
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-5910
Research Article(ISSN: 2638-5910) 
Disparities in Oral Health Utilization and Outcomes in Diabetics in the United States Volume 3 - Issue 5
Hoda M Abdellatif 1,2*
- 1Community Division, Department of Preventive Dental Sciences, College of Dentistry, Princess Nourah bint Abdulrahman University, Saudi Arabia
- 2Public Health Sciences, Texas A&M University College of Dentistry, Dallas, Texas, United States of America
Received:December 23, 2021; Published:January 20, 2022
Corresponding author:Dr. Hoda M Abdellatif, Princess Nourah Bint Abdulrahman University, PO Box 84428, Riyadh, Saudi Arabia
DOI: 10.32474/ADO.2022.03.000175
Abstract
Introduction: As the relationship between periodontitis and type 2 diabetes (T2D) is bidirectional, oral hygiene and compliance with regular dental visits are especially important for wellness in T2D patients. The United States (US) has been identified as a high-income country with significant barriers to accessing healthcare due to cost issues and the necessity of enrolling in a health insurance plan, but level of dental visit compliance and oral health outcomes among diagnosed T2D patients in the US are unknown. The purpose of this analysis was to estimate the number of diagnosed diabetes patients in the US facing unmet need for oral health services and suffering from poor oral health outcomes.
Materials and Methods: Data from the Behavioral Risk Factor Surveillance System (BRFSS), a nationally representative health survey in the US, were used to estimate frequencies of the general population and of diagnosed T2D patients in the US who lacked a health insurance plan, could not access care in the previous twelve months due to cost, had a most recent dental visit of longer than one year before the survey, and had lost six or more teeth at the time of the survey.
Results: Approximately 370,000 diagnosed T2D patients were estimated to have been in the US in 2020. While only about 24,000 lacked health insurance and about 41,000 experienced cost barriers, over one third had a most recent dental visit of longer than a year before the survey, and over one fourth had lost six or more teeth.
Discussion: While T2D patients in the US faced lower barriers to accessing health insurance and healthcare, over a third were out of compliance with preventive dental care, and over one fourth were experiencing severe dental outcomes. These results highlight the necessity to expand oral healthcare access to older patients, especially those with T2D, which could happen through an expansion of public insurance plans to cover oral healthcare as well.
Introduction
The prevalence of type 2 diabetes (T2D) has been increasing globally, and with it, the burden of suffering (Khan et al., 2020). Using the Global Burden of Disease (GBD) database, researchers estimated that the 2017 prevalence of T2D in the United States (US) was close to 9%, with the burden of suffering estimated at 1,046 disability-adjusted life years (DALYs) per 100,000 [1]. These estimates were similar to the rates seen in the same study in European countries such as Germany and the United Kingdom (UK) [1].
Access to care is especially important for T2D patients, who face high risks of disability if their condition remains undiagnosed and/or uncontrolled [2]. The US is different from European countries in an important way, in that that there are significant barriers to accessing healthcare in the US compared to European countries as well as Canada. In a 2021 comparison of eleven highincome countries, researchers at the Commonwealth Fund ranked the US last in access to care [3]. In the US, it has been observed by many researchers that those diagnosed with T2D face high risk of disability due to barriers to accessing care, such as not having health insurance, or having health insurance but still facing cost barriers, and that these barriers are promoters of disability in this group [4-6].
Barriers to accessing care increase complications and subsequent disability in diabetics because their condition progresses more rapidly [6]. It is estimated that 1.8% of the global population has a T2D-related lower-extremity complication [2]. In the US, 40% of women and 25% of men with T2D report a major mobility disability, with a high proportion of those facing barriers to working [5]. T2D patients also face risks of blindness due to diabetic retinopathy, and optimally, should regularly undergo preventive screening [7]. Unfortunately, due to barriers accessing care in the US, a non-trivial proportion of diabetics go undiagnosed, making them at even higher risk for disability resulting from uncontrolled T2D [4].
Many articles discussing disability in diabetics neglect to highlight the impact of barriers to accessing dental care, and the importance of maintaining oral health in this patient group [4,5,8- 10]. It has been established that T2D and periodontitis, or “gum disease”, have a bidirectional relationship, in that they are both a cause and result of each other [8]. Because control of periodontitis also positively impacts control of T2D, good oral hygiene and regular dental visits (at least once per year) are recommended to preserve oral health and prevent tooth loss [9,11]. Yet, one systematic review showed that T2D patients in general have limited oral health knowledge and poor oral health behaviors, and another showed that as quality-of-life (QoL) declined in T2D patients, so did oral health-related QoL (OHRQoL) [11,12].
Further, in the US, a primary obstacle to accessing healthcare exists through needing to enroll in a health insurance plan [13,14]. Medicare is a federally-administered public insurance plan that covers US residents aged 65 and older, and Medicaid is a stateadministered (but federally-supported) health insurance plan that covers indigent adults and children [15]. While virtually all US adults aged 65 and over are enrolled in Medicare, and policy changes have expanded Medicaid to cover a larger proportion of the population, access to dental care still remains elusive in the US, as dental insurance is rarely offered through these programs, and must be purchased independently as a private plan [9,16]. As a result, in the US population in general, there is a low compliance with preventive dental care, and there are significant racialized and socioeconomic disparities in oral healthcare access [9].
The Behavioral Risk Factor Surveillance System (BRFSS) is an annual cross-sectional anonymous phone health survey done by the US government (United States Centers for Disease Control and Prevention, 2021b) [17]. Because the BRFSS uses multi-stage representative sampling of the national US population, data from the BRFSS are routinely used to quantify unmet need and access to care barriers at the population [18,19]. The aim of this analysis was to estimate the frequency of patients diagnosed with T2D in the US facing unmet need for oral health services and suffering from poor oral health outcomes.
Materials and Methods
This study represents a weighted, cross-sectional analysis of the BRFSS 2020 dataset (United States Centers for Disease Control and Prevention, 2021b) [17].
Participants and Setting
The BRFSS 2020 dataset consists of 401,958 records, each with a set of weighting variables to facilitate estimates of absolute frequencies of individuals in the US nationally (United States Centers for Disease Control and Prevention, 2021b) [17]. To develop national estimates, all records were used in this analysis.
Variables Seven variables of interest were selected:
Two demographic variables, two variables measuring barriers to access to care, two variables associated with oral health, and a variable associated with diagnosed T2D status. (No variables referring specifically to access to dental insurance were asked in the 2020 core questions of the BRFSS.)
The two demographic variables were sex (SEXVAR, categorized into binary “female” and “male” categories), and age group (_AGE_G, six categories, including adults age 18 to a maximum coded age of 90). The two variables measuring access to care barriers included the answer of “no” to the question, “Do you have any kind of health care coverage, including health insurance, prepaid plans such as HMOs, or government plans such as Medicare, or Indian Health Service?” (variable HLTHPLN1), and the answer of “yes” to the question, “Was there a time in the past 12 months when you needed to see a doctor but could not because of cost?” (variable MEDCOST), as these variables have been used in other analyses to represent barriers to access to care [13, 19,20].
The two variables associated with oral health were one oral health access variable (answering that the last dental visit was more than 12 months ago to the question, “Including all types of dentists, such as orthodontists, oral surgeons, and all other dental specialists, as well as dental hygienists, how long has it been since you last visited a dentist or a dental clinic for any reason?”, variable LASTDEN4), and one oral health outcomes variable (answering “six or more” or “all” to the question, “Not including teeth lost for injury or orthodontics, how many of your permanent teeth have been removed because of tooth decay or gum disease?”, variable RMVTETH4). T2D diagnostic status was determined through the answer of “yes” to the question, “Has a doctor, nurse, or other health professional ever told you that you had any of the following? (Ever told) you had diabetes?” (variable DIABETE4).
Analytic Approach
First, the analytic dataset was prepared using R software [21]. Next, the analytic file was uploaded to SAS OnDemand for Academics (ODA) where it was analyzed using PROC SURVEYFREQ as recommended by BRFSS (SAS OnDemand for Academics, n.d.; United States Centers for Disease Control and Prevention, 2021a) [22,23]. Weighted population percentage estimates with 95% confidence intervals (CI) were calculated for the variables for the entire US population, and for diagnosed diabetics specifically. These percentages were applied to the population census total to estimate absolute frequencies. The total population estimate from the US census in 2020 is 331,449,281 (United States Census Bureau, n.d.) [24].
Results
The 401,958 records in the BRFSS 2020 dataset represented an unweighted frequency of approximately 260 million US residents (Table 1). In terms of representativeness of the US population in the BRFSS, females were slightly overrepresented (51.29% vs males 48.71%), as were individuals aged 65 and older at 21.92% compared to the other age groups, which included less than 18% in each. In terms of access to care, the analysis estimated that 12.31% of the US population was not on a health insurance plan in 2020, and 10.61% were not able to access care in the 12 months prior to the survey due to cost barriers. In terms of oral health, the analysis estimated that over a third of the US population (34.81%) reported a most recent dental visit of longer than 12 months ago, and over 10% (13.28%) had lost six or more teeth.
Also in Table 1 are estimates specific to patients diagnosed with T2D in the US. As can be seen in Figure 1, which provides a chart of the estimated percentages, T2D patients make up a relatively small percentage of the US population without health insurance (< 1% compared to 12% non-diabetics) and not able to access care due to cost (1% vs. 9% non-diabetics). On the other hand, approximately one seventh of the US population with a most recent dental visit of longer than 12 months ago are diabetic (5% diabetics vs. 30% nondiabetics), and over a fourth of the US population having lost six or more teeth are diabetic (3% diabetics vs. 10% non-diabetics).
Table 1: Estimated Frequencies and Percentages of Individuals in the United States (US) Reporting Barriers to Accessing Medical and Oral Healthcare by Diabetes Status. Although there are challenges overall with access to medical care in the US, only an estimated 41,000 diagnosed diabetics in the US go without health insurance. Of the estimated 35% of the US population with a most recent dental visit longer than one year ago, diabetics make up almost 5%, and of the estimated 13% of the US population that has lost six or more teeth, diabetics make up almost 4%.
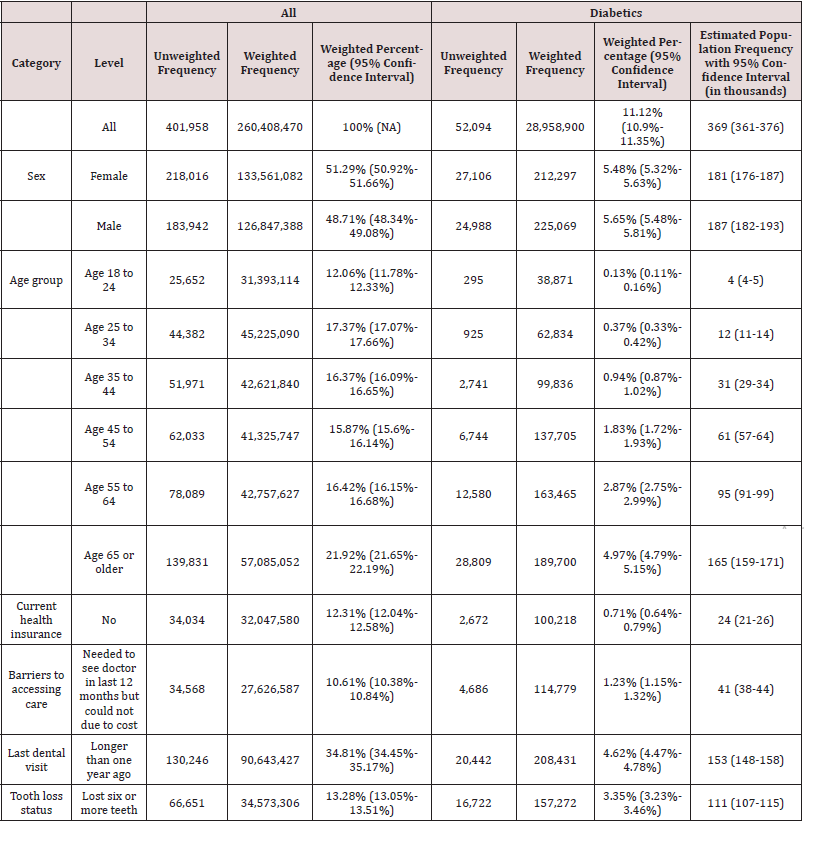
Figure 1: Estimated Percentages of United States (US) Population with Barriers to Accessing Medical and Oral Healthcare and Oral Health Outcomes: Diagnosed Diabetics vs. Non-diabetics. The figure shows how while diagnosed diabetes patients make up a relatively small percentage of the US population reporting not being on a current health insurance plan or not being able to see the doctor because of cost in the past 12 months, they make up a relatively larger percentage of the US population that reports a most recent dental visit of longer than 12 months ago, and having lost six or more teeth.

Figure 2: Estimated Frequency of Diabetics in the United States (US) with Barriers to Accessing Medical and Oral Healthcare. Estimates based on the 2020 US population and weighted percentages from Table 1 are graphed (along with 95% confidence intervals). Approximately 370,000 individuals are estimated to have been diagnosed with diabetes in the US. Among this group, the most prevalent barrier to care was seen with oral healthcare, in that at least 150,000 US diabetics are estimated to have not had a dental visit in the past 12 months, and over 100,000 have been estimated to have lost six or more teeth.
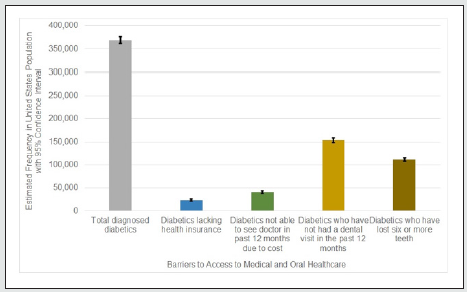
As shown in Table 1, when weighted percentages were applied to the US population in 2020, the frequency of diagnosed diabetics in the US was estimated to be almost 370,000 (Figure 2). While there were an estimated 181,000 female diagnosed diabetics compared to 187,000 males in the US in 2020, over one third (165,000) fell in the age category 65 years and over. While only about 24,000 of these patients lacked health insurance, and only 41,000 had barriers accessing care in the past 12 months due to cost, over one third (153,000) are estimated to have had a most recent dental visit of longer than one year before taking the survey, and over one fourth (111,000) are estimated to have lost six or more teeth at the time of the survey.
Discussion
This analysis estimated that in 2020, the approximately 370,000 diagnosed T2D patients in the US were suffering from disproportionate access to care barriers with respect to oral health, in that while most had health plan coverage and did not face cost barriers in accessing medical care, over one third were not up-todate on preventive dental visits, and over one fourth had lost six or more teeth. Diabetics in the US often find themselves in the same groups experiencing disparities in access to oral healthcare: lowincome, older age, uninsured, or members of a racialized minority or rural population [9,10]. The findings in this analysis are consistent with research that suggests that if dental benefits are simply added to public insurance in the US, dental visit compliance improves and patients experience fewer access barriers to oral [9, 16].
The results of this analysis highlight the necessity of considering oral healthcare as a requirement in order to maintain wellness in diabetics [12, 8]. While this study estimated that over a third of US diagnosed diabetics are aged 65 and older and therefore likely on Medicare, it also showed that diabetics make up a disproportionate number of those going without dental care and experiencing severe tooth loss. Simply extending dental benefits to diabetics on Medicare would likely greatly improve these oral health numbers, as it would likely increase the proportion of US diabetics engaging in preventive oral health behaviors [12,9]. If that were to happen, due to the bidirectional influence between oral health and overall health in diabetics, the rate of diagnosed diabetics in the US where the condition in controlled would likely increase [8].
Although the BRFSS is a dataset representative of the US population, which represents a strength, there are important limitations to this analysis. First, due to the wording of the survey questions, this analysis could only focus on diagnosed diabetics, thus biasing the analysis toward those who already have lowered barriers to accessing care. Second, barriers to access to oral healthcare were approximated through measures of visit compliance and tooth loss outcomes; a more accurate measurement would have been available if the BRFSS had asked a direct question about dental insurance coverage. Finally, it is not clear what the absolute impact would be of expanding dental coverage to all diabetics in the US, as dental care can also be costly in the US, so insurance access may not remove all barriers [10].
In conclusion, this analysis estimated that of the approximately 370,000 diagnosed diabetics in the US in 2020, over one third were out of compliance with preventive dental visits, and over one fourth had lost six or more teeth. As diabetics are at higher risk for poor oral health outcomes, and regular oral hygiene is an important part of bringing diabetes under control, these results highlight the necessity of expanding access to oral healthcare to diabetics in the US population in order to ensure their overall wellness, and to reduce their risk of disability as they age.
Acknowledgements
The author would like to thank Monika Wahi for her scientific advice on this manuscript.
References
- Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, et al. (2020) Epidemiology of Type 2 Diabetes-Global Burden of Disease and Forecasted Trends. Journal of Epidemiology and Global Health 10(1): 107-111.
- Zhang Y, Lazzarini PA, McPhail SM, van Netten JJ, Armstrong DG, et al. (2020) Global Disability Burdens of Diabetes-Related Lower-Extremity Complications in 1990 and 2016. Diabetes Care 43(5): 964-974.
- Schneider EC, Shah A, Doty MM, Tikkanen R, Fields K, et al. (2021) Mirror, mirror 2021: Reflecting poorly. Commonwealth Fund.
- Cowie CC (2019) Diabetes Diagnosis and Control: Missed Opportunities to Improve Health. Diabetes Care 42(6): 994-1004.
- Gregg EW, Menke A (2018) Diabetes and Disability. Diabetes in America (3rd), National Institute of Diabetes and Digestive and Kidney Diseases (US).
- Hill Briggs F, Adler NE, Berkowitz SA, Chin MH, Gary Webb TL, et al. (2020) Social Determinants of Health and Diabetes: A Scientific Review. Diabetes Care 44(1): 258-279.
- Piyasena MMPN, Murthy GVS, Yip JLY, Gilbert C, Zuurmond M, et al. (2019) Systematic review on barriers and enablers for access to diabetic retinopathy screening services in different income settings. PLoS One 14(4): e0198979.
- Kane SF (2017) The effects of oral health on systemic health. General Dentistry 65(6): 30-34.
- Northridge ME, Kumar A, Kaur R (2020) Disparities in access to oral health care. Annual Review of Public Health 41: 513-535.
- Vujicic M (2018) Our dental care system is stuck: And here is what to do about it. Journal of the American Dental Association 149(3): 167-169.
- Poudel P, Griffiths R, Wong VW, Arora A, Flack JR, et al. (2018) Oral health knowledge, attitudes and care practices of people with diabetes: A systematic review. BMC Public Health 18(1): 577.
- Cervino G, Terranova A, Briguglio F, De Stefano R, Famà F, et al. (2019). Diabetes: Oral Health Related Quality of Life and Oral Alterations. BioMed Research International, 2019, 5907195.
- Griffith K, Evans L, Bor J (2017) The Affordable Care Act reduced socioeconomic disparities in health care access. Health Affairs, 10.1377/hlthaff.2017.0083.
- Woolhandler S, Himmelstein DU (2017) The relationship of health insurance and mortality: Is lack of insurance deadly?. Annals of Internal Medicine 167(6): 424-431.
- Wray CM, Khare M, Keyhani S (2021) Access to care, cost of care, and satisfaction with care among adults with private and public health insurance in the US. JAMA Network Open 4(6): e2110275.
- Singhal A, Damiano P, Sabik L (2017) Medicaid adult dental benefits increase use of dental care, but impact of expansion on dental services use was mixed. Health Affairs 36(4): 723-732.
- United States Centers for Disease Control and Prevention (2021b) 2020 BRFSS survey data and documentation.
- Baccaglini L, Kusi Appiah A, Ray M, Yu F (2021) US adults with diabetes mellitus: Variability in oral healthcare utilization. PLoS One 16(5): e0251120.
- Daher M, Al Rifai M, Kherallah RY, Rodriguez F, Mahtta D, et al. (2021) Gender disparities in difficulty accessing healthcare and cost-related medication non-adherence: The CDC behavioral risk factor surveillance system (BRFSS) survey. Preventive Medicine 153: 106779.
- Lutfiyya MN, Gross AJ, Soffe B, Lipsky MS (2019) Dental care utilization: Examining the associations between health services deficits and not having a dental visit in past 12 months. BMC Public Health 19(1): 265.
- R Core Team (2021) R: A language and environment for statistical computing. R Foundation for Statistical Computing.
- (2021) SAS OnDemand for Academics.
- United States Centers for Disease Control and Prevention (2021a) Complex sampling weights and preparing 2020 BRFSS module data for analysis.
- (2021) United States Census Bureau. (n.d.). Census.gov.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




