridians to provide the body with the instructional intelligence required to maintain normal physiological activity and balance bodily functions. According to TCM, when disruptions of the flow of qi through the meridian pathways occur due to insufficient or stagnant qi, patterns of organ disharmony will ensue resulting in pain and/or disease. Another important theory in TCM is the concept of dualism represented by the symbols, yin and yang. These two opposing forces are complementary and remain in constant flux in order to maintain balance within the body. According to Chinese philosophy, any disharmony in proportion of yin and yang will result in patterns of hyper- or hypoactivity within the body and contribute to the development of a diseased state. Therefore, one unique property of acupuncture is that the same stimuli applied to the same acupuncture point can induce opposite regulatory responses under different physiological conditions. In other words, stimulation of a specific acupoint can either increase insufficient qi, decrease excessive qi, circulate stagnant qi, or stabilize disharmonious qi depending on the individual’s unique pathophysiology. For example, the acupoint that runs along the large intestine meridian has been shown to promote gastric peristalsis in individuals with low initial gastric motility and suppress peristalsis in individuals with active initial motility [4]. This dual regulatory feature of acupuncture aids in restoring the harmonious flow of qi, rebalancing patterns of disharmony, and eliciting a return to health. This is the basis of acupuncture theory.
Common Acupoints For Treating Gastrointestinal Disorders
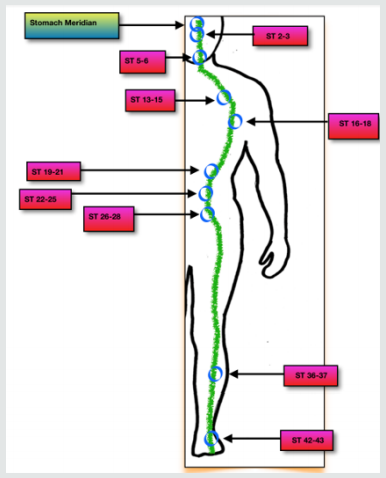
The most common acupuncture points used to treat symptoms associated with digestive disorders include those of the stomach (Figure 2) and large intestine (Figure 3). These points are generally treated in combination with other points and/or in conjunction with moxibustion and herbs. The exact treatment plan will depend on the specific diagnosis of each patient, based on diagnostic procedures (i.e. tongue, appearance, heart rate, and other vital signs). Rather than treating primary symptoms, TCM adopts a holistic approach that addresses the complex patterns of disharmony in the body.
Healing the Common Gastrointestinal Disorders with Acupuncture
Although acupuncture is best known for its analgesic and anesthetic properties, numerous randomized controlled trials, systematic reviews and meta-analyses have documented its clinical efficacy for treating a number of acute and chronic digestive conditions such as peptic ulcer disease, irritable bowel syndrome (IBS), chronic atrophic gastritis, and inflammatory bowel disease (IBD) [5-7]. The most common causative factors of these diseases include perturbations in intestinal motility, mucosal inflammation, functional disturbances in intestinal smooth muscle, visceral paresthesia, gastrointestinal hormone imbalances, and dysregulation of the brain-gut axis which manifests itself in symptoms such as abdominal pain, distension, and alterations in defecatory function [8]. Evidence from a considerable number of studies indicates that acupuncture effectively antagonizes the intestinal inflammatory response, promotes GI mucosal epithelial restitution, restores intestinal barrier function, normalizes gut motility and peristalsis, and attenuates chronic visceral hyperalgesia [9-13]. Recently, researchers at the Shanxi Provincial People’s Hospital conducted a human clinical trial to determine the efficacy of acupuncture for the treatment of patients with chronic atrophic gastritis, a condition characterized by chronic inflammation of the stomach and mucosal lining. Following a six-week treatment cycle, the cohort receiving acupuncture demonstrated superior clinical outcomes compared to the group receiving conventional drug therapy (i.e. proton pump inhibitor, antibiotics, anti-inflammatory drugs). According to the results, the symptom severity improvement rate for the group receiving acupuncture was 92.5% compared to 77.4% in the control group. The acupuncture group also demonstrated an 88.7% improvement rate in quantifiable microscopic results compared to 73.6% in the control group. The improvement rate for Helicobacter pylori clearance was 84.9% in the acupuncture group compared to 86.8% in the control group. These results suggest that acupuncture outperforms conventional drug therapy for relieving symptoms associated with chronic atrophic gastritis and inducing biochemical responses that provide protection to the gastric mucosa [14]. In a randomized control trial performed on patients with irritable bowel syndrome (diarrhea-predominant type), acupuncture treatment (“Soothing Gan & Invigorating Pi”) produced significantly greater clinical improvements in the degree and frequency of patient symptoms such as abdominal pain, distension, fecal incontinence, and rectal tenesmus as well as significantly increased quality of life scores compared to the control group who received conventional drug therapy [15]. Numerous other studies have corroborated these findings and concluded that the curative effects of acupuncture may exceed conventional drug therapy in the treatment of adverse symptoms associated with gastrointestinal dysfunction as well as significantly improving overall quality of life [16,17].
Conclusion
A growing body of literature continues to support the efficacy of acupuncture for alleviating adverse gastrointestinal symptoms associated with various GI disorders. Current evidence indicates the potential for acupuncture to treat GI disorders through regulating intestinal motility, reducing visceral sensitivity, antagonizing intestinal inflammation, and modulating neuroendocrine mechanisms involved in the gut-brain axis. While the evidence is compelling and consistent, there remains multiple challenges inherent in the study design of acupuncture research that may impede the production of truly objective analysis. Clinical studies of acupuncture are complicated by the fact that applying stimulation to the same acupoint with different manipulation tactics, frequencies of stimulation, and basal body conditions sometimes yield discordant results. In addition, devising a physiologically inert needling procedure that is indistinguishable from real acupuncture remains a challenge. Therefore, the lack of adequate control groups has made it difficult to properly interpret the data in acupuncture research. Despite these methodological obstacles, the current state of clinical evidence validating the efficacy of acupuncture remains an important consideration in the era of increasing consumer interest in complementary alternative treatment methods. While these studies elucidate the therapeutic benefits of acupuncture unaccompanied by other interventions, it is important to emphasize that achieving optimal GI health requires a multifactorial approach that combines healthy dietary and lifestyle modifications that aim to reduce chronic stress, inflammation, and exposure to environmental toxins. Nevertheless, acupuncture may provide an effective adjunct long-term solution for treating gastrointestinal disorders and its symptomatology.
References
- (2009) National Institutes of Health, U.S. Department of Health and Human Services. Opportunities and Challenges in Digestive Diseases Research: Recommendations of the National Commission on Digestive Diseases. US Government Printing Office, Bethesda, USA, pp 08-6514.
- Wu ZL (2017) Analysis of therapeutic effect of acupuncture and moxibustion on functional dyspepsia. Asia-Pacific Traditional Medicine 13(2): 112-113.
- Du MH, Luo HM, Hu S, Lv Y, Lin ZL, et al. (2013) Electroacupuncture improves gut barrier dysfunction in prolonged hemorrhagic shock rats through vagus anti-inflammatory mechanism. World J Gastroenterol 19 (36): 5988-5999.
- Wang H, Wang CY, Zhang JS, Sun L, Sun JP, et al. (2005) Acupuncture therapy for experimental stomach ulcer and c-Fos expression in rats. World J Gastroenterol 11: 5517-5520.
- MacPherson H, Bland M, Bloor K, Cox H, Geddes D, et al. (2010) Acupuncture for irritable bowel syndrome: a protocol for a pragmatic randomised controlled trial. BMC Gastroenterol 10 (63).
- Rafiei R, Ataie M, Ramezani MA, Etemadi A, Ataei B, at al. (2014) A new acupuncture method for management of irritable bowel syndrome: A randomized double-blind clinical trial. J Res Med Sci 19(10): 913-917.
- Tian SL, Wang XY, Ding GH (2008) Repeated electro-acupuncture attenuates chronic visceral hypersensitivity and spinal cord NMDA receptor phosphorylation in a rat irritable bowel syndrome model. Life Sci 83(9-10): 356-363.
- Xing J, Larive B, Mekhail N, Soffer E (2004) Transcutaneous electrical acustimulation can reduce visceral perception in patients with the irritable bowel syndrome: a pilot study. Altern Ther Health Med 10(1): 38-42.
- Lin YP, Yi SX, Yan J, Chang XR (2007) Effect of acupuncture at Foot-Yangming Meridian on gastric mucosal blood flow, gastric motility and brain-gut peptide. World J Gastroenterol 13(15): 2229-2233.
- Li XP, Yan J, Yi SX, Chang XR, Lin YP, et al. (2006) Effect of electroacupunture on gastric mucosal intestinal trefoil factor gene expression of stress-induced gastric mucosal injury in rats. World J Gastroenterol 12 (12): 1962-1965.
- Xu GY, Winston JH, Chen JD (2009) Electroacupuncture attenuates visceral hyperalgesia and inhibits the enhanced excitability of colon specific sensory neurons in a rat model of irritable bowel syndrome. Neurogastroenterol Motil 21(12): 1302-e125.
- Chao GQ, Zhang, S (2014) Effectiveness of acupuncture to treat irritable bowel syndrome: a meta- analysis. World J Gastroenterol 20(7): 1871-1877.
- Ren BB, Yu Z, Xu B (2012) Overview of the two-way regulatory effect of acupuncture on gastrointestinal motility. Zhongguo Zhen Jiu 32(8): 765-768.
- Zhang Y, Xue ZX, Hu W (2016) Effect of acupuncture on chronic atrophic gastritis complicated with Helicobacter pylori infection [J]. Shaanxi Journal of Traditional Chinese Medicine 37(08): 1078-1079.
- Zhang Y, Liu CC, Lian LY, Shen JC, He QD, at. al (2018) Time-effect relationship and molecular mechanism of electroacupuncture for repair of gastric mucosal lesion . Chinese Acupuncture and Moxibustion 38(7): 747-752.
- Sun JH, Wu XL, Xia C, Xu LZ, Pei LX, et al. (2011) Clinical evaluation of Soothing Gan and invigorating Pi acupuncture treatment on diarrhea-predominant irritable bowel syndrome. Chinese Journal of Integrative Medicine 17(10): 780-785.
- Zeng LF, Tuo L (2017) Effect of Acupuncture on Dyspepsia with Sleep Disorders. Liaoning Journal of Traditional Chinese Medicine 44(2): 359-361.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...