Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1652
Research Article(ISSN: 2641-1652) 
Diagnosis of Excess Bacterial Growth Syndrome in the Small Intestine in Patients with Bauhinia Deficiency and after its Surgical Correction as a Possible Cause of Toxic Endogenous Hepatitis Volume 2 - Issue 4
Vladimir Leonidovich Martynov* and Natalia Vladimirovna Kazarina
- Headquarters of the State Educational Establishment of the City of Nizhny Novgorod, Russia
Received:June 13, 2019; Published: July 23, 2019
*Corresponding author:Martynov VL, Headquarters of the State, Educational Establishment of the City of Nizhny Novgorod, Russia
DOI: 10.32474/CTGH.2019.02.000142
Abstract
Objective: to determine the syndrome of excessive bacterial growth in the small intestine (SIBO) in patients with insufficiency of the bauhinia valve (NBZ) and after its surgical correction.
Methods of Examination: patients of the studied groups were examined using direct and indirect methods of diagnosis of SIBO. Bacteriological examination of ileal aspirate and other surgical material was performed. All patients underwent a hydrogen respiratory test with a load of lactulose and performed a qualitative reaction of urine to indican.
Characteristics of The Material: 50 patients were examined, of which 30 were included in the main group, who underwent surgical correction of NBZ - Bauginoplasty; 20 patients are included in the control group in which the ileocecal valve is consistent. Patients of the main group were examined before surgery and on the 7th and 45th day after Bauhinoplasty.
Main Results: all patients of the main group had SIBS of varying severity, in 80% of patients SIBS was localized in the distal small intestine. Patients with normal function of ileocecal valve syndrome of excessive bacterial growth did not suffer. Intraoperatively, 76% of patients showed signs of mesenteric mesentery of the small intestine, and the fact of bacterial translocation in SIBO was also confirmed. After 7 days after surgical correction of the Bauhinia valve, the normalization of peak and background excretion of hydrogen was observed in 37% of patients. For 45 days in all patients the hydrogen curve corresponded to the norm.
Conclusion: the deficiency of the bauhinia valve is obligately accompanied by the syndrome of excessive bacterial growth in the small intestine, surgical correction is an effective method for correcting the syndrome of excessive bacterial growth in patients with NBD.
Keywords: Excess Bacterial Growth Syndrome; Bauhinia Valve Insufficiency; Hydrogen Respiratory Test; Bauhinoplasty
Introduction
The deficiency of the Bauhinium Damper (NBZ) is widespread among the population. In the study of 900 protocols of irrigoscopy, performed for various indications and not related to the diagnostic search for a Bauhinia flap insufficiency, the NBZ was detected in 64% of patients as an accompanying finding [1]. Widespread NBZ among the population of Russia due to connective tissue dysplasia (DST) and an extensive range of diseases of the colon and terminal part of the small intestine, determining, respectively, the primary and secondary NBZ [2]. Diseases of the gastrointestinal tract (GIT) occupy a prominent place in the structure of the pathology of internal organs, in Russia they are about 2500 per 100 thousand population [3]. In recent years, much attention has been paid to functional diseases of the digestive organs, which is primarily due to their high prevalence and the costs incurred by health care in connection with the examination and treatment of such patients [4]. Leading experts say that irritable bowel syndrome (IBS) affects from 10 to 20% of the adult population of developed countries, which is up to 50% of all visits to a gastroenterologist [5]. According to recent studies, the frequency of DST among adolescents reaches up to 20% (in the cohort about 3000 studied, according to the data of Professor Nechaeva GI and 8.5% in a sample of 400 adults [6]. According to our data [1,2] classical appendectomy, and even more so appendectomy with technical difficulties and appendectomy under conditions of a complicated course of acute appendicitis, can lead to an insolvency of the bauhinia valve. The fact of intimate anatomical and functional proximity of the valve structures of the ileocecal junction and appendix is undeniable. Appendectomy destroys these connections and leads to the development of secondary acquired NBZ. Many authors [7-9] admit the fact of ascending retrograde infection of the small intestinal mucosa at NBD. A pathological condition in which the titer of microorganisms in the mucous membrane of the small intestine exceeds 105 CFU / ml, or colonization of the colonic flora occurs, has been called Small Bacterial Overgrowth Syndrome (SIBO).
SIBR is a pathological condition that develops as a result of bacterial contamination of the small intestine by various microflora and is accompanied by functional disorders of the digestive conveyor [10,11]. Direct evidence of the occurrence of SIBR in case of the failure of the Bauhinia Damper (NBZ) is the experience of Larry S Miller [9]. In a clinical experiment, the author modeled the ileocecal valve insufficiency by placing a 4-lumen probe behind the lips of the bauhinia valve in the direction of the ileum of 19 healthy volunteers during a colonoscopy. 1 month after the manipulation with the help of the hydrogen breathing test, all the subjects under study revealed a syndrome of excessive bacterial growth of the small intestine. Thus, by virtually destroying the Bauhinia flap, the author achieved the emergence of SIBR from volunteers. Currently, SIBO is recognized as a key pathogenetic mechanism in the development and persistence of many diseases of the digestive tract and associated extra-digestive conditions (bronchial asthma, dermatological atopy, diabetes, autoimmune allergic conditions, arthritis, obligate precancerous conditions, etc.). The actual prevalence of SIBO is unknown today. Clinically, this pathological condition is poorly diagnosable due to the nonspecificity of its symptoms, which are often attributed to the main disease that causes SIBO [12]. In fact, SIBO is extremely common in the presence of one or more predisposing pathological conditions. Thus, Ardatskaya MD [8] indicates that the frequency of detection of excessive bacterial growth in the small intestine in various diseases (chronic gastritis, peptic ulcer, chronic cholecystitis, pathology of the hepatobiliary system, inflammatory and other intestinal diseases (in tons. irritable bowel syndrome), scleroderma, neuropathy (as a complication of diabetes mellitus), the effects of surgery, etc.) is 40-99%. The results of the last metaanalysis [13], which included 11 studies, showed that pathological respiratory tests are much more frequently recorded in patients with IBS than in healthy individuals (OR = 4.46; 95% CI = 1.69 - 11, 80). Similar results were achieved in the second meta-analysis, published a year later, - pathological test results were significantly more frequent in patients with IBS: odds ratio (OR) 4.46, 95% confidence interval (CI) 1.69-11.80. At the same time, taking into account age and gender showed an even more significant result (OSH 9.64, 95% CI 4.26-21.82. According to the literature, the problem of SIBR is currently a purely therapeutic one. Treatment of bacterial overgrowth syndrome in the small intestine provides for the treatment of the underlying disease, replacement therapy for malabsorption syndrome and antibacterial therapy [14,10]. The main group of drugs used for SIBR is intraintestinal antibiotics [15- 17]. It should be recognized that in the absence of an impact on the cause, successful pathogenetic treatment is temporary, which is confirmed by the example of rifaximin therapy. The frequency of recurrence of SIBR after effective therapy with rifaximin reached 44% after 9 months [18]. Many authors [10,19] separately stop at an obvious conclusion - the prediction of the SIBR and the risk of its recurrence after successful antibiotic therapy depends primarily on the therapeutic effect on the primary background disease that has contributed to the contamination of the small intestine [18,20] rightly points out that the recurrence of SIBO in the event of persisting predisposing causes often leads to a chronic process and a complex, and sometimes impossible, conservative correction.
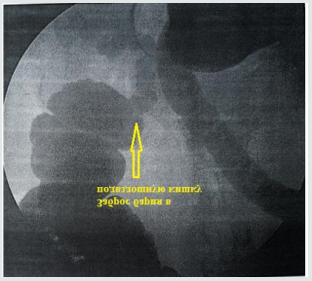
Thus, we have not encountered literary data that would describe etiotropic therapy. In our opinion, the problem of SIBO in patients with functional pathology of the gastrointestinal tract in many cases is due to damage to a specific anatomical structure, namely, the Bauhinia valve, which is a surgical problem. We have not met domestic studies on the etiotropic effect on the syndrome of excessive bacterial growth in patients with proven deficiency of the bauhinia valve. The few foreign works [7,9] are devoted only to the statement of the fact that there is a SIBR at the NBZ. The purpose of the study is to determine the syndrome of excessive bacterial growth of the small intestine in patients with proven insufficiency of the bauhinia valve and after its surgical correction. Materials and methods. The study was conducted on the basis of the surgical department of the city hospital “Nizhny Novgorod City Clinical Hospital No. 12” in the period from September 2014 to December 2014. The main group included 20 patients (16 women, 8 men, age from 23 to 57 years) with proven by the results of irrigoscopy the insufficiency of the bauhinia valve. All patients of the main group performed Bauginoplasty according to the methods of prof. Martynova V.L. A control group of 20 patients was also formed (11 women, 9 men, age from 28 to 49 years), who underwent an irrigoscopy in order to diagnose diseases of the large intestine, according to the results of which the ileo-cecal valve turned out to be wealthy. Simultaneously, patients of the main group underwent appendectomy. The removed vermiform process was sent for histological examination. In the case of intraoperative diagnosis of mesenteric mesentery of the ileum, the altered lymph node was resected, a back seed from a section of the lymph node was performed, and his histological examination was performed. Preparation for irrigoscopy was carried out for two days and consisted in the prohibition of food intake containing slags, in the formulation of high enemas with a total volume of 1.5 to 3 liters 3-4 times a day. It is imperative to thoroughly empty the cecum from the intestinal contents, since its presence in the form of an embossed mass may prevent the radiopaque substance from passing into the ileum with the failure of the bauhinia valve. This can lead to a false negative conclusion. The taut intestine must be filled with a radiopaque substance. Repeated X-ray examination after a bowel movement is fundamentally important, since during bowel movement a maximum pressure is created in the intestine, which, if the ileocecal locking apparatus fails, will be accompanied by a pronounced reflux of the radiopaque substance into the ileum (Figure 1). We performed intraoperative digital diagnostics of the failure of the bauhinia valve. Normally, the gap of the thin-colic transition is no more than 2cm and does not miss the first finger of the surgeon’s left hand. In the NBZ environment, on average, this transition has a diameter of 3.3-5.4cm, which determines the almost unhindered passage of 1 finger of the left hand (so conveniently) by the surgeon into the ileum. The technique consists in the following: after extracting the ileocecal angle from the right ileal fossa, the surgeon 1 finger of the left hand brings the lateral wall of the ascending colon, opposite the ileocecal anastomosis, closer to this anastomosis and tries to insert it and the finger into the ileum. With its introduction into the ileum, in our opinion, the diagnosis of NBZ is established (Figure 2). If it is impossible to perform this manipulation, the diagnosis of the NBZ can be rejected. Direct intraoperative diagnostic method for small intestine SIBR is a bacteriological examination of aspirate of the intraluminal and mucosal contents of the distal ileum (Figure 3(a)). The technique of material sampling is as follows: 20cm proximal to the ileocecal junction after isolation of the 10-cm long loop of the ileum with a length of 10cm by ileum intestinal tissue, the lumen puncture is performed. The needle is held obliquely relative to the intestinal wall, 10 ml of sterile physiological NaCl solution is injected into the intestinal cavity.
Figure 2: The first finger of the left hand of the surgeon with the lateral wall of the ascending colon is inserted into the ileum. Intraoperative digital diagnosis NBZ installed.

Figure 3(a): Intraoperative sampling of the intraluminal and mucosal contents of the distal ileum followed by bacteriological examination.

Figure 3(b): Intraoperative sampling of the intraluminal and mucosal contents of the distal ileum followed by bacteriological examination.
The exposure is maintained for 5 minutes, the contents of the isolated ileum are aspirated, until the needle passes through the mucous layer of the intestine, the needle is removed. The puncture site is peritonized. Aspirate is sent for bacteriological examination. Indirect techniques included the determination of urinary indican (by the method of Obermeyer) before the operation and on the 7th and 45th day after bauginoplasty; hydrogen respiratory test (VDT) with a lactulose load, which was carried out using a Gastrolyser apparatus before the operation and on the 7th and 45th day after the operation. A preoperative study of patients with NBZ using these techniques was performed prior to the radiopaque examination of the intestine, or 4 weeks after irrigoscopy. Patients of the main group did not receive antibiotic therapy in the postoperative period. Preoperative preparation consisted of 3-fold cleansing enemas, which could not affect the biocenosis of the small intestine. In order to determine the syndrome of excessive bacterial growth in the patients of the control group, indirect diagnostic methods were carried out, which included the determination of urine indican (by the method of Obermeier) and VDT with a load of lactulose, performed using a Gastrolyser apparatus. The study preceded the irrigoscopy. Preparation of patients for VDT with lactulose was carried out according to the method proposed by [21]. The diagnostic criterion for the presence of SIBS in patients was an increase in H2 excretion after exercise in the period from 0 to 60 min by 10 ppm (in the absence of abdominal symptoms after lactulose, such as abdominal pain, rumbling, flatulence, diarrhea) and 5 ppm (in the presence of abdominal symptoms). The group included patients with basal secretion of hydrogen up to 5ppm. It was carried out using statistics.
Results and Discussion
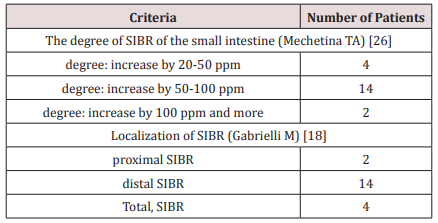
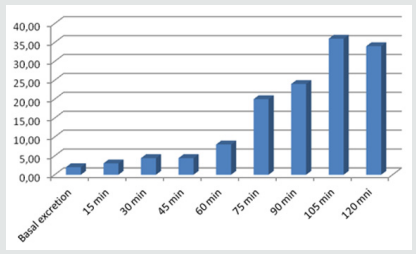
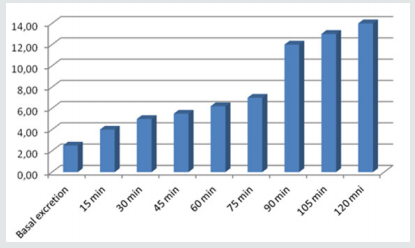
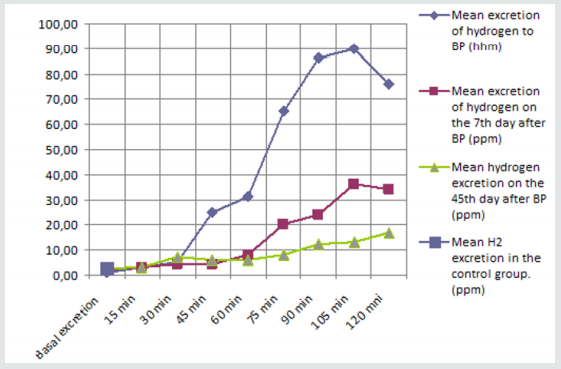
Postoperative complications in the patients of the main group were not observed. The proposed preoperative irrigoscopy. It was confirmed that a chronic inflammatory catarrhal was observed in all 20 cases. Intraoperative mesadenitis was detected in 16 patients of the main group. It has been shown that there has been no clear link between the cortical and cerebral layers. The following is the result: E. coli hemolytic was determined in 9 cases (104 CFU / ml), St. aureus - in 7 cases (103-4 CFU / ml). It has been taken for 20 patients who have been diagnosed in the biocenosis. The spectrum of microorganisms is determined by the following microorganisms: E. coli hemolytic was determined in 10 patients (105-107 CFU / ml), St. aureus - in 6 patients (106-108 CFU / ml), C. albicans - in 4 patients (105-109 CFU / ml). The sown flora is identical. Bauginoplasty (BP) according to the results of the patient’s patient’s life cycle (Figure 3(b)), the colony peak at 90th minute) (Table 1).
Mean Excretion of Hydrogen in The Main Group Before BP (N=20)
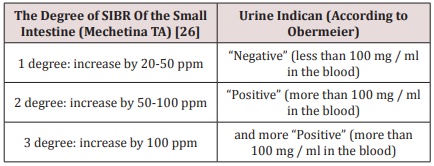
The determination of urinary indican in patients of the main group before surgical correction gave positive results in 16 cases (Table 2). The presence of an insignificant (1 degree - increase up to 50 ppm) distal syndrome of excessive bacterial growth in 4 patients in whom urine indican was negative may indicate a lack of sensitivity of this screening test compared to VDT.
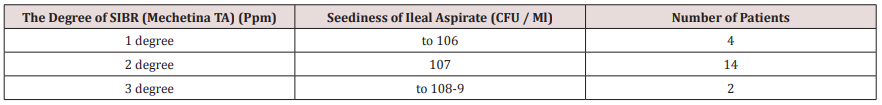
Mean excretion of hydrogen on the 7th day after BP (n=20)
On the 7th and 45th days of the postoperative period, in the absence of antibiotic therapy, indican urine in all operated patients (n = 20) was negative. According to the results of VDT with lactulose load in patients of the main group on the 7th day after the Bauginoplasty (BP) (Figure 4), all of the patients underwent a significant reduction in the amount of hydrogen released, while the lactulose passage through the intestines normalized (the large intestinal peak is determined at 75 minute).
Mean hydrogen excretion on the 45th day after BP (n=20)
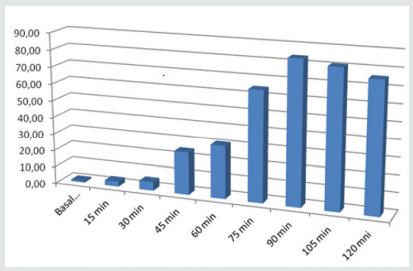
On the 45th day after Bauginoplasty, VDT corresponded to the norm in all patients (Figure 5). Results of H2 excretion in patients of the main group on the 45th day after the operation. The urine index in the control group of patients with the proven consistency of the bauhinia valve was confirmed with an irrigoscopy. The results of the hydrogen respiratory test in the control group (Figure 6) did not differ from the normal values described in the literature [22].
Average Hydrogen Excretion in The Control Group (N=20)
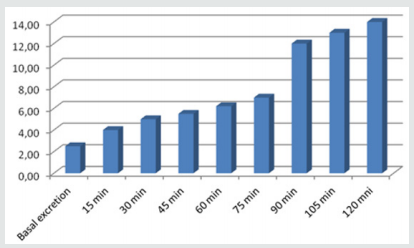
(Figure 6) Results of excretion of H2 in patients of the control group. Our studies confirm the presence of small intestine SIBR in patients with NBZ, which is consistent with the data of foreign authors [7,9] and fits into the logic of colonic reflux pathogenesis in the small intestine. On the reliability of the data in this study cannot speak. However, an obvious difference is found in the results of VDT in patients of the compared groups: a significant decrease in the concentration of hydrogen released after the operational benefit (Figure 7). The first facts obtained objectively indicate the effectiveness of Bauginoplasty, the positive clinical results of which we observed in 500 operated patients with NBZ [2]. (Figure 7) Comparative characteristics of H2 excretion in patients of the control and main groups before and after bauginoplasty. The results of the bacteriological examination of the ileum aspirate of patients with NBZ confirm the presence of SIBR detected by HTD with a load of lactulose. At the same time, a correspondence was established between the degree of SIBR (according to the results of VDT) and the degree of contamination of ileal aspirate (Table 3). This is consistent with the data of E Mendoza [21], which established the sensitivity (85.7%) and specificity (90.9%) of the hydrogen breath test with lactulose compared with the “gold standard”. The determination of indican urine makes it possible to suspect SIBS in patients with a pronounced degree of dissemination of the small intestine (increased H2 excretion above 50 ppm), but not informatively in patients with SIBS grade 1 (elevation of H2 to 50 ppm) compared to VDT. The revealed diagnostic value of this method retains its value as a screening test for small intestine SIBR of 2 and 3 degrees. The phenomena of mesadenitis and the presence of microorganisms in the lymph nodes confirm the translocation of microorganisms through the intestinal wall. The fact of bacterial translocation diagnosed in patients with SIBO of the small intestine under NBZ conditions is consistent with the literature data [23-27].
Figure 7: Comparative characterization of H2 excretion in patients of the control and main groups before and after biogenetic.
Findings
a) Patients with a normally functioning ileocecal valve are not predisposed to the formation of a distal SIBO.
b) SIBR is obligately associated with the NBZ and determines the process of bacterial translocation.
c) A positive qualitative reaction of urine to indican indicates that the patient has a SIBO of the 2nd degree and higher.
d) SIBO was determined in 20 (100%) patients with NBZ: 1 degree - in 4 (20%) patients; Grade 2 in 14 (70%) patients; Grade 3 in 2 (10%) patients;
e) On the 7th day after Bauginoplasty, SIBR Grade 1 was determined in 8 (40%) patients, and in 12 (60%) operated patients, data for SIBO were not revealed according to the results of VDT;
f) On the 45th day after Bauginoplasty, the concentration of hydrogen released corresponded to the norm;
g) Bauginoplasty - a method of etiopathogenetic impact on the syndrome of excessive bacterial growth in the small intestine in patients with NBZ
References
- Martynov, VL (2013) Surgical treatment of reflux disease: Monograph V L Martynov. Nizhny Novgorod, Publishing house LLC, Center for operational printing, pp.535.
- Martynov VL (2006) Refluxes of the digestive tract and their surgical correction: dis Dr honey Sciences: Martinov Vladimir Leonidovich. Saransk, pp. 261.
- Filippova, TV (2014) The value of medical genetic counseling for diseases of the digestive system T V. pp. 56-61.
- Sheptulin A A (2010) Gastroesophageal reflux disease and functional diseases of the gastrointestinal tract: is there any connection? pp. 44-48.
- Sperber AD, Drossman DA, Quigley EM (2012) The Global Foundation for World Gastroenterology Organization symposium. Am J Gastroenterol 107(11): 1602-1609.
- Nechaeva GI, Yakovlev VM, Gromova OA, Torshin I Yu (2009) Connective tissue dysplasia in children and adolescents. Innovative hospital-saving technologies for diagnosis and treatment in pediatrics. M: Union of Pediatricians of Russia, pp. 96.
- Oren Zaidel, (2003) Uninvited Guests: The Henry C. Lin. Practical Gastroenterology.XXVII (7): 24-37.
- Ardatskaya MD (2011) Syndrome of excess bacterial growth: a tutorial / MD Ardatskaya-Moscow: Forte print, pp: 56.
- Larry S Miller, Anil K. Vegesna, Aiswerya Madanam Sampath, Shital Prabhu, Sesha Krishna Kotapati, et al. (2012) Ileocecal valve dysfunction in small intestinal bacterial overgrowth: A pilot study. World J Gastroenterol 18: 6801-6808.
- Curly, Yu A Kucheryavy, SV Cheryomushkin, EA Mayevskaya, EA Sutugina (2014) Interrelation of irritable bowel syndromes and excessive bacterial growth: is it there? p. 5-14.
- Maev, NYu Ivashkina, Yu A Kucheryavy, TS Oganesyan Eksper (2011) Diagnosis and treatment of the syndrome of excessive bacterial growth in the small intestine. wedge gastroenterol, pp. 125- 129.
- Bures J, Cyrany J, Kohoutova D, Forst LM, Rejchr T S, et al. (2010) Small intestinal bacterial overgrowth syndrome. M World J Gastroenterol 28 :2978-2990.
- Ford AC, Spiegel BM, Talley NJ, Moayyedi P (2009) Small intestinal bacterial overgrowth in irritable bowel syndrome: review and meta-analysis. Clin Gastroenterol Hepatol 7(12): 1279-1286.
- Avdeev v (2010) Diagnosis and treatment of bacterial overgrowth syndrome in the small intestine. V Avdeev Doctor, pp.1-3.
- Plotnikova, E Yu Plotnikova, M. V. Borsch, M. V. Krasnova, E. N. Baranova (2013) Some aspects of diagnosis and treatment of excessive bacterial contamination of the small intestine in clinical practice [electronic resource] Attending doctor.
- Poluektova, EA Poluektova, S. Yu. Kuchumova, A. A. Sheptulin, V. T. Ivashkin (2013) Treatment of irritable bowel syndrome from the standpoint of modern ideas about the pathogenesis of the disease RZGGK. 23(1): 57-65.
- Kucheryavyi, Yu A, TS Oganesyan (2010) Syndrome of excess bacterial growth RGGGK. 5: 63-68.
- Gabrielli M, Bonazzi P, Scarpellini E, Bendi AE, Lauritano EC, et al. (2011) Prevalence of small intestinal bacterial overgrowth in Parkinson's disease. Mov Disord 26(5): 889-892.
- Lauritano E, Gabrielli M, Scarpellini E, Lupascu A, Novi M, Sottilii S, et al. (2008) Small intestinal bacterial overgrowth recurrence after antibiotic therapy. Am J Gastroenterol 103(8): 2031-2035.
- Gabrielli M, GD Angelo, TD I Rienzo, E Scarpellini, V Ojetti (2013) Diagnosis of small intestinal bacterial overgrowth in the clinical practice. European Review for Medical and Pharmacological Sciences 17: 30-35.
- Mendoza, E Crismatt C, Matos R (2007) Diagnosis of small intestinal bacterial overgrowth in children. Biomedical 27 (3): 325-332.
- Wiest R, Garcia Tsao G (2005) Bacterial translocation in cirrhosis. Hepatology 41: 422-433.
- Hashimoto N, Ohyanagi H (2002) Effect of portal portal hypertension on gut mucosa. Hepatogastroenterology 49 :1567-1570.
- Heuman, D Abu-assi, SG, Habib AM (2004) Persistent ascites and low sodium, identify patients with MELD scores and low MELD scores who are at high risk for early death. Hepatology 40: 802-810.
- Zharkova MS, MV Mayevskaya, VT Ivashkin (2012) Influence of excess bacterial growth syndrome and bacterial translocation on the course of the disease in patients with cirrhosis of the liver. MS Zharkova RGGG 22(5): 56-63.
- Mechetina, Tatyana Anatolevna Mechetina Moscow (2011) Syndrome of excessive bacterial growth in the small intestine after cholecystectomy: dis Cand. honey Sciences, pp.134.
- Ledochowski M (2008) Hydrogen Breath tests. (1st edn) Innsbruck: Akademie, pp.59.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...