
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1652
Research Article(ISSN: 2641-1652) 
Childhood Intussusception: Profile of Infants with Pathologic Lead Points Volume 3 - Issue 5
Chukwubuike Kevin Emeka1*, Igweagu Chukwuma Paulinus2 and Anijunsi Livinus Patrick1
- 1Department of Surgery, Enugu State University Teaching Hospital, Nigeria
- 2Department of Community Medicine, Enugu State University Teaching Hospital, Nigeria
Received: August 02, 2022; Published: August 17, 2022
*Corresponding author: Chukwubuike Kevin Emeka, Department of Surgery, Enugu State University Teaching Hospital, Nigeria
DOI: 10.32474/CTGH.2022.03.000173
Abstract
Background: Intussusception is considered an acquired disease of infants and most of the times, the etiology is not known (idiopathic). The presence of a pathologic lead point causing intussusception is uncommon in infants. The aim of this study was to evaluate our experience with regards to infants who were managed for intussusception and were found to have pathologic lead point (PLP) at surgery.
Materials and Methods: This was a retrospective study of children, aged 1 year and younger (infants), who were operated upon for intussusception at the pediatric surgery unit of a teaching hospital in Enugu, Nigeria. Only patients with confirmed intussusception resulting from a pathologic lead point at surgery were enrolled into the study. The information analyzed included the patients’ demographics, intra-operative finding, operative procedure performed and outcome of treatment.
Results: A total of 181 cases of intussusceptions in infants were operated upon during the study period. Out of this number, 4 (2.2%) infants had a pathologic lead point. Equal number of males and females were affected. Abdominal pain and passage of red currant jelly stool were consistent symptoms in the patients. Two patients had Meckel’s diverticulum. One patient each had intestinal duplication cyst and intestinal lymphoma as their pathologic lead point. All the patients had resection of the pathological lead points with end-to-end intestinal anastomosis. Wound infection and stitch related complications were the post-operative complications. The overall outcome of treatment was good.
Conclusion: Childhood intussusception is a common cause of acute abdomen in children and pediatric abdominal surgical emergency. Majority of the intussusception in infants is idiopathic. However, a small number of infants may have pathologic lead point. Meckel’s diverticulum, intestinal duplication cysts and lymphoma are the pathologic lead points recorded in the present study.
Meckel’s Diverticulum; Intussusception; Infants; Pathologic Lead Point; Lymphoma
Introduction
The invagination of a portion of the intestine into another segment is defined as intussusception. Intussusceptum is the portion that invaginates while the portion that receives the intussusceptum is the intussuscipiens [1]. Intussusception is a common cause of pediatric abdominal surgical emergency as it causes intestinal obstruction in children [2]. The peak age of occurrence of childhood intussusception has been referenced as 4 to 10 months and its published incidence is between 34 and 100 per 100,000 children [3,4]. The cause of intussusception in infants is mostly unknown (idiopathic). However, pathologic lead point may also be found in infants and the incidence of the pathological lead point causing intussusception varies from 0.3 to 20 percent [5]. The origin of these lead points could be from mucosal, intramural or extrinsic structures. Such pathological lead points may include Meckel diverticulum, enlarged lymph nodes, duplication cysts, submucosal hematomas, ectopic pancreatic and gastric rests, hemangioma, foreign body, benign and malignant tumors of mesentery and intestine [6]. The clinical presentation of intussusception may include abdominal pain, vomiting and passage of red currant jelly stool. Ultrasound is the investigation of choice for the diagnosis of intussusception because of its high sensitivity and specificity [7]. Management of intussusception could be nonoperative or operative. Although intussusception is considered a disease of infancy where no cause is mostly found, however, occurrence of intussusception in infants secondary to pathologic lead point (PLP) is a relatively infrequent event. The aim of this study was to evaluate our experience with regards to infants who were managed for intussusception and were found to have PLP at surgery.
Materials and Methods
This was a retrospective study of children, aged 1 year and younger, who were operated upon for intussusception between January 2016 and December 2020 at the pediatric surgery unit of Enugu State University Teaching Hospital (ESUTH) Enugu, Nigeria. Diagnosis of intussusception was made based on clinical and imaging findings and confirmed at surgery. Patients who presented primarily to ESUTH and those referred from peripheral hospitals were recruited into the study. Patients who are older than 1 year of age and those without intussusception at surgery were excluded from the study. Only patients with confirmed intussusception resulting from a pathologic lead point at surgery were enrolled into the study. All the PLP(s) were sent for histopathological evaluation which confirmed the diagnosis. ESUTH is a tertiary hospital located in Enugu, Southeast Nigeria. The hospital serves the whole of Enugu State, which according to the 2016 estimates of the National Population Commission and Nigerian National Bureau of Statistics, has a population of about 4 million people and a population density of 616.0/km2. The hospital also receives referrals from its neighboring states. Information was extracted from the case notes, operation notes, operation register and admission-discharge records. The information extracted included the patients’ age, gender, presenting symptoms, symptoms duration, time interval between presentation and surgical intervention, intra-operative finding/type of PLP, definitive operative procedure performed, complications of treatment, duration of hospital stay and outcome of treatment. The follow-up period was 12 months. Ethical approval was obtained from the ethics and research committee of ESUTH and informed consent from the patients’ caregivers was not required because of the retrospective nature of the study and the identities of the patients were not revealed. Statistical Package for Social Science (SPSS) version 21 (manufactured by IBM Corporation Chicago Illinois) was used for data entry and analysis. Data were expressed as percentages, mean, and range.
Results
Patients’ Demographics
A total of 181 cases of intussusceptions in infants were managed during the study period. Out of this number, 4 (2.2%) infants had a pathologic lead point and form the basis of this report. Amongst these 4 patients, 2 were males and the other 2 were females. The mean duration of symptoms before presentation to the hospital was 5 days. The mean time interval between presentation to the hospital and surgical intervention was 24 hours. Following surgical treatment, the average duration of hospital stay was 12 days.
Presenting Symptom (n=4)
All the patients had abdominal pain and passage of red currant jelly stool. There was bilious vomiting in 3 (75%) infants and abdominal distension in 2 (50%) patients.
Intra-operative finding/types of pathologic lead point (n=4)
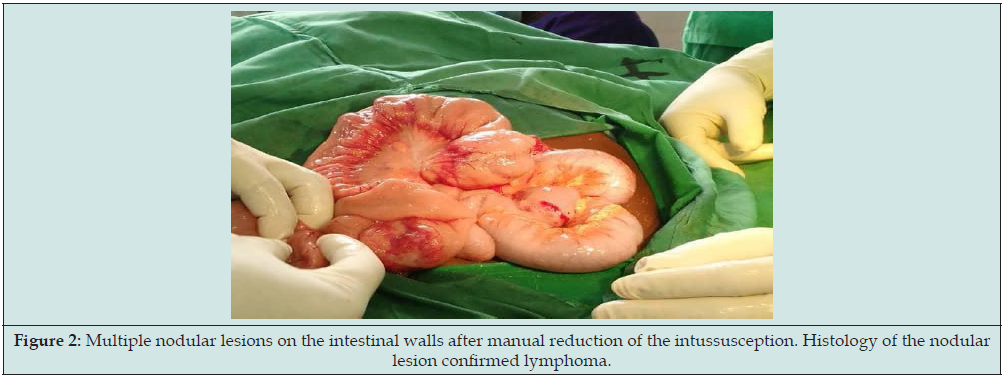
Two (50%) patients had Meckel’s diverticulum. One (25%) patient each had intestinal duplication cyst and intestinal lymphoma as their pathologic lead points. Figures 1 & 2 show Meckel’s diverticulum and intestinal lymphoma that caused intussusception.
Figure 2: Multiple nodular lesions on the intestinal walls after manual reduction of the intussusception. Histology of the nodular lesion confirmed lymphoma.
Definitive operative procedure performed
All the patients had resection of the pathological lead points with end-to-end intestinal anastomosis.
Complications of treatment
Wound infection was registered in 1 (25%) patient and there was stitch related complications in 1 (25%) patient.
Treatment outcome
All the patients survived the intussusception and its treatment. However, the patient that had lymphoma required chemotherapy.
Discussion
Intussusception was first described by Barbette of Amsterdam in 1674 and John Hunter described it in detail in 1789. Wilson in 1831 first successfully treated intussusception surgically. In 1876, Hirschsprung, a Danish pediatrician, first reported the technique of hydrostatic reduction and he subsequently reported a mortality of 35% that is attributable to intussusception. Unlike childhood intussusception, adult intussusception is uncommon, however, a pathologic lead point is found in 75% to 90% of adult intussusception [8]. In the present study, 2.2% of the infants had a pathologic lead point. This finding is comparable to the report of Cogley et al [9]. However, reports of pathologic lead points causing intussusception, as high as 25%, have also been documented [10]. The wide differences in the incidences of the pathologic lead point are difficult to explain but may be related to the cohort of patients studied. For instance, the incidence of pathologic lead point causing intussusception is higher in infants younger than 3 months of age [11]. Equal number of males and females had pathologic lead points in the current series. The reason for the gender parity, in pathologic lead point causing intussusception, is not known. Howbeit, idiopathic childhood intussusception has severally been published to occur more in males [12,13]. From the onset of symptoms to presentation to the hospital, a mean period of 5 days elapsed. This reflects the delayed presentation of the patients. Late presentation of patients is a regular finding in low-income countries due to poverty, ignorance and lack of awareness. It took an average of 24 hours to investigate, resuscitate and stabilize the patients for surgery. This long interval before surgery was necessitated by the poor clinical state of the patients prior to presentation. A mean period of hospital stay of 12 days was obtained in the index study. The duration of hospitalization of children with intussusception may be related to the extent of the surgical procedure and the postoperative course. Post-operative complications increase the patients’ period of hospital stay.
Abdominal pain was a consistent finding in children who presented with intussusception. However, painless intussusception has been reported especially in younger infants [14]. Children with intussusception manifest abdominal pain by sudden loud crying and they pull their knees to their chest while crying. Other symptoms such as vomiting, passage of red currant jelly stool, constipation and abdominal distension may be present. All the symptoms may not be present in all the patients and do not occur in a particular order; the sequence of occurrence of these symptoms may be in various combinations depending on the time of presentation. Meckel’s diverticulum was the most common pathologic lead point recorded in the current study. One study from Frankfurt, Germany also reported Meckel’s diverticulum as the most common pathologic lead point causing intussusception in children [15]. Khasawneh et al reported Meckel’s diverticulum and Henoch-Schonlein purpura as the most common pathologic lead point causing intussusception [16]. Meckel’s diverticulum is the most common congenital malformation of the gastrointestinal tract, and it occurs due to persistence of the vitello-intestinal duct. Meckel’s diverticulum is present in 2-4% of the population, measures about 2 inches in length, located 2 feet from the ileocecal valve and usually contains 2 ectopic gastric or pancreatic tissues [17]. Besides intussusception, other complications that may result from Meckel’s diverticulum include ulceration, hemorrhage, intestinal obstruction and perforation [18].
Intestinal (enteric) duplication cyst is an uncommon pathology that may serve as a pathologic lead point for intussusception. Al-Qahtani also reported duplication cyst as a lead point for intussusception [19]. Intestinal duplication cysts are rare congenital anatomical abnormalities of the digestive tract with an incidence of one in 4500 [20]. Intestinal lymphoma is a rare pathologic lead point that may cause intussusception. Several other studies have reported intestinal lymphoma triggering intussusception [21,22]. Lymphoma is a heterogeneous group of malignant tumors of the hematopoietic system and is characterized by the aberrant proliferation of mature lymphoid cells or their precursors [23]. The definitive surgical procedure performed was resection of the pathological lead points with end-to-end intestinal anastomosis. Although manual reduction of the intussusception was possible in the studied patients, bowel resection was still required because of the pathologic nature of the lesions and the high chance of intussusception recurrence. However, wedge resection of Meckel’s diverticulum can be performed if the base is narrow and there is no mass in the lumen of the diverticulum [24]. Surgical site infection was recorded postoperatively in one-quarter of the patients in the present study. Milano et al also reported an infection rate of 26% following laparotomy for intussusception [25]. Exposure of the surgical site to the pathogenic organisms of the intestinal tract may explain the high wound infection rates. Generally, the outcome of treatment of infants with intussusception caused by pathologic lead point is good. However, the nature of the pathologic lead point may determine the overall outcome. For instance, prognosis may be poor in infants with malignant pathologic lead point.
Conclusion
Childhood intussusception is a common cause of acute abdomen in children and a pediatric abdominal surgical emergency. Majority of the intussusception in infants is idiopathic. However, a small number of infants may have pathologic lead point. Meckel’s diverticulum, intestinal duplication cysts and lymphoma are the pathologic lead points recorded in the present study.
References
- Cera SM (2008) Intestinal intussusception. Clin Colon Rectal Surg 21(2): 106-113.
- Madan AJ, Haider F, Alhindi S (2021) Profile and outcome of pediatric intussusception: a 5-year experience in a tertiary care centre. Ann Pediatr Surg 17: 31.
- Jiang J, Jiang B, Parashar U, Nguyen T, Bines J, et al. (2013) Childhood intussusception: A literature review. Plos One 8(7): e68482.
- Buttery JP, Danchin MH, Lee KJ, Carlin JB, Mclntyre PB, et al. (2011) Intussusception following rotavirus vaccine administration: post-marketing surveillance in the National Immunization Program in Australia. Vaccine 29(16): 3061-3066.
- Yehouenou Tessi RT, El Haddad S, Oze KR, Mohamed T, Dinga E, et al. (2021) A Child’s Acute Intussusception and Literature Review. Glob Pediatr Health 8: 1-5.
- Gale HI, Gee MS, Westra SJ, Nimkin K (2016) Abdominal ultrasonography of the pediatric gastrointestinal tract. World J Radiol 8(7): 656-667.
- Li XZ, Wang H, Song J, Liu Y, Lin Y, et al. (2021) Ultrasonographic diagnosis of intussusception in children. J Ultrasound Med 40(6): 1077-1084.
- Kim KH, Namgung H, Park DG (2014) Adult intussusceptions: preoperative predictive factors for malignant lead point. Ann Surg Treat Res 86(5): 244-248.
- Cogley JR, O’Connor SC, Houshyar R, Al Dulaimy K (2012) Emergent US: what every radiologist should know. Radiographics 32(3): 651-665.
- Blakelock RT, Beasley SW (1999) The clinical implications of non-idiopathic intussusception. Pediatr Surg Int 14(3): 163-167.
- O, Daneman A (2004) Intussusception. Part 3: Diagnosis and management of those with an identifiable or predisposing cause and those that reduce spontaneously. Pediatr Radiol 34(4): 305-312.
- Navarro OM. Daneman A, Chae A (2004) Intussusception: The use of delayed, repeated reduction attempts and the management of intussusception of intussusceptions due to pathologic lead points in pediatric patients. AJR Am J Roentgenol 182(5): 1169-1176.
- Chukwubuike K (2020) Intussusception in Children treated on the basis of clinical features: A prospective observational study from Enugu State, Nigeria. Med J Zambia 47(3): 223-230.
- Chukwubuike KE, Ilo AC, Anijunsi LP (2022) Painless intussusception in children: Is it a recognized clinical entity? EC Gastroenterology and digestive system 9(6): 6-10.
- Fiegel H, Gfroerer S, Rolle U (2016) Systemic review shows that pathologic lead points are important and frequent in intussusception and are not limited to infants. Acta Paediatr 105(11): 1275-1279.
- R, El-Heis M, Al-Omari M, Al-Qaralleh MA, Al-Manasra AR, et al. (2021) The radiological characteristics of childhood intussusception including unusual features and rare pathological lead points. Heliyon 7(6): e7231.
- Sajar J, Kumar V, Shah DK. (2006) Meckel’s diverticulum: a systemic review. J R Soc Med 99(10): 501-505.
- Kuru S, Kismet K (2018) Meckel’s diverticulum: clinical features, diagnosis and management. Rev Esp Enferm Dig 110(11): 726-732.
- Al-Qahtani HH (2016) Enteric duplication cyst as a leading point for ileoileal intussusception in an adult: A rare cause of complete small intestinal obstruction. World J Gastrointest Surg 8(6): 472-475.
- Patino Mayer J. Bettolli M (2014) Alimentary tract duplications in newborns and children: diagnostic aspects and the role of laparoscopic treatment. World J Gastroenterol 20(39): 14263-14271.
- Shakya VC, Agrawal CS, Koirala R, Khaniya S, Rajbanshi S, et al. (2009) Intussusception due to non-Hodgkin’s lymphoma; different experiences in two children: two case reports. Cases J 2: 6304.
- Xu XQ, Hong T, Li BL, Liu W (2013) Ileo-ileal intussusception caused by diffuse B cell lymphoma of the ileum. World J Gastroenterol 19(45): 8449-8452.
- Mawardi H, Cutler C, Treister N (2009) Medical management update: non-Hodgkin lymphoma. Oral Surg Oral Pathol Oral Radiol Endod 107(1): e19-33.
- Sharma RK, Jain VK (2008) Emergency surgery for Meckel’s diverticulum. World J Emerg Surg 3: 27.
- Milano L (2016) Prognostic factors for surgical-site infection (SSI) event and length of hospitalization for children with intussusception post operative. 5(7): 00209.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...



