Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1652
Mini Review(ISSN: 2641-1652) 
Case of Application of Syrolimus in a Patient with Progressing Pultifocal Pepatic Nodular Hyperplasia Volume 3 - Issue 1
Garbuzov RV*, Polyaev Yu A, Donyush EK and Kondrashova ZA
- Russian children’s clinical hospital Pirogov Russian National Research Medical University, Russia
Received: March 09, 2020; Published: July 17, 2020
*Corresponding author: Garbuzov Roman, Doctor of Sciences MD, Department of Pediatric Surgery and Interventional Radiology, Russia
DOI: 10.32474/CTGH.2020.03.000153
Abstract
Introduction: A case presented to the public demonstrates the possibility of treatment with Sirolimus in a patient with progressive multifocal liver Focal Nodular Hyperplasia (FNH) with progressive growth and a tendency to formation of liver function insufficiency after splenorenal shunt for portal hypertension.
Material and Methods: Patient E. 08.03.2001 year of birth c Diagnosed with multifocal bilobar nodular liver hyperplasia after splenorenal bypass surgery for portal hypertension, established in 2018/ Sirolimus treatment was prescribed from 06.22.18 to the present.
Conclusion: As a result of the treatment with Sirolimus, a normalization of the level of liver enzymes, bilirubin in the blood is noted. According to radiation methods, a reduction in liver size and FNH size is up to 30%.
Keywords:Multifocal liver Focal Nodular Hyperplasia (FNH); Sirolimus
Introduction
Today, FNH is regarded as a benign vascular formation of the liver. VNG is the second most common benign liver neoplasm [1]. Edmonton first described it in 1958 [2]. FNH most often occurs as a monofocal lesion, in more rare cases there are two or more nodes [3]. FNH is believed to be a hyperplastic response of liver tissue to arterial malformation, and not a true tumor. When conducting radiation diagnostics, the central scar is determined in 44% of cases. The central scar with T2-weighted MRI is hyperintensive [4]. It is possible to determine the filling of blood formation from the center to the periphery, which distinguishes it from monofocal liver hemangiomas. As a rule, in the case of PF, the risk of complications is low; there is no risk of malignancy. Therefore, a patient with VNF rarely requires their surgical removal. The most common indication for removal is pain, which usually occurs with FNH greater than 7 cm in distance [5]. The presence of more than five nodes are characterized as multiple FNH. This is very rare and only a few cases are described in the literature [6]. With progressive multiple FNH, we did not find any treatment recommendations in the literature other than liver transplantation. Therefore, we decided to present a case of treating multiple liver FNHs in a patient using Sirolimus therapy. We also did not find such articles in the literature and therefore we bring this case to the public.
Materials and Methods
Patient E. 08.03.2001 year of birth. Born from the first
pregnancy, proceeding against the background of chronic
intrauterine hypoxia of the fetus. Childbirth - emergency cesarean
section. Height at birth 51 cm, weight 3118 grams, Apgar score of 8
points. In the neonatal period: pneumonia, urinary tract infection,
perinatal hypoxic encephalopathy of the fetus, intraventricular
hemorrhage. Grew and developed according to age.
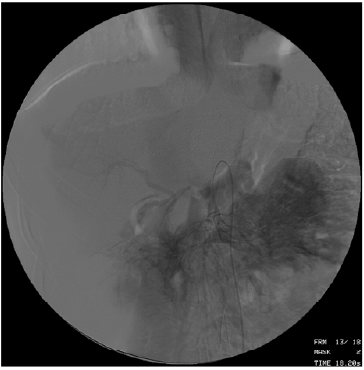
In August 2008, he suffered bleeding from the dilated veins of
the esophagus and stomach. Bleeding is stopped conservatively.
The diagnosis of portal hypertension syndrome, cavernous portal
vein transformation. In October 2008, surgical treatment was
carried out: the formation of spleno-renal anastomosis “side-byside”
(Figure 1). No more bleeding was noted.
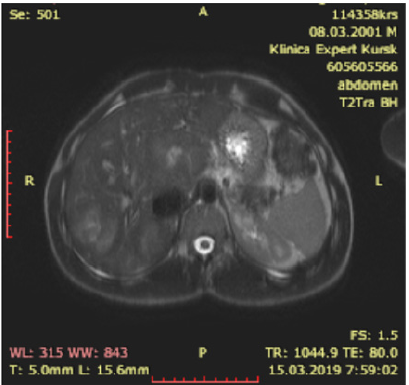
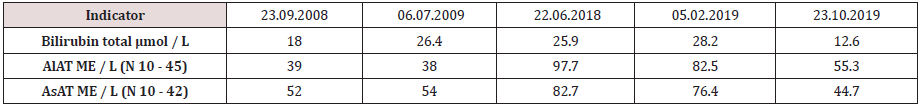
In February 2018, during a control study, multiple FNHs were identified in C1, C4, C8 with dimensions of 87x61 mm, in C7 with dimensions of 51 by 43 mm, 50 by 40 mm (Figure 2). Diagnosed with multifocal bilobar nodular liver hyperplasia after splenorenal bypass surgery for portal hypertension. Blood test for alphafetoprotein 1.66 IU / ml. During the control examination in July 2018, an increase in FNH sizes to 90 by 70 mm, an increase in blood transaminases (Table 1), alkaline phosphatase up to 218.00 IU / L (N 42 - 110), a moderate increase in bilirubin were noted. The patient complained of chronic fatigue, weakness, moderate pain in the liver. lack of appetite.
After examining the child, we came to the conclusion that the observed progression of the disease can lead to the replacement of the liver parenchyma with the subsequent occurrence of organ failure. This could endanger the patient’s life, but there is no possibility of surgery due to the prevalence of the lesion. Sirolimus (Pfizer, USA) from 06.02.2018 was prescribed orally daily at a dose of 3 mg / day until a therapeutic concentration of the drug in blood serum of 6-15 ng / ml was achieved. Due to the excess of the therapeutic interval, the dose of Sirolimus was consistently reduced from 11/06/2018 to 1 mg / day, 02/05/2019 the concentration of Sirolimus was 7.8 ng / ml.
Résultats
As a result of the treatment with Sirolimus, a normalization of the level of liver enzymes, bilirubin in the blood is noted. According to radiation methods, a reduction in liver size and FNH size is up to 30%. Now the patient is feeling well. There is no pain in the liver. Playing sports. Reception of sirolimus continues to date.
Discussion
Multifocal FNH is a rare form of this disease. An even rarer situation arose in our patient, there was a progression of the disease with signs of emerging hepatic cell failure. There was a high risk of severe disease with subsequent liver transplantation. There is an interesting fact that the physiological characteristics of the patient appeared after application of a splenorenal shunt for portal hypertension. Apparently, in the growth stimulation of the nodes, the FNH played the role of impaired portal blood flow. In the available literature, we found only recommendations for liver transplantation in such patients. Teaching ability of Sirolimus to suppress vascular growth through inhibition of M-TOP, we suggested the possible effectiveness of this therapy. After an explanation with the patient and his legal representatives, we started therapy with Sirolimus at a dose of 3 mg / day, then we reduced it to 1 mg / day taking into account the concentration in the blood. The patient had no complications associated with Sirolimus therapy. After a year of treatment, we noted a clear positive trend. The patient’s condition improved, there was no pain, blood counts returned to normal (Table 1).
Conclusion
Of course, this question still requires research in other patients with multiple progressive FNH, in order to draw conclusions about the effectiveness and safety of Sirolimus. But with this patient, we got encouraging results.
References
- Nagorney DM (1995) Benign hepatic tumors: Focal nodular hyperplasia and hepatocellular adenoma. World J Surg 19:13-18.
- Edmondson HA (1958) Tumors of the liver and intrahepatic bile ducts. In: Atlas of tumor pathology. Washington, DC: Armed Forces Institute of Pathology.
- Benhamou JP, Erlinger S (1995) Maladies du Foie et des Voies Biliares, 3rd ed. Paris: Medicines-Sciences: Flammarion.
- Brancatelli G, Federle MP, Grazioli L, Blachar A, Peterson MS, etal. (2001) Focal nodular hyperplasia: CT findings with emphasis on multiphasic helical CT in 78 patients. Radiology 219(1): 61-68.
- Yun Shin Chun, Michael G House, Harmeet Kaur, etal. (2013) SSAT/AHPBA Joint Symposium on Evaluation and Treatment of Benign Liver Lesions. J Gastrointest Surg. 17(4): 636-644.
- Colle I, de Beeck BO, Hoorens A, Hautekeete M (1998) Multiple focal nodular hyperplasia. J Gastroenterol 33 (6): 904-908.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...